Savita S. Nadgouda1, Pratap N Mukhopadhyaya2#, Arpan Acharya2, Anju Nagee3 and Prashant D Kunjadia4
1Jaypriya Hospital, 2, Ashoknagar Road, Bailappanavar Nagar, Hubli 580 029, Karnataka, India
2Molecular Genetics Division, geneOmbio Technologies, Krishna Chambers 4th floor, Pashan-Sus Road, Pashan, Pune-411021, Maharashtra, INDIA;
3Ashok & Rita Patel Institute of Integrated Study and Research in Biotechnology and Allied Sciences, New Vallabh Vidyanagar, Anand-388021
4MB Patel Science College, Anand-388001, India
- Corresponding Author:
- Dr. Pratap Narayan Mukhopadhyaya
CEO & Head, R&D Operations geneOmbio Technologies
Krishna Chambers, 4th Floor, Pashan-Sus Road
Pashan, Pune-411 021, Maharashtra, INDIA
Cell phone: +91 9881153425
Fax: +91 20 25871154
E-mail: pnm6619@gmail.com
Introduction
In developing countries like India Genital tract tuberculosis is identified as an important cause of infertility. Most often, hysterosalpingograms (HSG) remain the primary method of diagnosis for understanding various tubal and peritoneal factors that might lead to cases of infertility (Karasick, 1991). This method has been identified as a unique procedure for ascertaining the internal architecture of female genital tract which is essential for ascertaining the changes associated with tuberculosis infection (Schwimmer, 1990).
It has been found that around 0.75% to 1% of total gynecological complaints are associated with genital tuberculosis in India although this number varies from place to place (Arora and Arora (1992). Around 5% of all pelvic infections are cases of genital tuberculosis and further it accounts for 10% of all cases of pulmonary tuberculosis also (Arora and Arora (1992; Dawn, 1998). Althoguh most of the cases are from females of reproductive ages only, it has also bene reported in post menopausal individuals also (Alenti and Pierandrei, 1998).
Infertility is defined as the inability to conceive by at least one year of unprotected intercourse. Treatment may be started earlier in case of an obvious cause or advanced age of the couple. Genital tuberculosis is an important cause of sub fertility, more so in endemic zones such as South India. Still, the true epidemiology of this disease remains unknown due to lack of highly sensitive and specific tests. Genital tuberculosis not only causes tubal obstruction and dysfunction but also impairs implantation due to endometrial involvement and ovulatory failure from ovarian involvement (Roy and Roy, 2003).
The prevalence of infertility is about 10-20% among couples (with somewhat equal prevalence among men and women). There are many factors that can affect female fertility. Some, such as tubal or age factor, are completely known and some are in debate (e.g. endometriosis, cervical or immunologic factors (Xiang et al., 1998).
Female genital tuberculosis (FGTB) is still a major cause of infertility in India in spite of the availability of specific therapy. The prevalence of FGTB in infertility clinics shows marked variations in different countries ranging between 15 and 25% (Xiang et al., 1998). In 80-90% of cases, FGTB affects young women between 18 and 38 years of age and is an important cause of infertility (Varma, 1991; Crofton et al., 1992). Genital tuberculosis (TB) predominantly affects individuals below 40 years of age and peak age frequency ranges between 21 to 30 year of age (Nwachokor and Thomas, 2000).
In this study, the prevalence of genital tuberculosis in a cross section of female population in India was surveyed with special reference to incidences of infertility.
Materials and Methods
Study population
The resource population for this study comprised of 170 female individuals, aged between 25-40 years visiting the clinic with complaints that were within the purview of inclusion criteria. The parameters for selection were complaining of infertility and symptoms of pelvic pain, irregular menstrual bleeding, scanty menstruation or amenorrhea. A pelvic mass in variable combination was also considered to be criteria for inclusion of a subject for study. Constitutional symptoms comprised of sweating and weight loss. Local organ dysfunction manifested in amenorrhea, and bilateral tubal blockage was also noted as seen through classical hysterosalpingographic study.
Analytical methods
The analytical assays performed under this study were as described by cited authors. (1) Conventional culture method (Nyendak et al., 2009) (2) Polymerase Chain Reaction (PCR) for Mycobacterium complex (Beige et al., 1995) (3) hysterosalpingographic study (HSG) (Chavan et al., 2004) (4) tissue histopathology (Lucas, 1988) and ultrasonography (Yapar et al., 1995).
Results and Discussion
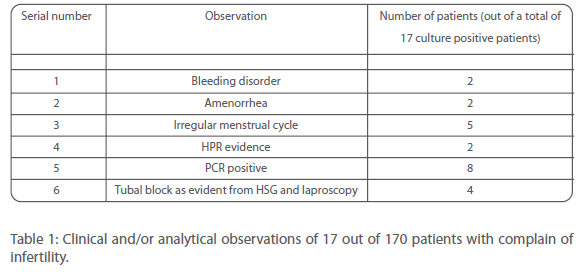
170 patients were analyzed in this study. Out of these 17 were found to be positive for Mycobacterium tuberculosis infection by culture method (Table 1). All these patients indicated bad obstetric history with ultrasonography finding confirming an altered endometrium associated with genital tuberculosis.
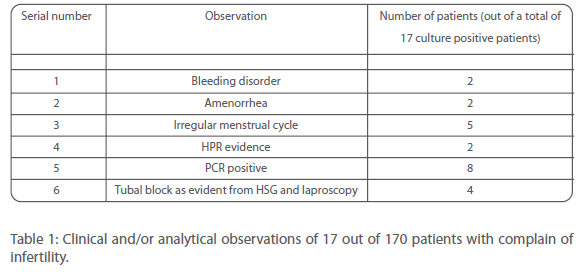
Table 1: Clinical and/or analytical observations of 17 out of 170 patients with complain of infertility.
It was noted that in 50% of genital MTB cases, the endometrium was involved. Further, around 30% of the patients with tubal adhesions, intrauterine adhesion was observed.
All 17 patients were subjected to treatment regimen that involved the WHO recommended treatment scheme (PZA=1500 mg/day + INH (300 mg/day) + Rifampicin (450 mg/day) + Ethambutol (800 mg/day) for 4 months and Rifampicin + INH = 450:300 for another 5 months respectively (World Health Organization, 2003. Treatment of Tuberculosis: Guidelines for National Programmes). Out of them, 3 patients discontinued medication because of side effects (jaundice, skin rash and acid peptic diseases) and/or non compliance of therapy.
Post treatment, all these patients were the subjected to standard in vitro fertilization (IVF) treatment. Around 5 of them were cured of menstrual problems and ascites while 2 patients successfully conceived. It was noted that the conception rate was low and further the birth rate was still lower. The risk factors not conducive to pregnancy were secondary amenorrhea, any endometrium or curettage and negative chromopertubation.
There has been a rapid surge in female genital TB and therefore gynecologists will be face increased cases of TB infection. Genital tuberculosis can be asymptomatic or may present atypical symptoms or even mimic other clinical conditions that make the situation all the more challenging. Therefore it is necessary that we consider the possibility of TB in patients within the reproductive age group who present with symptoms of infertility, chronic pelvic pain and menstrual dysfunction where other causes have been ruled out. This if further important for those women who fall unto the high risk category for TB infection.
This study highlights the fact that tuberculosis, a chronic infectious disease is one of the major etiological factors of female tubal infertil- ity especially on the Indian subcontinent. In women with genital tuberculosis, the clinical pregnancy rate per cycle is lower and further, spontaneous abortion rate is high. Therefore they appear to represent a less favorable subset within other tubal factor-patients when treated with IVF-ET.
364
References
- Schwimmer M. Gynecological inflammatory diseases. In: Pollack HM, editor. Clinical urography (1st edn) Philadelphia: W.B. Saunders, 1990: 985.
- Arora R.. Rajaram P., Oumachigui A., Arora V.K.; Prospective analysis of short course chemotherapy in female genital tuberculosis; Int J Gynecol Obstel 1992;38:311
- Dawn C.S.; Pelvic infections; In: Dawn C.S.; ed Textbook of Gynaecology and Contraception: 9th ed.; Calcutta: Arati Dawn; 1998; 321
- Alenti C., Pierandrei G.; Postmenopausal endometrial tuberculosis. A clinical case; Minerva Ginecol 1998; 50: 93
- Roy H, Roy S. Use of polymerase chain reaction for diagnosis of endometrial tuberculosis in high risk subfertile women in an endemic zone. J Obstet Gynecol India 2003;53:260
- Xiang W, Liao, ACR and Chan, C. A new molecular variant of Luteinizing Hormone associated with female infertility. Fertil Steril 1998; 69: 102
- Varma TR. Genital tuberculosis and subsequent fertility. Int J Gynaecol Obstet 1991;35:1.
- Crofton J, Horne N, Miller F. Clinical tuberculosis. 1st edn. London: Macmillan Education Ltd. 1992;502-10.
- Nwachokor FN, Thomas JO. Tuberculosis in Ibadan, Nigeria – a 30 year review. Cent Afr J Med 2000; 46:287
- Chavhan GB, Hira P, Rathod K, Zacharia TT, Chawla A, Badhe P, Parmar H. Female genital tuberculosis: hysterosalpingographic appearances. Br J Radiol. 2004;77:164.
- Beige J, Lokies J, Schaberg T, Finckh U, Fischer M, Mauch H, Lode H, Köhler B, and Rolfs A. Clinical evaluation of a Mycobacterium tuberculosis PCR assay. J Clin Microbiol. 1995; 33: 90.
- Lucas SB. Histopathology of leprosy and tuberculosis—an overview. British Medical Bulletin 1988; 44:584
- Yapar EG, Ekici E, Karasahin E and Gokmen O. Sonographic features of tuberculosis peritonitis and female genital tract tuberculosis. Ultrasound Obstet Gynecol. 1995;6: 121-125.
- Nyendak MR, Lewinsohn DA, Lewinsohn DM. New diagnostic methods for tuberculosis. Curr Opin Infect Dis. 2009; 22:174