Allam Fayez Abuhamda1* and El-Sakka Mazen2
1Shifa Women`S Hospital, Shifa Nicu, Ministry of Health, Gaza, Palestine, Qatar
2Faculty of Pharmacy, Al Azhar University, Gaza, Palestine, Qatar
*Corresponding Author:
Allam Fayez Abuhamda
Consultant Neonatologist, Shifa Women`S Hospital
Shifa Nicu, Ministry of Health, Gaza, Palestine, Qatar
Tel: +97082829468
E-mail: allam570@yahoo.com
Received Date: July 29, 2018; Accepted Date: September 11, 2018; Published Date: September 13, 2018
Citation: Abuhamda AF, Mazen ES (2018) A Case Study of Prune Belly Syndrome with Congenital Vesico-Subumbilical Skin Fistula. Ann Clin Lab Res Vol.6 No.3:254. DOI: 10.21767/2386-5180.100254
Keywords
Prune belly syndromes; Palestinian neonate; Vesico-subumbilical skin fistula
Introduction
Prune Belly syndrome (PBS) is a rare congenital disorder affecting about 1 in 30,000 birth of which about 96% of those affected are male [1-4]. Three main features of PBS; abdominal wall muscular layer defect, urinary system malformation and bilateral cryptorchidism. The pathogenesis of PBS is still an unsettled controversy with the following predominating theories: The first theory proposes a prenatal obstruction of the urinary tract, the second theory proposes the failure of primary mesodermal differentiation between the 6th and 10th week of gestational age, and the third theory proposes dysgenesis of the yolk sac and allantois as causative for PBS [5,6]. PBS could be associated with chromosomal anomalies like; turner syndrome, trisomy 21, trisomy 18 and trisomy 13 [7,8]. The familial transmission was reported as autosomal recessive [9]. A muscarinic acetylcholine receptor M3 (CHRM3) (1q41-q44) homozygous frame shift mutation in familial congenital bladder malformation associated with a prunebelly- like syndrome [10]. But more studies is need to find out the responsible gene [11,12].
The PBS characterized by the deficient development of abdominal muscles that causes the skin of the abdomen to wrinkle like a prune, bilateral cryptorchidism, abnormalities of the urinary tract such as bilateral gross hydronephrosis, megaureter, and megacystis.
This article presents a case of neonate seen in our institution Al Shifa Hospital-Gaza, State of Palestine, presenting of PBS with congenital vesico-subumbilical fistula.
Case Report
Mother is G1P1, at 16th weeks gestational age by antenatal ultrasound found to have a fluid collection within the fetal abdomen 9 cm diameter was noted, suspected as fetal ascites or cyst. The fluid decreased gradually and disappeared at 33rd week gestational age, at 36th week gestational age abnormal curvature of the fetal vertebral column was noted but no ascites.
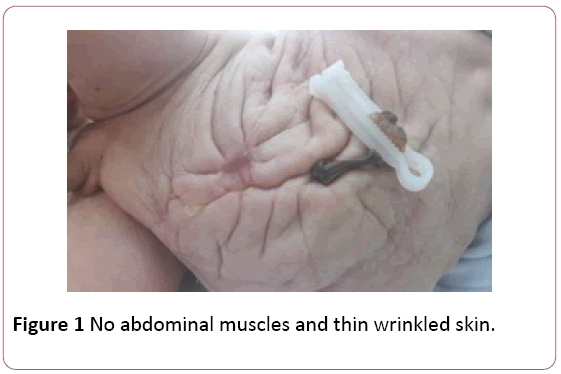
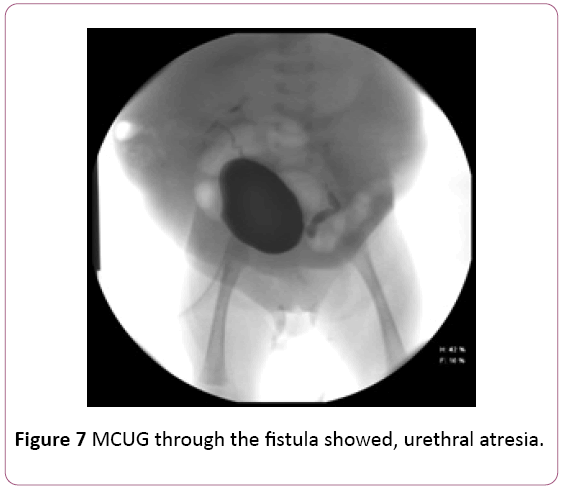
The baby was male, birth was through cesarean delivery due to obstructed normal labor, Apgar score was 7, 9 at 1, 5 minute respectively, birth weight was 2900 grams. He was the 1st sibling to the parents. There was no familial history of the congenital disease. Physical examination of the infant showed a normal tone. Abdominal examination revealed a soft abdomen no distention no organomegaly with thin wrinkled skin (Figure 1) kidneys and bladder are not palpable. Abdominal examination showed a small skin fistula opening below the umbilicus pouring urine (Figures 2 and 3). Genital examination showed small phallus with bilateral non-palpable testes and empty scrotum scrotal skin showed little rugae. Other systemic examination revealed no abnormality. Serum electrolytes at 1st day and 5th days of age were in normal range sodium was 141 mmol/l, potassium was 3.5 mmol/l and total calcium was 8.6 mg/dl, at five days of age urea was 16 mg/dl and creatinine was 0.51 mg/dl, renal ultrasound.
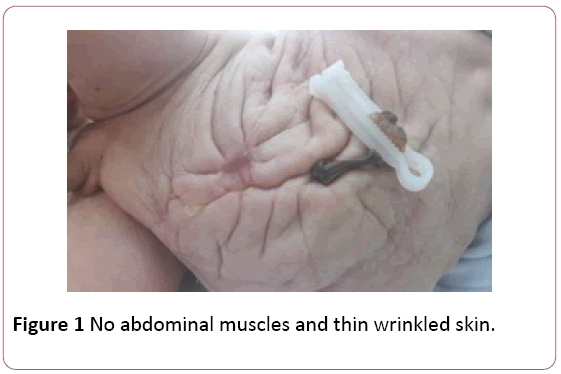
Figure 1: No abdominal muscles and thin wrinkled skin.

Figure 2: Urine is coming out from the opening of the fistula.

Figure 3: Vesico-subumbilical abdominal skin fistula.
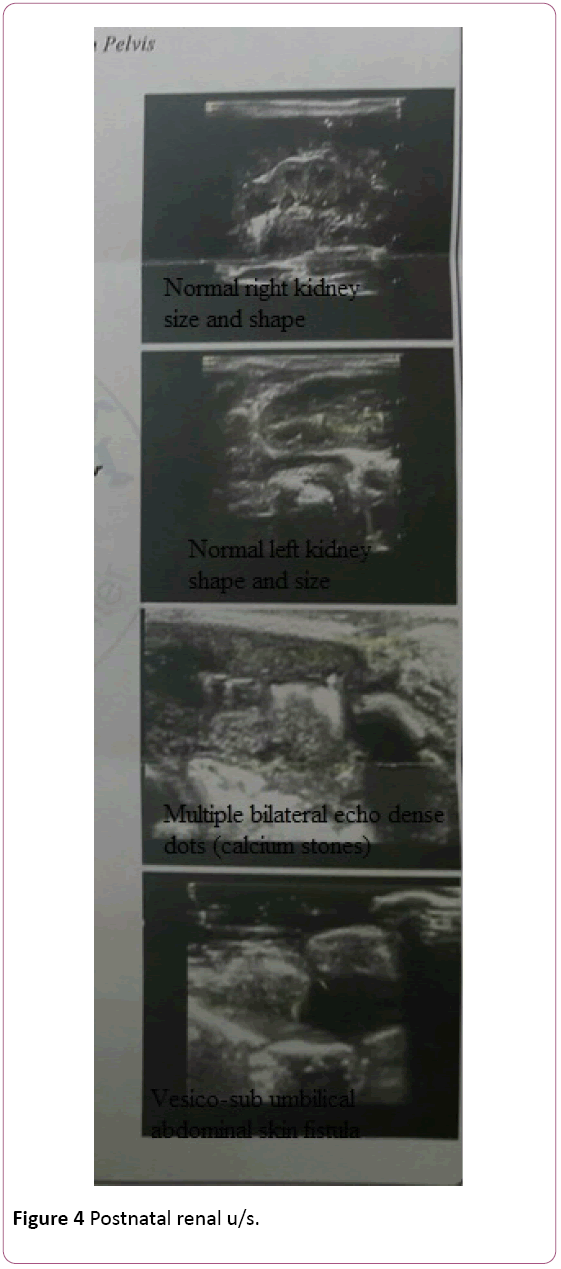
Post natal renal U/S showed; both kidneys had normal shape, normal size, normal echogenicity and well– differentiated corticomedullary junction, no cyst, no mass no hydronephrosis but multiple bilateral echo dense dots (calcium stones), urinary bladder was empty during whole exam and a small tract connected from the anterior wall of urinary bladder to skin opening (fistula) (Figure 4). Echocardiography and chest X-ray both were normal study.
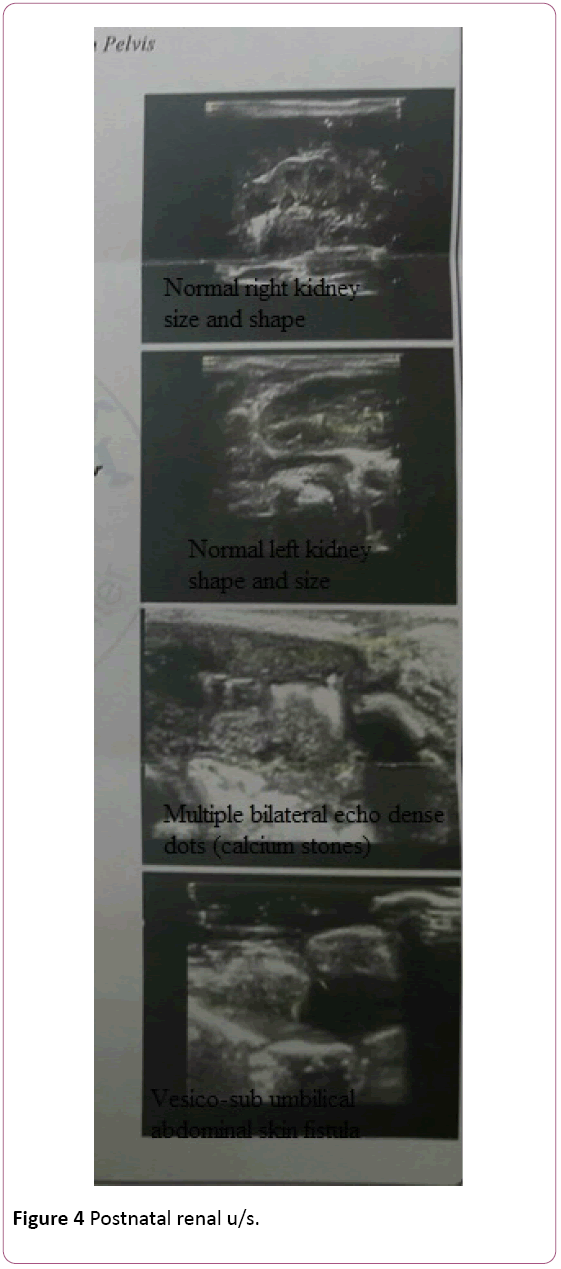
Figure 4: Postnatal renal u/s.
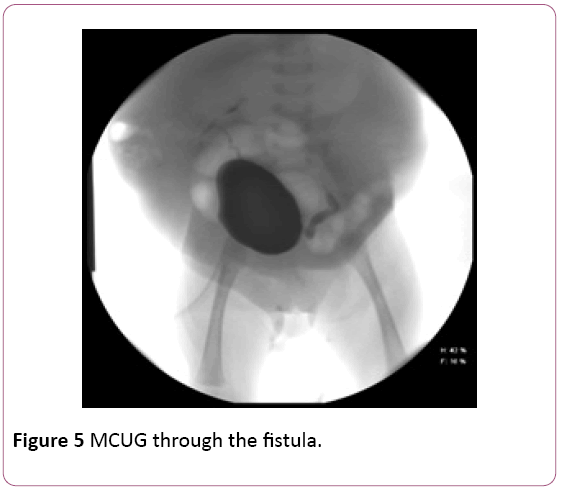
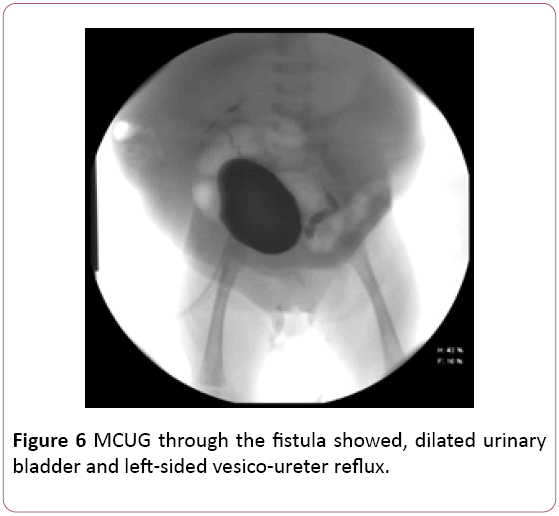
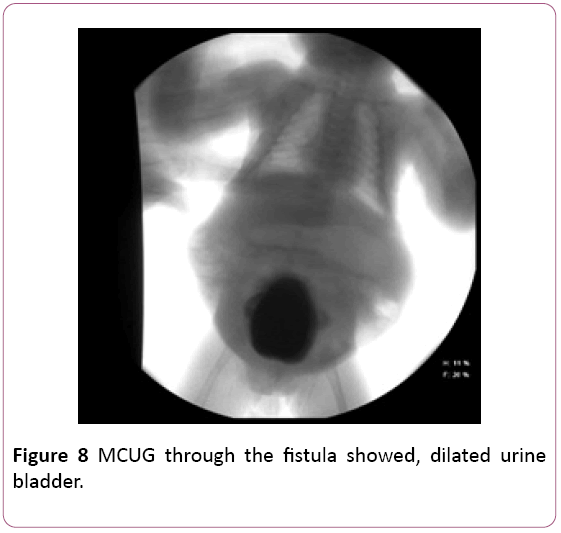
Baby was evaluated by a pediatric surgeon, VCUG was recommended to be done at the of 5th days of age, pediatric surgeon failed to insert the catheter through the urethra as suspected urethral atresia, dye was given through the vesicosubumbilical abdominal skin fistula, the study showed mildly dilated bladder and left-sided ureteral reflux (Figures 5-8).
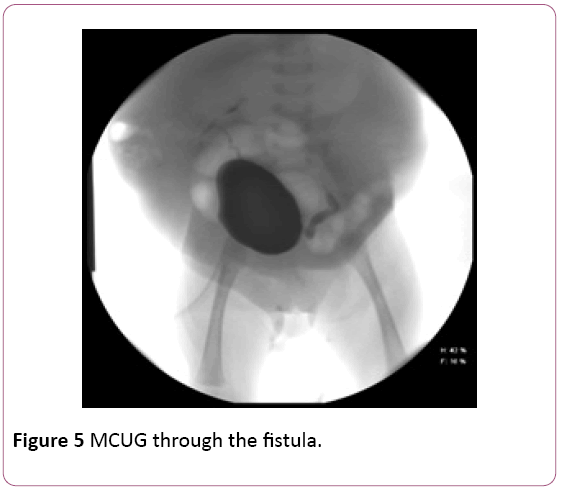
Figure 5: MCUG through the fistula.
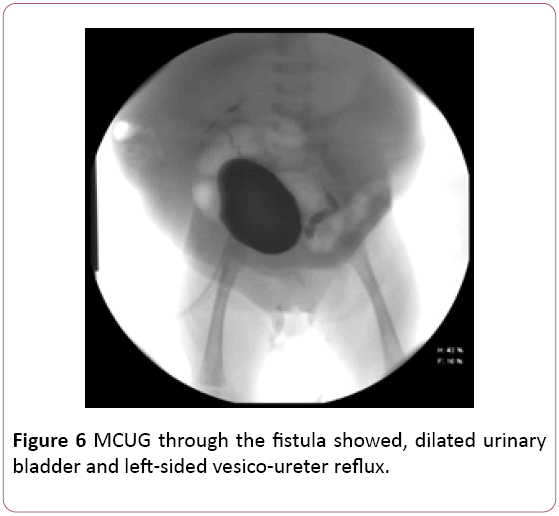
Figure 6: MCUG through the fistula showed, dilated urinary bladder and left-sided vesico-ureter reflux.
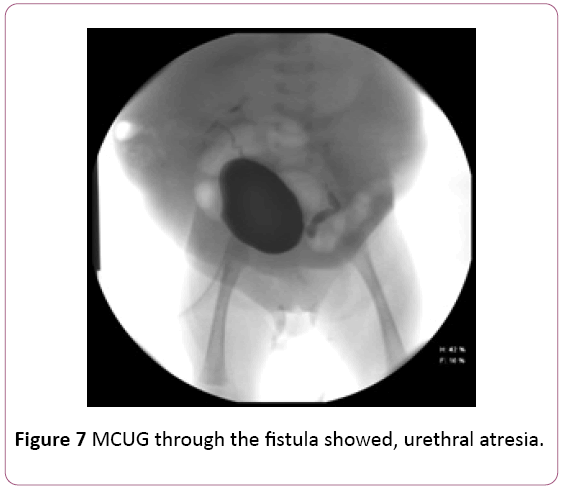
Figure 7: MCUG through the fistula showed, urethral atresia.
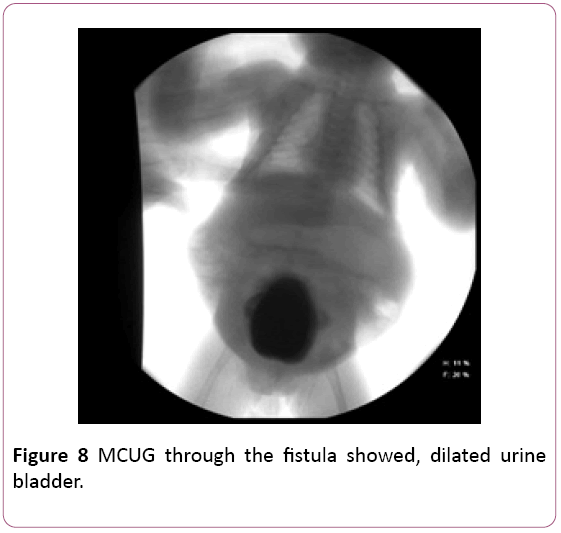
Figure 8: MCUG through the fistula showed, dilated urine bladder.
The baby was discharged home at the age of 4 hours in good general condition with a daily oral single prophylactic dose of amoxicillin. He was active, sucking well, no distress on room air. The patient had no abdominal muscles and wrinkled abdominal skin.
Discussion
All these clinical features were consistent with the prunebelly syndrome. The patient had urethral atresia as there was small phallus and the smallest urine catheter did not pass through the urethra. The patient also had vesico-subumbilical abdominal skin fistula as the urine came out from the fistula skin opening. Postal renal ultrasonography showed both kidneys with normal size, shape, and echogenicity. MCUG and renal ultrasound showed the fistula between the urinary bladder and abdominal skin. Renal function test and see um electrolytes were normal. All these clinical data, laboratory result, and imaging were suggestive of a rare case of PBS with sub umbilical skin fistula which had major role by the release of urinary tract obstruction and protection of kidney and lung function.
The diagnosis has been broadly inclusive by using clinical and morphological e features in combination. Clinical features of our patient were similar as those described in the literature and were diagnosed as PBS. The bladder outlet or distal urethral obstruction led to the urinary tract obstruction, dilatation of bladder and vesico-ureter reflux as documented by MCUG.
The antenatal ultrasound at 16 gestations which showed ascites, it was mostly related to urine accumulation in the abdominal cavity as urine bladder had fistula to abdomen cavity then later veico-subumbilical skin fistula well formed. By the progression of gestational age, the abdominal collection totally was recovered through the fistula to the amniotic fluid.
Bladder outlet obstruction and atrophied abdominal wall created the vesico-subumbilical skin fistula which in turn releases the urine and the obstruction and maintained normal anatomy and function of both kidneys and lung.
Conclusions and Recommendations
• A rare case of PBS with subumbilical abdominal skin fistula.
• The case needed multidisciplinary approach included; paediatric surgeon, paediatric urologist, paediatric nephrologist and paediatrician.
• The patient needs surgical intervention for vesicostomy, repair of the atretic urethra, undescended testis, and augmentation of abdominal muscles [13,14].
• Ministry of health in Gaza needs a tertiary center with different subspecialties to include; paediatric surgeon and paediatric urologist to manage these complicated cases.
Conflict of Interest
The authors declare no conflict of interests.
23418
References
- Sunil Kumar Samal, Setu Rathod (2015) A rare case report. J Nat Sci Biol Med 6(1): 255-257.
- Aloni MN, Mujinga V, Tady BM, Nkidiaka ED (2015) A first description of prune belly syndrome in central Africa. Pediatr Neonatol 56(5): 355-356.
- We Xu, Hui Wu, Dong-Xuan Wang, Zhi-Hong Mu (2015) A case of prune belly syndrome. Pediatr Neonatol 56: 193-196.
- Cascio, Salvatore, Hideshi Miyakita, Prem Puri (2017) Prune belly syndrome: Newborn surgery. CRC Press pp: 813-820.
- Andreas Fette (2015) Associated rare anomalies in prune belly synsdrome: A case report. J Ped Surg 3: 65-71.
- Joseph, David B (2016) Congenital anomalies of the kidney and urinary tract. Springer, Cham pp: 197-213.
- Daldrup-Link HE, Newman B (2014) Pearls and pitfalls in pediatric imaging: Variants and other difficult diagnoses. Cambridge University Press.
- Metwalley KA, Farghalley HS, Abd-Elsayed AA (2008) Prune belly syndrome in an Egyptian infant with Down syndrome: A case report. J Med Case Rep 2(1): 322.
- Sarhan OM, Al-Ghanbar MS, Nakshabandi ZM (2013) Prune belly syndrome with urethral hypoplasia and vesico-cutaneous fistula: A case report and review of literature. Urology annals 5(4): 296.
- Weber S, Thiele H, Mir S, Toliat MR, Sozeri B, et al. (2011) Muscarinic acetylcholine receptor M3 mutation causes urinary bladder disease and a prune-belly-like syndrome. Am J Hum Genet 89(5): 668-674.
- Brewer, Fallon R, Lorie M Harper (2017) Obstetric imaging: Fetal diagnosis and care (2nd Ed.) pp: 574-576.
- Boghossian NS, Sicko RJ, Giannakou A, Dimopoulos A, Caggana M, et al. (2018) Rare copy number variants identified in prune belly syndrome. Eur J Med Genet 61(3): 145-151.
- Hassett S, Smith GH, Holland AJ (2012) Prune belly syndrome. Pediatr Surg Int 28(3): 219-228.
- Ekwunife OH, Ugwu JO, Modekwe V (2014) Prune belly syndrome: early management outcome of nine consecutive cases. Niger J Clin Pract 17(4): 425-430.