Sasapu A1*, Arnaoutakis K2 and Pandey T3
1Department of Gastroenterology, University of Arkansas for Medical Sciences, Little Rock, Arkansas, United States
2Department of Internal Medicine, University of Arkansas for Medical Sciences, Little Rock, Arkansas, United States
3Department of Radiology, University of Arkansas for Medical Sciences, Little Rock, Arkansas, United States
Corresponding Author:
Appalanaidu Sasapu
Department of Gastroenterology, University of Arkansas for Medical Sciences
Little Rock, Arkansas 72205, United States
Tel: (501) 296-1200
E-mail: asasapu@uams.edu
Keywords
Avascular necrosis, germ cell tumor, BEP, Corticosteroids, hip pain
Case Report
Mr. A is 21-year-old Caucasian man with history of testicular cancer presents to clinic complaining of pain in his left hip for 2-3 weeks. Pain radiates to thigh and has progressively getting worse. This required him to limit his activity and is unable to sleep or work due to the pain. He denies obvious physical trauma. He had been diagnosed with stage IS non-seminomatous germ cell tumor of testis (NSGCT) and was in remission having completed chemotherapy 9 months earlier.
He has undergone radical right orchiectomy in March, 2012 and was started on chemotherapy with BEP (Blemoycin, Etoposide, and Cisplatin) in June, 2012. He completed all three cycles of BEP chemotherapy by August, 2012. Chemotherapy consisted of etoposide 100 mg/m2 on days 1 to 5, cisplatin 20 mg/m2 on days 1 to 5, and bleomycin 30 IU on day 2, 9 and16. Dexamethasone 12 mg by mouth was given as premedication on days 1 to 5, 9, and 16 of each cycle, totaling 252 mg. He tolerated chemotherapy well except for mild nausea/vomiting. He also received 90 tablets of dexamethasone 4 mg, by mouth as needed for nausea and his low energy level totaling to 360 mg. He developed skin rash during the course of chemotherapy and was given oral prednisone 40 mg for five days (total 200 mg). In total, he likely received 4280 mg of equivalent dose of prednisone during his treatment course (4mg of dexamethasone=26.6 mg of prednisone). His tumor markers (AFP, Beta-HCG) have normalized and CT scans showed no evidence of metastatic disease in March, 2013.
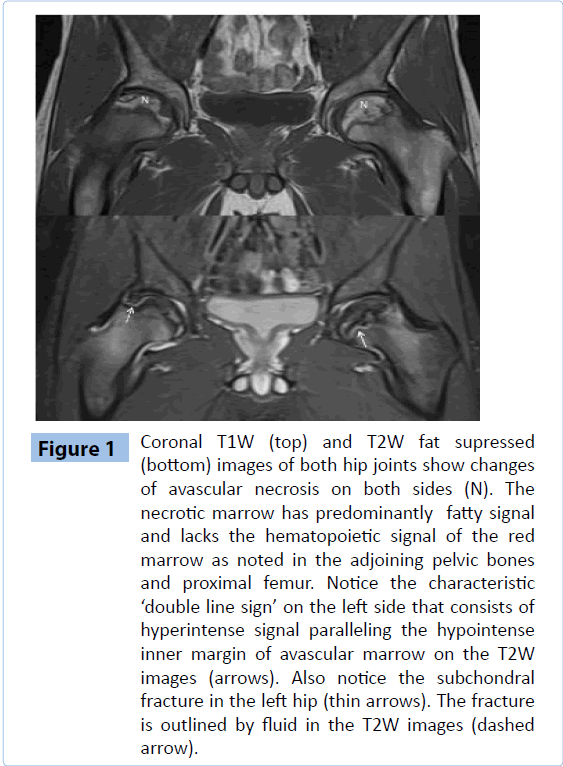
His family history is unremarkable. He has no children and is single. He smokes cigarettes occasionally. He has no known drug allergies. On review of systems, he has right hip pain, but denied fevers or night sweats. No weight loss. He has no respiratory or cardiac complaints. He denied muscular discomfort, joint pain or swelling. He was a very active person. His physical exam is significant for right inguinal scar from orchiectomy. He has absent right testis. He does not have any hepato-splenomegaly or lymphadenopathy. He has left hip pain and discomfort, particularly on external rotation. Extension of the left hip caused increased pain (Figure 1).
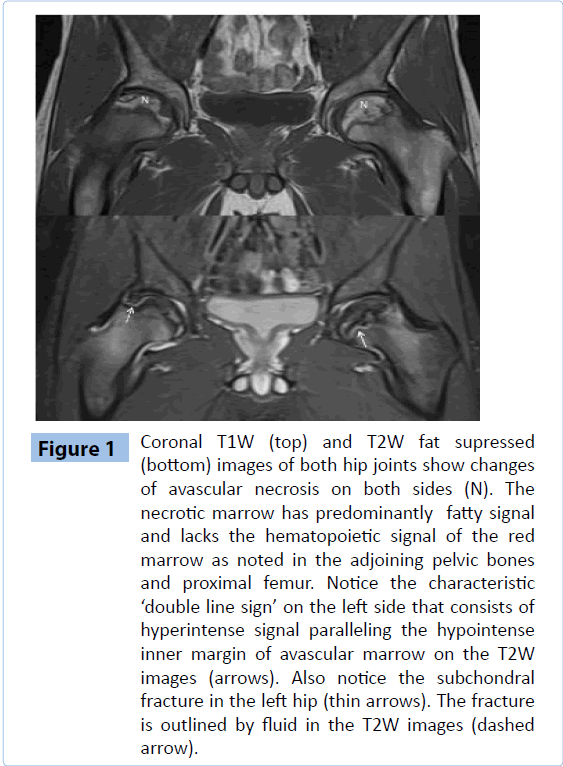
Figure 1: Coronal T1W (top) and T2W fat supressed (bottom) images of both hip joints show changes of avascular necrosis on both sides (N). The necrotic marrow has predominantly fatty signal and lacks the hematopoietic signal of the red marrow as noted in the adjoining pelvic bones and proximal femur. Notice the characteristic ‘double line sign’ on the left side that consists of hyperintense signal paralleling the hypointense inner margin of avascular marrow on the T2W images (arrows). Also notice the subchondral fracture in the left hip (thin arrows). The fracture is outlined by fluid in the T2W images (dashed arrow).
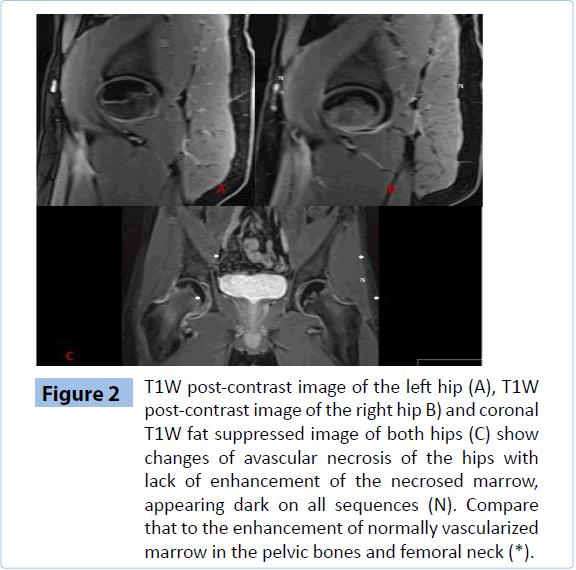
MRI hips showed avascular necrosis involving both femoral heads with serpiginous signal abnormality seen bilaterally and a double line sign seen on the left. He was seen by orthopedics and recommended non-steroidal anti-inflammatory drugs and physical therapy for range of motion exercises. He was advised to limit his weight bearing to only as needed. Patient declined initially surgical intervention. After 6 weeks of above measures, his pain and range of motion got better. He later underwent bilateral hip replacement due to unsatisfactory level of pain and function (Figure 2).
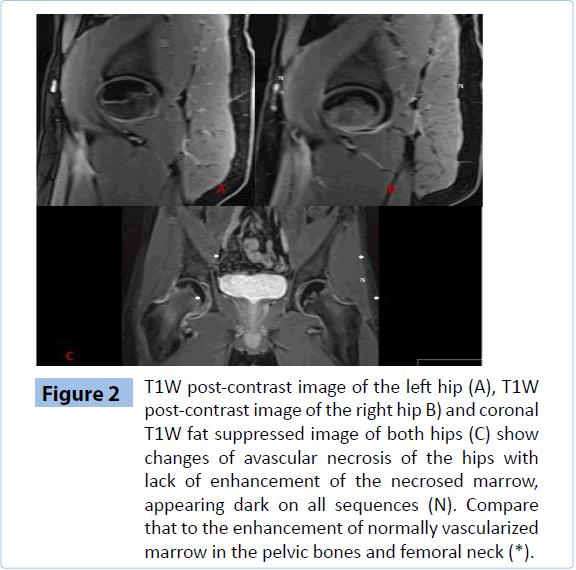
Figure 1: T1W post-contrast image of the left hip (A), T1W post-contrast image of the right hip B) and coronal T1W fat suppressed image of both hips (C) show changes of avascular necrosis of the hips with lack of enhancement of the necrosed marrow, appearing dark on all sequences (N). Compare that to the enhancement of normally vascularized marrow in the pelvic bones and femoral neck (*).
Discussion
Testicular cancer is the most common solid tumor in men between the ages of 20 and 35 years. Testicular cancer has very high cure rates with current chemotherapy even in advanced disease. Avascular necrosis (AVN) is a well reported complication of chemotherapy when given with high-dose corticosteroids in patients treated for lymphoma and solid tumors like testicular cancer [1-3, 4-10]. It was also, though less commonly, reported in patients who received combination chemotherapy without any steroids [4].
Femoral head is the most commonly affected site [1, 2]. Risk factors for the development of avascular necrosis include corticosteroids, radiotherapy, alcohol use, Caisson’s disease, sickle cell disease, and trauma [9-10, 11]. AVN occurring at single site is usually from trauma, but it can occur at multiple sites from conditions like sickle cell disease, collagen vascular disease, radiation, and chemotherapy. Corticosteroid use is associated with single or multiple site AVNs [12].
In one study, the prevalence of AVN in patients who have received chemotherapy for testicular tumors was as high as 9%. In this study, mean steroid dose was 2.25 g of prednisolone equivalent. The affected patients received BEP chemotherapy at three or four cycles. AVN was diagnosed at a median of 21 months (range 14–32 months) after the start of chemotherapy [5]. The mean cumulative dose of steroids in other reports varied from 1.8 g to 19.8 g [6-9]. The risk of femoral head osteonecrosis is greatest during the first 12 months after steroid treatment with chemotherapy. In patients with malignant disease it occurs as early as 2 months, and as late as 78 months after starting steroids [9].
Presenting complaints are groin or hip pain. Radiological studies are indicated in patients with persistent hip pain, when there is no obvious cause. Radiological changes can precede symptoms by several months. MRI is the most specific and sensitive modality if there is suspicion for AVN of femoral heads [1-3].
In our patient the cumulative dose of ‘‘prednisone equivalent’’ delivered prior to onset of symptoms was 4.28 g. He developed symptoms of osteonecrosis 9 months after the corticosteroid administration with bilateral hip involvement. Oncologists should be cautious in the use of steroids especially in young patients with testicular cancer who are treated with BEP. This uncommon but significant side effect should also be discussed with patients.
6595
References
- Winquist EW, Bauman GS, Balogh J (2001) Nontraumatic osteonecrosis after chemotherapy for testicular cancer: a systematic review. Am J ClinOncol 24: 603-606.
- Shim K, MacKenzieMJ, Winquist E (2008) Chemotherapy-associated osteonecrosis in cancer patients with solid tumours: a systematic review. Drug Saf 31: 359-371.
- Fung C, Vaughn DJ (2011) Complications associated with chemotherapy in testicular cancer management. Nat Rev Urol 8: 213-222.
- Harper PG, Trask C, SouhamiRL (1984) Avascular necrosis of bone caused by combination chemotherapy without corticosteroids. Br Med J (Clin Res Ed) 288: 267-268.
- Cook AM, Dzik-Jurasz AS, Padhani AR, Norman A, Huddart RA (2001) The prevalence of avascular necrosis in patients treated with chemotherapy for testicular tumours. Br J Cancer 85: 1624-1626.
- Cook AM, Patterson H, Nicholls J, Huddart RA (1999) Avascular necrosis in patients treated with BEP chemotherapy for testicular tumours. ClinOncol (R CollRadiol) 11: 126-127.
- Coles C, Williams M (2000) Avascular necrosis in patients treated with BEP chemotherapy for testicular tumours. ClinOncol (R CollRadiol) 12: 69.
- Forrai G, Baki M, Bodrogi I (1994) Incidence of osteoporosis and aseptic femur head necrosis following complex therapy of germ cell testicular tumors. OrvosiHetilap, 135: 1695-1700.
- Kaila R, Wolman R L (2006) Groin pain in athletes: A consequence of femoral head avascular necrosis after testicular cancer chemotherapy. Clin J Sport Med. 16: 175-176.
- van den Berkmortel F, de Wit R, de Rooy J, DeMulder P (2004) Osteonecrosis in patients with testicular tumours treated with chemotherapy. Neth J Med 62: 23-27.
- Renedo RJ, Sousa MM, Pérez SF, Zabalbeascoa JR, Carro LP (2010) Avascular necrosis of the femoral head in patients with Hodgkin's disease. Hip Int 20: 473-481.
- Virik K, Karapetis C, Droufakou S, Harper P (2001) Avascular necrosis of bone: the hidden risk of glucocorticoids used as antiemetics in cancer chemotherapy. Int J ClinPract 55: 344-345.