Keywords
Surgical approach; Cerebral aneurysm; Neurovascular; Ruptured; Surgery
Abbreviations
CSF: Cerebrospinal Fluid; EVD: Extra-Ventricular Drainage; GOS: Glasgow Outcome Scale; H-H: Hunt and Hess Grades; ICH: Intracerebral Hemorrhage; IOR: Intraoperative Aneurysm Rupture; MLSO: Modified Lateral Supraorbital Approach; PCA: Posterior Cerebral Artery; SCA: Superior Cerebellar Artery
Introduction
The pterional approach is one of basic approaches for most cerebral aneurysm operations [1,2]. Recently, several approaches have been developed to secure a spacious and safe operation field with a smaller skin incision and craniotomy bone flap. Up to now, most authors reported the supraorbital approach as a surgical method for unruptured aneurysm and small and less complex aneurysm in the literature. The authors devised the Modified Lateral Supraorbital (MLSO) approach, which is a modification of the supraorbital approach. This study presented a 16 year experience with MLSO approach for ruptured anterior circulation aneurysms and some parts of posterior circulation aneurysms.
Methods
Patients
The 2478 patients had carried out ruptured aneurysm surgery from January 1996 through December 2012. Among them, 323 patients who were operated on using the MLSO approach by one senior neurosurgeon were included. Patients who underwent surgery via a different approach or by a different neurosurgeon were excluded. This retrospective study protocol was approved by the Hospital Institutional Review Board.
Selection of surgical approach
Initially, the MLSO approach was chosen regardless of the size, character, complexity and location of the aneurysm (aneurysms in anterior circulation and some parts of posterior circulation-superior cerebellar artery (SCA), posterior cerebral artery (PCA), basilar artery). After several years’ experience of MLSO approach, most ruptured aneurysms were clipped via MLSO approach except for cases associated with severe brain swelling and with a large amount of intracerebral hemorrhage (ICH). In the cases associated with severe brain swelling and with an ICH over 100 cc, which was judged that a large craniotomy would be necessary for decompression and hemorrhage removal, the pterional approach was chosen.
General guideline for treatment
To reduce the risk of aneurysm rebleeding, in principle, the operation was conducted within 24 hours. Cerebral angiography was carried out in most cases, except for those with severely unstable vital signs before surgery. In cases with severe vascular spasm after the operation and other necessary cases, a follow up angiography was also carried out. Extra-ventricular drainage (EVD) was carried out in patients with hydrocephalus if necessary, and lumbar catheter cerebrospinal fluid (CSF) drainage was carried out selectively to reduce brain swelling during the operation. The period of the EVD was limited to 8 days. For cases needing additional drainage, a new EVD was carried out, while a ventriculo-peritoneal shunt was used for indicated cases. The surgery was performed under general endotracheal anesthesia with continuous neurophysiological monitoring. The patients were treated in the neurosurgery intensive care unit after the operation. To prevent vasospasm after diagnosis of the subarachnoid hemorrhage, nimodipine was administered immediately. For the patients with symptomatic vasospasm, hypertensive hypervolemic treatment and medical treatment were carried out.
Surgical technique: MLSO approach
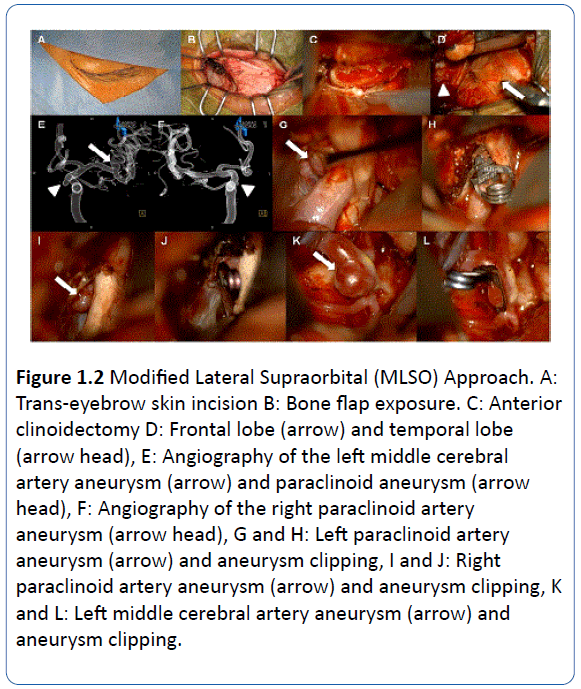
The patient was placed in the supine position with a Mizuho head holder, and the head was elevated above the level of the heart and turned 10°-30° to the contra-lateral side. The skin incision was made on the inferior edge of the eyebrow, starting from 0.5 cm medial to the mid-pupilary line and extending laterally to just behind the frontal process of the zygomatic bone, then extending inferior laterally about 1 cm. To expose the frontal bone and temporalis fascia, subcutaneous dissection was performed carefully, so as not to damage the supraorbital nerve. After making an incision of about 2 cm in the temporal fascia, the temporal muscle was detached from the temporal bone to expose the pterion. Then, the temporal muscle was retracted with privately designed muscle hooks. Unlike other approaches, after placing one burr hole on the frontosphenoid suture, a free bone flap was made with a craniotome, including the supraorbital bone, frontozygomatic process and frontal bone, making an opening of nearly 2.0 cm × 2.5 cm. The orbital roof and lateral wall were fractured with an osteotome, then the temporal bone was removed using a rongeur and punch. If necessary, part of the orbital roof was removed, and the optic canal was unroofed with an anterior clinoidectomy. After clipping of the aneurysm, cranial plates were used to fix the bone flap, and the temporal bone defect area was filled with bone chips (Figure 1).
Variables and Data Sources
Patient's clinical data, such as age, sex, Hunt and Hess (H-H) grades, Fisher grades, aneurysm size, aneurysm locations, associated hemorrhage, operation time, temporary clipping time, procedural complications, mortality, status at discharge, and clinical outcomes at 6 months and 1 year were retrospectively collected through medical records. Aneurysms were divided into single and multiple, according to the number of lesions. The size distribution of the aneurysm was classified into small (<7 mm), medium (7-12 mm), large (>12 mm, <25 mm) and giant (≥ 25 mm). The associated ICH was classified into the following 4 categories: I none; II <50 cc; III 50~100 cc; and IV>100 cc.
The operating time was measured from the time of anesthetic induction to the time of completion of the skin closure. The procedural complications included wound problem, ischemic events that may occur in all courses, intraoperative aneurysm rupture (IOR), postoperative hemorrhage, cranial nerve function abnormality, and CSF leakage during the operation. The clinical outcomes were evaluated using the Glasgow Outcome Scale (GOS), which was classified patients into the following five grades: I: death; II: vegetative state and severely disabled; III: moderately disabled; IV: mildly disabled; V: not disabled.
Statistical Analysis
The statistical analysis was conducted using SPSS vs. 18.0. Continuous variables were presented as means with the range, and categorical variables were presented as frequency. Statistical analysis was conducted with the independent t-test for continuous variables, and the × 2 test for categorical variables. The significant level was set at 0.01 (p=0.01).
Results
Aneurysm clipping surgery using the MLSO approach was performed on 323 patients. The mean age was 52.3 years and the ratio of males to females was 1:1.2.293 patients had single aneurysms and 30 patients had multiple aneurysms. The proportion of small, medium, large, and giant aneurysms were 64%(206/323), 31%(101/323), 4.7%(15/323), and 0.3%(1/323) (Table 1).
| |
No. of patients |
Mean age |
Sex |
No. of aneurysms |
Size of aneurysms |
| Male |
Female |
Single |
Multiple |
Small |
Medium |
Large |
Giant |
| MLSO |
323 |
52.3 |
150 |
173 |
293 |
30 |
206 |
101 |
15 |
1 |
Table 1 Characteristics of subjects and aneurysms.
A direct clip was carried out for most of the aneurysms, while additional wrapping was carried out in 10 cases which had difficulties in clipping, due to fusiform or dissecting aneurysms. A second clipping operation was performed only 1 case (failed clipping due to severe brain swelling, with re-clipping performed after the brain swelling was controlled).
Mild temporal muscle atrophy occurred in only 6 cases (1.8%), but fat graft for temporal muscle atrophy was not needed.
Single aneurysm
Most of the aneurysm lesions were located in anterior cerebral artery (ACA) (Table 2). Mean H-H and Fisher grades were 2.54 and 2.61. Hydrocephalus was noted in 24% (70/293). Infarction occurred at a rate of 9% (27/293). ICH was developed in 12% (35/293), showing small (11%), medium (1%), and large (0%) (Table 3). Mean operation time was 215 minutes. For the first eight years, the mean operation time was 234.4 minutes, while that of the later eight years was 207.9 minutes. The temporary clipping time was 412 seconds (Table 3).
| No. of aneurysms |
Location |
No. of aneurysms |
| Single |
ACA |
110 |
| MCA |
77 |
| ICA distal |
93 |
| ICA proximal |
11 |
| Posterior circulation |
2 |
| Multiple |
Group 1 |
22 |
| Group 2 |
4 |
| Group 3 |
- |
| Group 4 |
3 |
| Group 5 |
1 |
Group 1: unilaterally in the anterior circulation including the anterior communicating artery
Group 2: bilaterally in the anterior circulation
Group 3: all an in the posterior circulation
Group 4: in both anterior and posterior circulation
Group 5: bilaterally in the anterior circulation and posterior circulation
Table 2 Location of aneurysms.
| |
Single aneurysms |
Multiple aneurysms |
| Mean Hunt-Hess grade |
2.54 |
2.67 |
| Fisher grade |
2.61 |
2.83 |
| Hydrocephalus |
70 |
14 |
| Infarction |
27 |
- |
| ICH |
35 |
4 |
| Small |
34 |
3 |
| Medium |
1 |
- |
| Large |
- |
1 |
| Operation time (min) |
215 |
264 |
| Temporary clipping time (sec) |
412 |
477.3 |
*P ≤ 0.01
Table 3 Preoperative evaluations and operative variants.
Procedural complications occurred in 20 cases (7%). There were 4 postoperative hemorrhages, 3 IOR, 3 ischemic events, 3 CSF infections, 2 CSF leakages, 2 wound problems, 1 permanent 3rd nerve palsy, 1 permanent 6th nerve palsy, and 1 lumbar catheter related tonsilar herniation (Table 4).
| |
Single aneurysms |
Multiple aneurysms |
| IOR |
3 |
1 |
| Postoperative hemorrhage |
4 |
- |
| Ischemic events |
3 |
- |
| Aneurysm clip slipping |
- |
- |
| CSF infection |
3 |
- |
| CSF leakage |
2 |
- |
| Wound problem |
2 |
- |
| Permanent 3rd nerve palsy |
1 |
- |
| Permanent 6th nerve palsy |
1 |
- |
| Trigeminal neuralgia |
- |
- |
| Lumbar catheter related tonsilar herniation |
1 |
- |
| Total |
20 |
1 |
Table 4 Procedure associated complications.
Mortality occurred in 6 patients. Of these patients, 5 patients died from severe brain swelling and refusal of additional treatment, while 1 patient died from tonsilar herniation due to lumbar catheter drainage. Excluding those deceased cases, clinical follow-up data was available for 287 patients. Favorable clinical outcomes, GOS IV or V, were observed in 82% (242/293) and 83% (245/293) at 6 months and 1 year follow-up (Table 5).
| |
Single aneurysms |
Multiple aneurysms |
| Mortality Glasgow outcome scale IV or V |
6 |
- |
| 6 months |
242/293(82%) |
25/30(83%) |
| 1 year |
245/293(83%) |
25/30(83%) |
Table 5: Clinical outcomes.
Multiple aneurysm
The lesions were located on various sites of the cerebral vessels, and most patients showed unilateral aneurysms (Table 2).
Mean H-H and Fisher grades were 2.67 and 2.83. Hydrocephalus was observed in 47% (14/30), while no cerebral infarction was observed.
ICH was developed in 13% (4/30), showing small (10%), medium (0%), and large (3%) (Table 3). Mean operation time was 264 minutes. The temporary clipping time was 477.3 seconds (Table 3).
Procedural complication occurred in one case, IOR was occurred (3.3%) (Table 4). There was no mortality. The clinical follow-up was available for 30 patients.
Favorable clinical outcome, GOS IV or V, was the same as 83% (25/30) in the follow-ups performed at 6 months and one year (Table 5).
Discussion
The standard pterional approach is one of the approaches used most commonly for sellar, parasellar, and suparsellar lesions in cerebral vascular and tumor surgery [1,2]. Various approaches, such as the lateral supraorbital approach, supraorbital keyhole surgery, and mini-pterional approach were also developed [3-5]. The most important goals of these surgical approaches are to minimize the brain retraction, to reduce the skin incision line associated cosmetic problems, to obtain a proper small size of bone flap for the operation, and to decrease the atrophy of muscles by reducing the temporal muscle manipulation. In addition, a sufficient operation field should be secured.
The biggest advantages of the supraorbital keyhole surgery, which was described first by Jane and generalized by Perneczky, are the smaller skin incision compared to the pterional approach, minimization of the craniotomy, and reduction of brain retraction [5-7]. However, this approach is more appropriate for cases with smaller aneurysms, or less complex cases than those for the pterional approach [8].
According to Asem Salma, the lateral supraorbital approach used in cadaveric study has the advantage of accessing the optic nerve and A-com complex with less temporal muscle manipulation and a smaller bone flap than the pterional approach.
However, it has the limitation on the sylvian dissection at the level of the limen insulae, so more brain retractions are needed to approach the proximal ICA or basilar artery area [9]. Consequentially, the two approaches have similar surgical exposure in the sellar, suprasellar and the anterior communicating artery space, but the standard pterional approach is considered more appropriate for approaching the retrosellar area.
There are biggest two differences between the MLSO approach and the existing surgical approaches, such as the supraorbital keyhole surgery, lateral supraorbital approach and pterional approach. One is the bone flap including the orbital rim, and the other is the temporal craniotomy from the zygoma suture line (Figures 1.1B and 1.1C).
Including the orbital rim in the bone flap would allow approaching the sellar, parasellar and retrosellar areas from further inferiorly and anteriorly [10-13]. Therefore the MLSO could have the advantage to relatively minimize brain retraction compared to the supraorbital approach, lateral supraorbital approach and pterional approach.
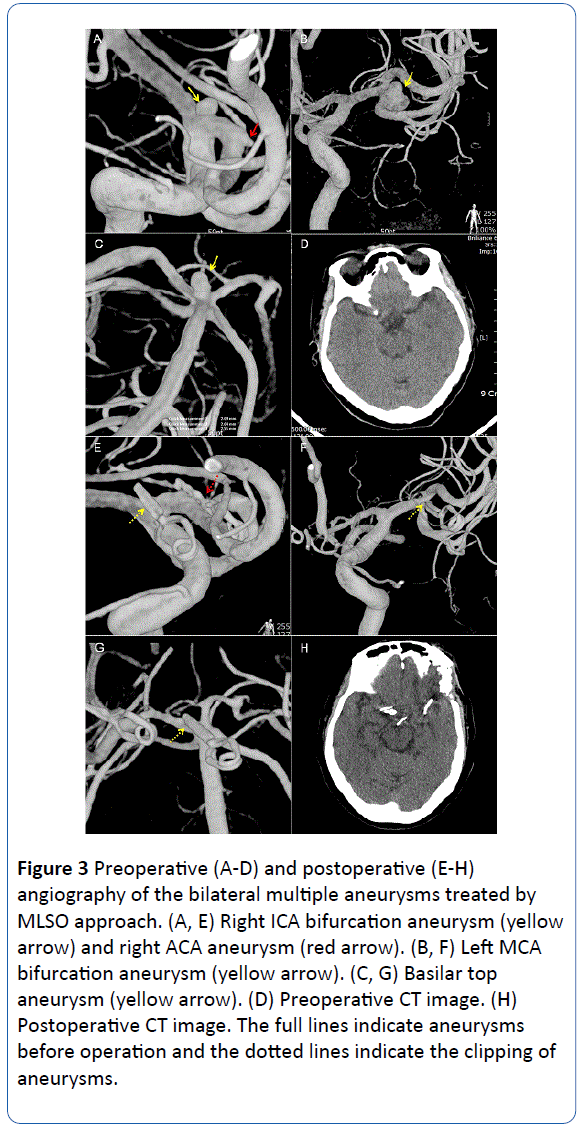
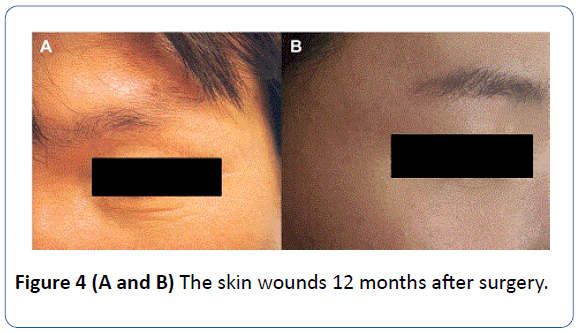
In case of the anterior communicating artery, contra-lateral ICA and proximal ACA segment aneurysms, the MLSO could performed with less brain retraction compared with other approaches, so it can be used for complex aneurysms operation (Figures 1 and 2). In addition, the MLSO approach can also treat aneurysms located in the high basilar artery area, and bilateral aneurysms (Figures 2 and 3). Because the MLSO can perform the temporal craniotomy from the zygoma suture line, the sylvian dissection can be completed and brain retraction can be minimized (Figure 1.1D). It can be assumed that because the supraorbital keyhole surgery don't perform the temporal craniotomy from the zygoma suture line and bone flap including orbital rim, it is proper to mainly small aneurysm and less complex aneurysm [14]. The lateral supraorbital approach also has the problem that more brain retractions are needed for sufficient surgical exposure, due to the incomplete sylvian dissection (Figure 4).
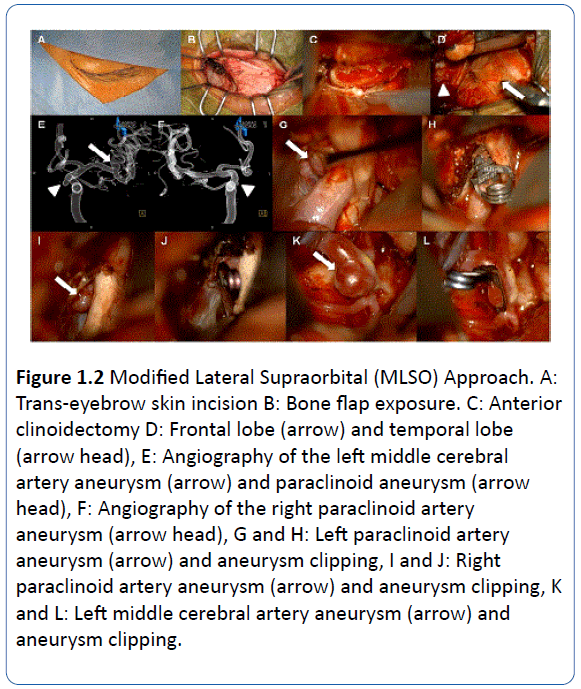
Figure 1.1: Modified Lateral Supraorbital (MLSO) Approach. A: Trans-eyebrow skin incision. B: Craniotomy lines. C: Frontal lobe (F), Temporal lobe (T) and Supraorbital nerve (S). D: Dural incision.
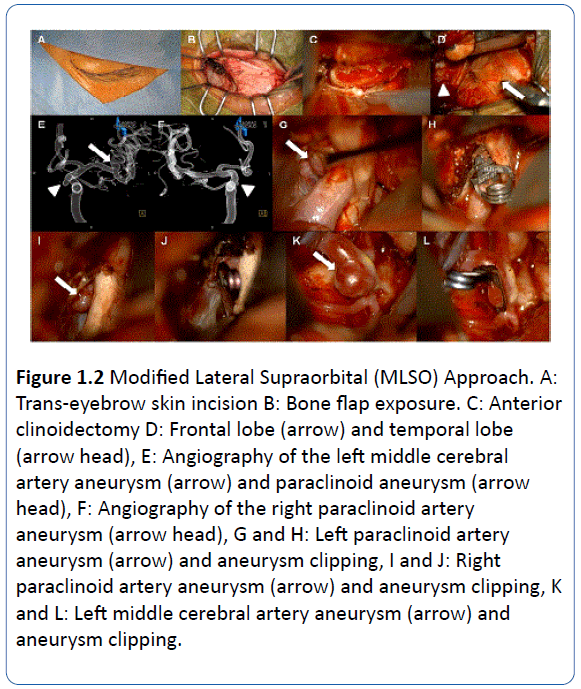
Figure 1.2 Modified Lateral Supraorbital (MLSO) Approach. A: Trans-eyebrow skin incision B: Bone flap exposure. C: Anterior clinoidectomy D: Frontal lobe (arrow) and temporal lobe (arrow head), E: Angiography of the left middle cerebral artery aneurysm (arrow) and paraclinoid aneurysm (arrow head), F: Angiography of the right paraclinoid artery aneurysm (arrow head), G and H: Left paraclinoid artery aneurysm (arrow) and aneurysm clipping, I and J: Right paraclinoid artery aneurysm (arrow) and aneurysm clipping, K and L: Left middle cerebral artery aneurysm (arrow) and aneurysm clipping.
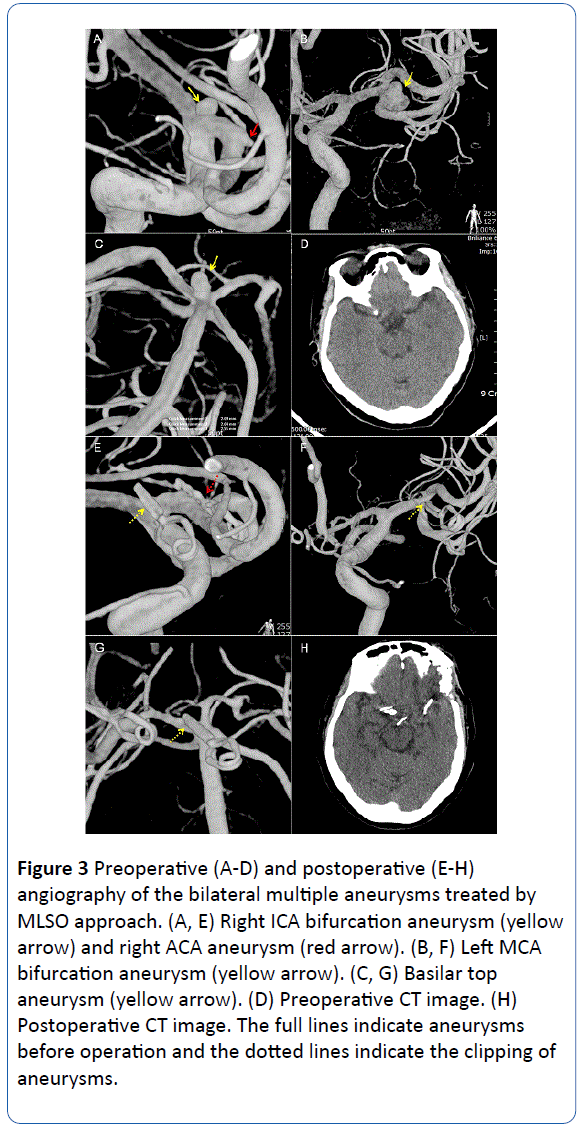
Figure 3 Preoperative (A-D) and postoperative (E-H) angiography of the bilateral multiple aneurysms treated by MLSO approach. (A, E) Right ICA bifurcation aneurysm (yellow arrow) and right ACA aneurysm (red arrow). (B, F) Left MCA bifurcation aneurysm (yellow arrow). (C, G) Basilar top aneurysm (yellow arrow). (D) Preoperative CT image. (H) Postoperative CT image. The full lines indicate aneurysms before operation and the dotted lines indicate the clipping of aneurysms.
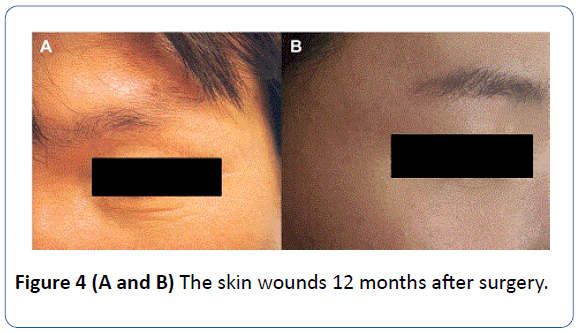
Figure 4 (A and B) The skin wounds 12 months after surgery.
The optic nerve unroofing, the anterior clinoidectomy, and the cavernous sinus manipulation are possible through MLSO approach easily, so brain retraction can be minimized and it can be used in treatment of aneurysms of the proximal ICA (paraclinoid, ophthalmic, cavernous extended) [15]. In the previous studies, the supraorbital keyhole approach demonstrated good outcomes on the aneurysm operation, but the aneurysms treated in that study were less complex, smaller than those in the pterional approach group [8]. In this study, we could treat the more complex and larger size aneurysm through MLSO approach successfully.
The IOR is an important item for evaluating the stability of the approach. In a study analyzing 9488 aneurym surgeries, IOR occurred at a frequency of 10.09% in the pterional group and 5.78% in the suprabrow group, but considering the group of 3039 ruptured aneurysms, it occurred in 13.8% of the pterional group, and 19.37% of the suprabrow group [16]. In a study focusing only on ruptured aneurysms, IOR occurred in the pterional group at 6%-34.9%, and in the suprabrow group at 0-26% [11,17-26]. In an analysis comparing the supraorbital keyhole approach (10.6%) and the pterional approach (2.5%) directly, the supraorbital group showed higher IOR frequency [8]. However, in this study, the frequency of IOR occurrence in ruptured aneurysm (1.2%) was lower than that of other studies.
In the previous studies, complications were reported in 2%-16.9% for the various surgical approaches used for aneurysms. In this study, the frequency of complications observed using the MLSO approach was relatively lower (6.5%) than other reports [8,27,28]. In addition, the incidence of postoperative hemorrhage was very low (1.2%, 4/323). The tonsilar herniation, as one of the fatal complications, due to lumbar catheter CSF over-drainage occurred in 1 case. It was thought that this complication occurred regardless of the surgical approach. Taking these results together, good results were obtained in the aspect of stability for the MLSO approach.
Regarding clinical outcome, favorable clinical outcomes, GOS IV or V, were observed 82% (242/293) and 83%(245/293) at 6 months and one year follow-up in single aneurysm group, 83% (25/30) and 83%(25/30) in multiple aneurysm group.
By making a small skin incision below the eyebrow in MLSO approach (Figure 1.1A), the scar formation and manipulation of the temporalis muscle could be minimized. The injuries of the superficial temporal artery, supraorbital artery, and frontal branch of the facial nerve could be reduced. The small skin incision and less temporal muscle atrophy might provide a good cosmetic effect. In addition, it might help to maintain the biting activity [10,29]. In some cases through pterional and lateral supraorbital approaches, additional rehabilitation was needed due to the difficulties of biting activity. It was not quantified, patients and families had a high level of satisfaction and the good response to the MLSO approach due to these cosmetic and functional benefits.
The limitations of this study are as follows: not being the result of a multicenter trial, small sample size, not being the randomized study, and the selection bias. In the case of severe brain swelling and huge ICH associated aneurysms, the author preferred to select the pterional approach rather than the MLSO approach and it caused the selection bias. This study was based on the cases operated by one surgeon, who used the MLSO and the pterional approach, so it may be difficult to generalize the result. In order to generalize the result, prospective randomized studies of a large series may be needed. In addition, un-ruptured aneurysms were not mentioned in this study, and further studies including un-ruptured aneurysm cases will also be necessary.
In conclusion, the MLSO approach has the following advantages: less brain retraction, good surgical field for high positioned A-com or basilar tip aneurysm surgery, short operation time, small skin incision, minimizing temporal muscle manipulation and good cosmetic outcome. In the cases of general ruptured aneurysms, except for cases associated with a large amount of intracerebral hemorrhage and those associated with severe brain swelling, we suggest that the MLSO approach can be a favorable surgical option for experienced neurosurgeons.
18353
References
- Figueiredo EG, Deshmukh P, Zabramski JM, Preul MC, Crawford NR, et al. (2008) The pterional-transsylvian approach: an analytical study. Neurosurgery 62: 1361-1367.
- Yasargil MG, Antic J, Laciga R, Jain KK, Hodosh RM, et al. (1976) Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol 6: 83-91.
- Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, et al. (2007) The minipterional craniotomy: technical description and anatomic assessment. Neurosurgery 61: 256-264.
- Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, et al. (2005) Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl 94: 17-21.
- Jane JA, Park TS, Pobereskin LH, Winn HR, Butler AB (1982) The supraorbital approach: technical note. Neurosurgery 11: 537-542.
- Reisch R, Perneczky A, Filippi R (2003) Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol 59: 223-227.
- van Lindert E, Perneczky A, Fries G, Pierangeli E (1998) The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol 49: 481-489.
- Chalouhi N, Jabbour P, Ibrahim I (2013) Surgical treatment of ruptured anterior circulation aneurysms: comparison of pterional and supraorbital keyhole approaches. Neurosurgery 72: 437-441.
- Salma A, Alkandari A, Sammet S, Ammirati M (2011) Lateral supraorbital approach vs pterional approach: an anatomic qualitative and quantitative evaluation. Neurosurgery 68: 364-372.
- Dare AO, Landi MK, Lopes DK, Grand W (2001) Eyebrow incision for combined orbital osteotomy and supraorbital minicraniotomy: application to aneurysms of the anterior circulation. Technical note. J Neurosurg 95: 714-718.
- Jeon BC, Chen SY, Zheng YR, Cho YW, Kwon KY (2003) Superior orbital rim approach for anterior communicating artery aneurysms: a surgical series of 27 patients. J Korean Med Sci 18: 566-572.
- Jho HD (1997) Orbital roof craniotomy via an eyebrow incision: a simplified anterior skull base approach. Minim Invasive Neurosurg 40: 91-97.
- Warren WL, Grant GA (2009) Transciliary orbitofrontozygomatic approach to lesions of the anterior cranial fossa. Neurosurgery 64: 324-329.
- Figueiredo EG, Deshmukh V, Nakaji P (2006) An anatomical evaluation of the mini-supraorbital approach and comparison with standard craniotomies. Neurosurgery 59: ONS212-ONS220.
- Lim J, Cho K (2016) The modified lateral supraorbital approach for tumors of the petroclival junction extending into the anterior cerebellopontine area. J neuro oncol 127: 541-550.
- Madhugiri VS, Ambekar S, Pandey P (2013) The pterional and suprabrow approaches for aneurysm surgery: a systematic review of intraoperative rupture rates in 9488 aneurysms. World Neurosurg 80: 836-844.
- Bhatoe HS (2009) Transciliary supraorbital keyhole approach in the management of aneurysms of anterior circulation: Operative nuances. Neurol India 57: 599-606.
- Bulters DO, Santarius T, Chia HL, Parker RA, Trivedi R, et al. (2011) Causes of neurological deficits following clipping of 200 consecutive ruptured aneurysms in patients with good-grade aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien) 153: 295-303.
- Chen L, Tian X, Zhang J, Huang Y, Chen E, et al. (2009) Is eyebrow approach suitable for ruptured anterior circulation aneurysms on early stage: a prospective study at a single institute. Acta Neurochir (Wien) 151: 781-784.
- Cunningham EJ, Debar S, Bell BA (2003) Association between surgeon seniority and outcome in intracranial aneurysm surgery. Br J Neurosurg 17: 124-128.
- Elijovich L, Higashida RT, Lawton MT, Duckwiler G, Giannotta S, et al. (2008) Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: the CARAT study. Stroke 39: 1501-1506.
- Fridriksson S, Säveland H, Jakobsson KE, Edner G, Zygmunt S, et al. (2002) Intraoperative complications in aneurysm surgery: a prospective national study. J Neurosurg 96: 515-522.
- Houkin K, Kuroda S, Takahashi A, Takikawa S, Ishikawa T, et al. (1999) Intra-operative premature rupture of the cerebral aneurysms. Analysis of the causes and management. Acta Neurochir (Wien) 141: 1255-1263.
- Ramos-Zuniga R, Velazquez H, Barajas MA, Lopez R, Sanchez E, et al. (2002) Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery 51: 125-130.
- Sandalcioglu IE, Schoch B, Regel JP, Wanke I, Gasser T, et al. (2004) Does intraoperative aneurysm rupture influence outcome? Analysis of 169 patients. Clin Neurol Neurosurg 106: 88-92.
- Woertgen C, Rothoerl RD, Albert R, Schebesch KM, Ullrich OW (2008) Effects of temporary clipping during aneurysm surgery. Neurol Res 30: 542-546.
- Beseoglu K, Lodes S, Stummer W, Steiger HJ, Hanggi D (2011) The transorbital keyhole approach: early and long-term outcome analysis of approach-related morbidity and cosmetic results. Technical note. J Neurosurg 114: 852-856.
- Fischer G, Stadie A, Reisch R, Hopf NJ, Fries G, et al. (2011) The keyhole concept in aneurysm surgery: results of the past 20 years. Neurosurgery 68: 45-51.
- Paladino J, Mrak G, Miklic P, Jednacak H, Mihaljevic D (2005) The keyhole concept in aneurysm surgery--a comparative study: keyhole versus standard craniotomy. Minim Invasive Neurosurg 48: 251-258.