Aejaz Ul Haq*, Victor H Kha and Kellie R Jones
University of Oklahoma Health Sciences Center, Oklahoma City, USA
- *Corresponding Author:
- Aejaz Ul Haq
University of Oklahoma Health Sciences Center
Oklahoma City, USA
Tel: 14052714000
E-mail: Aejaz-UlHaq@ouhsc.edu
Received date: December 26, 2017; Accepted date: January 10, 2017; Published date: January 17, 2017
Citation: Aejaz UH, Victor HK, Jones KR. A Bair’s Crushing Hug: An Unusual Cause of Pseudo pneumothorax. Arch Med. 2017, 9:1 doi: 10.21767/1989-5216.1000184
Copyright: © 2017 Aejaz UH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Pseudo-pneumothorax; Antibiotics; Radiologist
Case report
A 64-year-old male with a history of smoking and recurrent pleural effusions with multiple chest tube placements in the past was admitted to the ICU with anasarca, bilateral moderate pleural effusions, dyspnea and hypothermia of 30.4°C. He was slowly rewarmed with a Bair Hugger warming blanket, started on empiric antibiotics and diuresed with intravenous furosemide. Supplemental oxygen was also provided via nasal cannula. Despite this, he developed worsening respiratory failure (Arterial blood gas: pH 7.22, PaCO2 57 mmHg, PaO2 48 mmHg, Oxygen saturation of 75% on FiO2 0.6) and was placed on Bi-level Positive Airway Pressure (BiPAP).
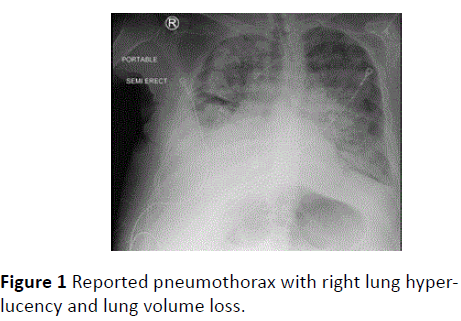
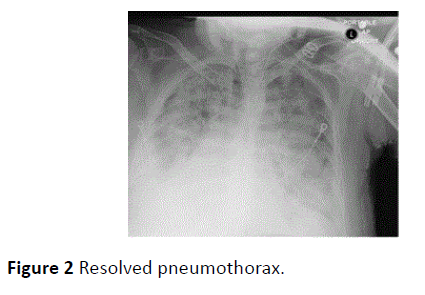
Intubation was contemplated, but the family refused, and further management continued on BiPAP. On clinical examination he was hemodynamically stable, tachypnic (respiratory rate of 36 breath/min) and in respiratory distress with poor inspiratory effort and coarse but equal breath sounds bilaterally. A portable chest X-ray showed right lung hyperlucency with lung volume loss (Figure 1), which was read as an occult pneumothorax by the radiologist. An emergent chest tube placement was indicated and during its preparation, the Bair Hugger warming blanket was noticed, unknown if it had been removed for imaging [1-4]. A repeat chest X-ray without the blanket was obtained which showed a spontaneously ‘resolved’ pneumothorax (Figure 2).
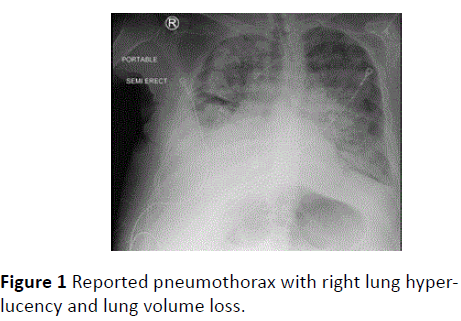
Figure 1: Reported pneumothorax with right lung hyperlucency and lung volume loss.
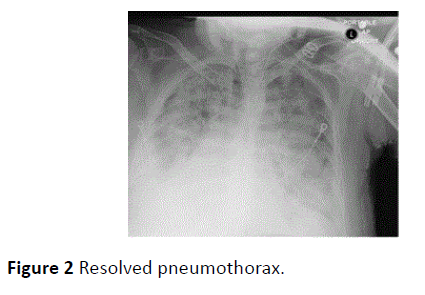
Figure 2: Resolved pneumothorax.
Discussion
Although suspicion for a pneumothorax should remain high in patients on positive pressure ventilation, esp. with increased oxygen requirements and appropriate radiographic findings, it is important to correlate with the patient’s clinical exam [5].
A pseudo-pneumothorax may closely mimic a true pneumothorax, even to an experienced radiologist, and can be caused by skin folds, pleural cysts, colonic interposition or herniated abdominal viscera, and as in this case, a Bair Hugger warming blanket. Clues to correctly identifying a pseudopneumothorax include:
• Presence of lung markings distils to the pseudo-lung border.
• A distally fading or broad lung border in contrast to a distinct hair-like pleural line seen in a pneumothorax.
• The color contrast across the lung border in a pneumothorax is much more dramatic and sharp compared to a pseudopneumothorax.
• A lung ultrasound (LUS) to identify B-lines and lung sliding.
• A pseudo-lung border extending beyond the anatomical chest wall.
Accurate and timely identification can prevent unnecessary interventions which may lead to complications including the formation of a pneumothorax.
18347
References
- Melton LJ, Hepper NG, Offord K P(1979) Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis 120: 1379-1382.
- Simonds AK (2004) Pneumothorax: an important complication of non-invasive ventilation in neuromuscular disease. NeuromusculDisord 14: 351-352.
- Hsu CW, Sun SF, Lee DL, Chu KA, Lin HS (2014) Clinical characteristics, hospital outcome and prognostic factors of patients with ventilator-related pneumothorax. Minerva Anestesiol80: 29-38.
- Fisher JK (1978) Skin fold versus pneumothorax. AJR Am J Roentgenol130: 791-792.
- Punyadasa A, Augustine T (2008) Pseudopneumothorax - Hold that chest tube. Int J Emerg Med 1: 59-60.