Keywords
Tuberculosis, Multi drug resistant, Prevalence, Bangladesh
Introduction
Drug-resistant tuberculosis (TB) is caused by M. tuberculosis organisms that are resistant to the drugs normally used to treat the disease. Drug-resistant TB is transmitted in the same way as drugsusceptible TB, and is no more infectious than drug-susceptible TB. However, delay in the recognition of drug resistance or prolonged periods of infectiousness may facilitate increased transmission and further development of drug resistance [1]. Multidrugresistant TB (MDR TB) is caused by organisms resistant to the most effective anti-TB drugs, isoniazid and rifampin. These drugs are considered first-line drugs and are used to treat most persons with TB disease [2,3]. Extensively drug-resistant TB (XDR TB) is a relatively rare type of drug-resistant TB. XDR TB is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Because XDR TB is resistant to first-line and second-line drugs, patients are left with treatment options that are more toxic, more expensive, and much less effective [4]. Data from national drug resistance surveys indicate low levels of MDRTB. A population-based survey is planned in 2009 to evaluate the magnitude of drug resistance. Isolated surveys have indicated that MDR-TB rates among newly diagnosed cases range between 0.4% and 3% and among previously treated cases, between 3% and 15.4%. A limited survey of drug susceptibility among patients failing category II regimens showed that 88% had MDR-TB [5].
Here our objective of this study is to compare the clinical parameters and characteristics of TB with or without MDR found in Bangladesh.
Methods
Study design
This is a cross sectional (descriptive) study, where data was collected through interviews with a structured questionnaire as well as recorded data of each patient.
Study area
The study was carried out at the inpatient department of National Institute of Diseases of the Chest and Hospital, NIDCH, Dhaka, the only tertiary referral hospital for TB and chest disease in Bangladesh, located in the central part of Dhaka Metropolitan City. Patients from all over the country mostly as referral cases attend this health facility. The study subjects were grouped randomly.
Study Populations
A total of 100 newly diagnosed and former patients with or without MDR of both sexes, ages varied from 20 to over 60 years were included in this study between May 2012 and May 2013.
Data collection
Patients were randomly interviewed and enrolled the cases from the TB patients admitted during the study period at NIDCH with or without previous history of TB and/or other complications including pleural effusion, anti-TB drug intolerance, ailing patients etc. The patients were diagnosed as having PTB on the basis of presenting symptoms, clinical signs, two acid-fast bacillus (AFB) smear-positive sputum samples and chest X-ray, if necessary. The patients were being treated with recommended standardized treatment regimen according to the patient category following the national TB control guidelines [6,7].
The pulmonary TB patients were interviewed by the researcher using structured questionnaires. Clinical information including their personal and social information, clinical presentation eg: signs and symptoms, date of diagnosis, date of treatment starting, weight variation, immunological change, age, hormonal change, associated diseases and their patterns, diagnosis pattern, type of TB, treatment of TB with or without MDR, follow-up of treatment and outcome were obtained directly from each patients and recorded data of each patients. I compared subjects with TB with or without MDR. The following covariates were evaluated: age, occupation, symptoms, Drugs taken during diagnosis and survey, diagnostic parameters, smoking and drug addiction, treatment patterns, vitamins taken, associated diseases and side effects of drugs. New TB patients were those cases who never had treatment for TB or who had taken anti-TB drugs for less than one month. Previously treated TB patients were patients who had received at least one month of anti-TB therapy. This is known as recurrence. Patients who relapsed after having successfully completed treatment in the past, patients who failed treatment, patients who returned after interrupting treatment and chronic TB cases (had failed at least one retreatment course) were also included in this category. Cases of relapse, treatment failure, treatment interruption and chronic TB were identified according to the definition of WHO [4].
Results
During the study period a total of 100 patients were interviewed. 37% patients were newly diagnosed, 23% patients were second time affected (relapse) and 40% patients were Multi Drug Resistant. Among TB patients (Newly diagnosed and relapse) 82% were male and 18% were female. Among MDR-TB patients 78% were male and 23% were female.
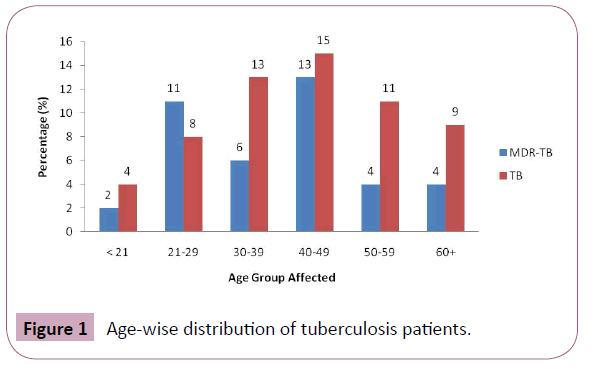
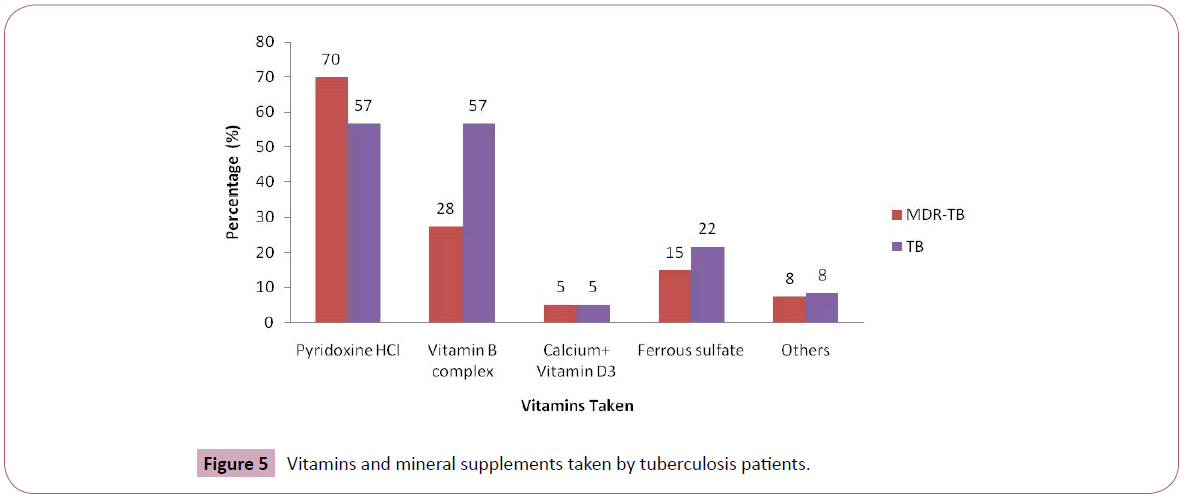
The mean age of the patients was 40.50 (range 21- 60+). 13% and 15% patients of MDR-TB and TB respectively were the age between 40- 49 (Figure 1). Among them 41% were from Dhaka division, the remaining 21%, 14%, 9%, 7%, 5% and 3% were from Chittagong, Barisal, Khulna, Sylhet, Rajshahi and Rangpur divisions respectively.
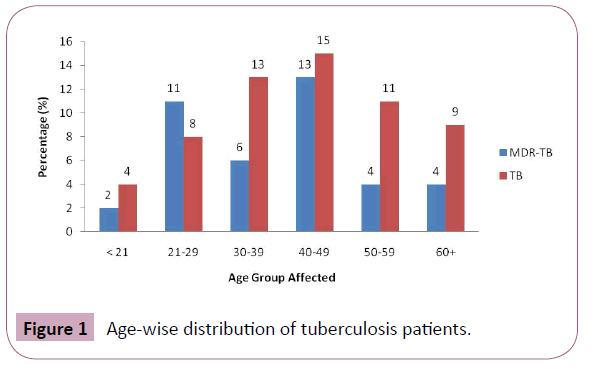
Figure 1: Age-wise distribution of tuberculosis patients.
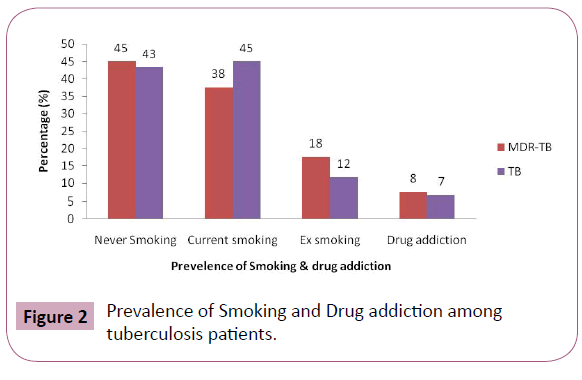
Among MDR-TB patients 33% and 15% Patients and Among TB patients 23% and 25% patients were labors and business/ Salesmen respectively. 38% of MDR-TB and 45% of TB patients were current smoker, 18% of MDR-TB and 12% of TB were past smoker and 8% of MDR-TB and 7% of TB patients were drug addicted (Figure 2).
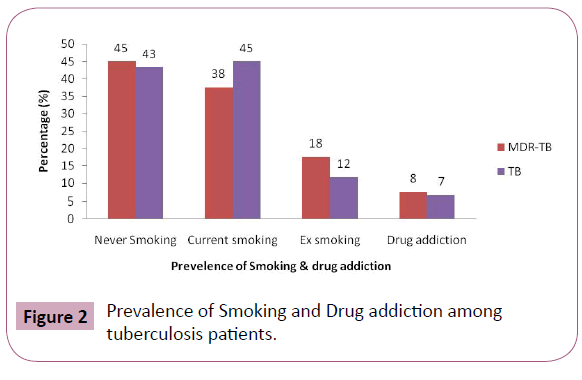
Figure 2: Prevalence of Smoking and Drug addiction among tuberculosis patients.
Presenting symptoms were more or less same for MDR-TB and TB patients. 98% of MDR-TB and 95% of TB were fever. 85% of MDR-TB and TB patients were anorexia, 45% of MDR-TB and 55% of TB patients were cough, 48% of MDR-TB and 40% TB patients were Haemopysis and 33% and 43% patients of MDR-TB and TB patients lost their weight affected after tuberculosis.
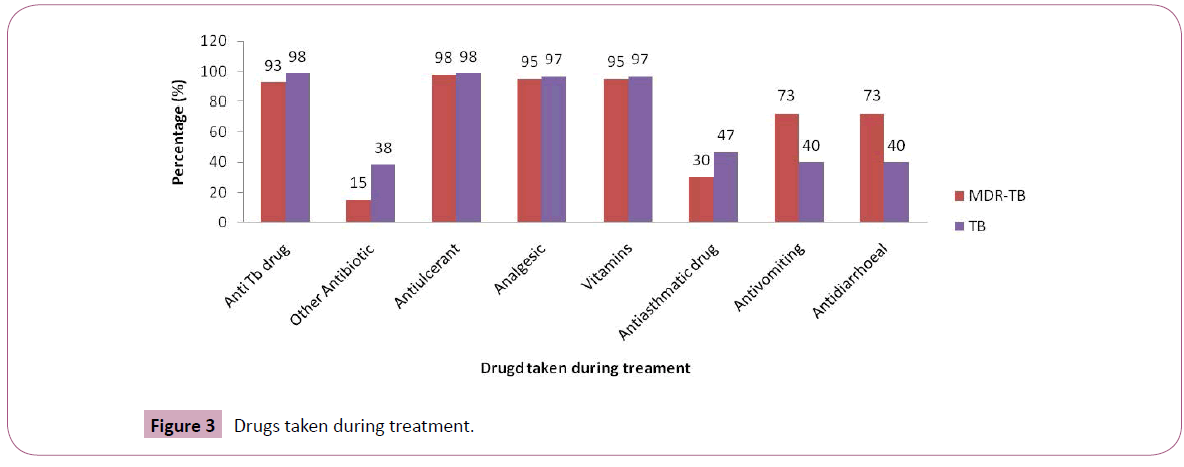
Both MDR-TB patients and TB patients were taken Antiulcerent, Analgesic and Vitamins 90% -100% patients during diagnosis and treatment period. During diagnosis 30% for MDR-TB and 22% for TB patients took Anti TB drugs. On the other hand during treatment 93% for MDR-TB and 98% for TB patients were taken Anti- TB drugs (Figure 3).
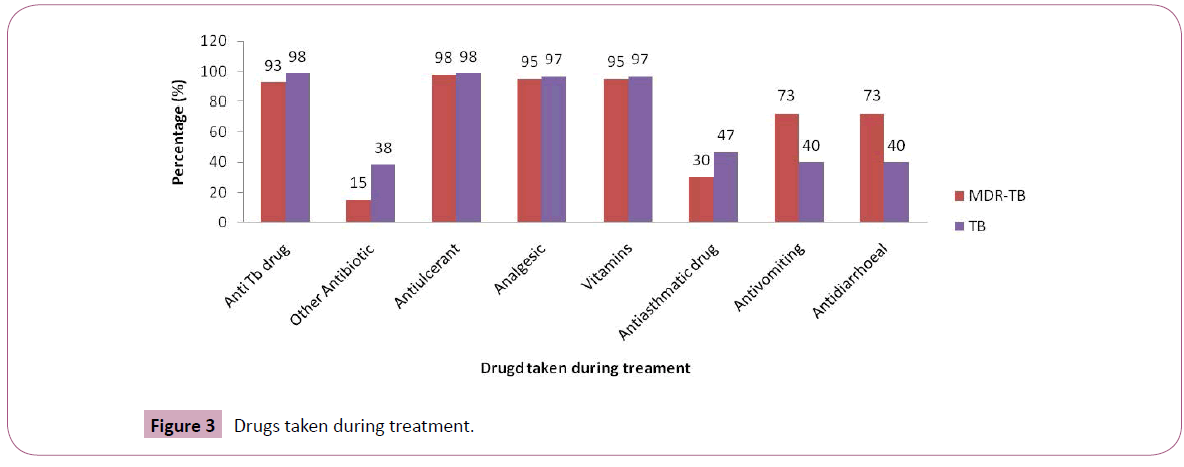
Figure 3: Drugs taken during treatment.
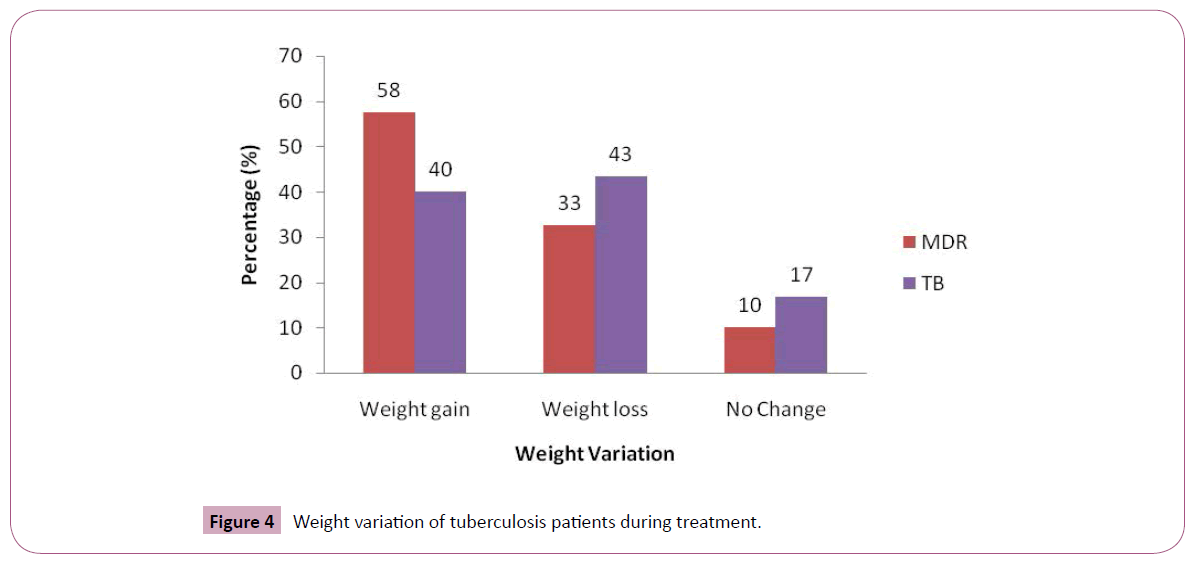
Among MDR-TB and TB patients 92% took first line oral agent and 62% took injectable agent and 43% took fluroqunolone drugs and 37% patients took second line therapy. After treatment, 58% and 40% gained weight, 33% and 43% lost weight and 10% and 17% neither gained nor lost weight of MDR-TB and TB patients respectively (Figure 4).
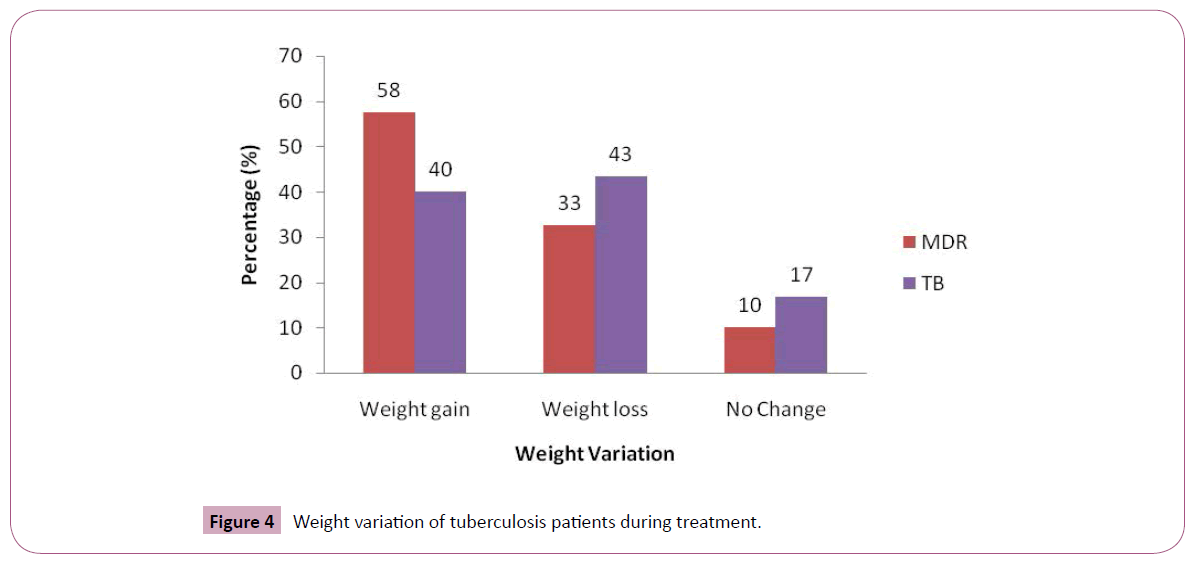
Figure 4: Weight variation of tuberculosis patients during treatment.
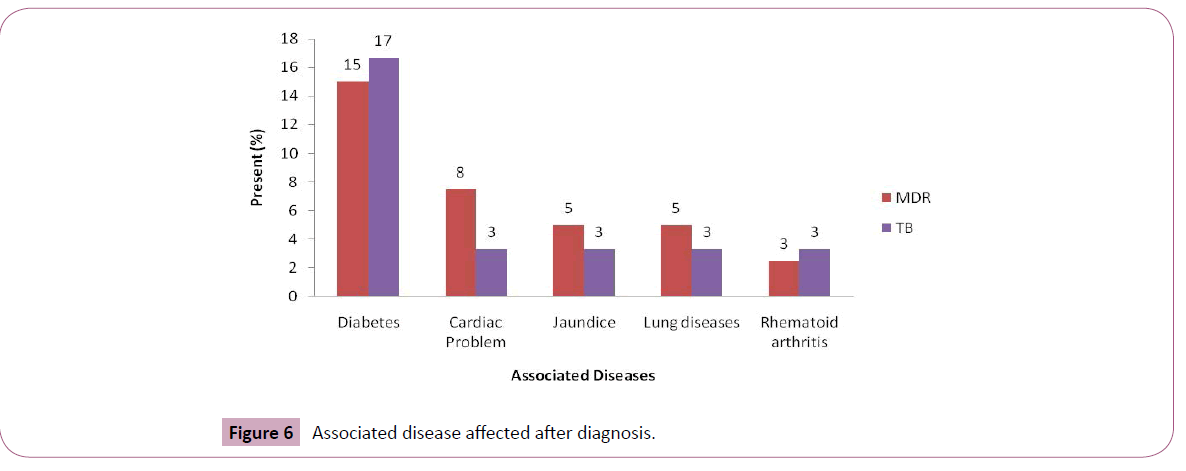
18% of MDR-TB and 52% of TB patients took folk medicine. 70% of MDR-TB and 57% of TB patients took Pyridoxine HCl and 28% of MDR-TB and 57% of TB took Vitamins B-Complex (Figure 5).
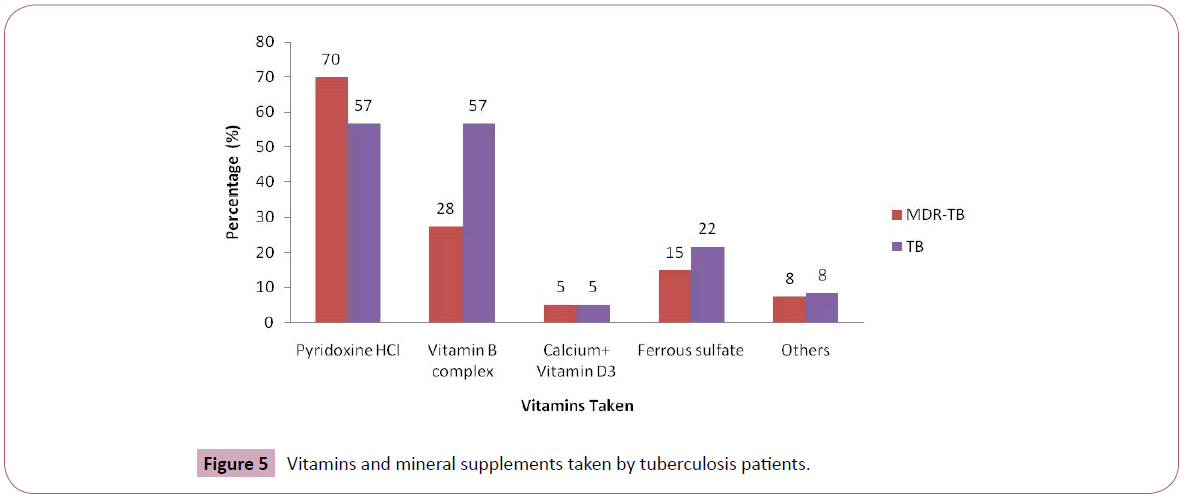
Figure 5: Vitamins and mineral supplements taken by tuberculosis patients.
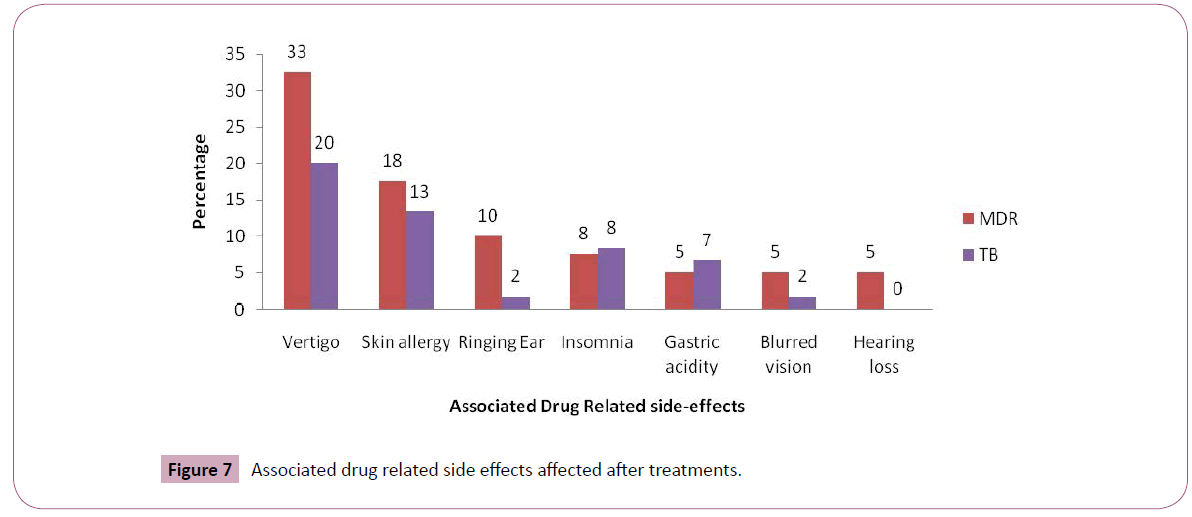
Diabetes was seen 15% of MDR-TB and 17% of TB patients. Cardiac Problem was seen 8% of MDR-TB and 3% of TB patients (Figure 6).
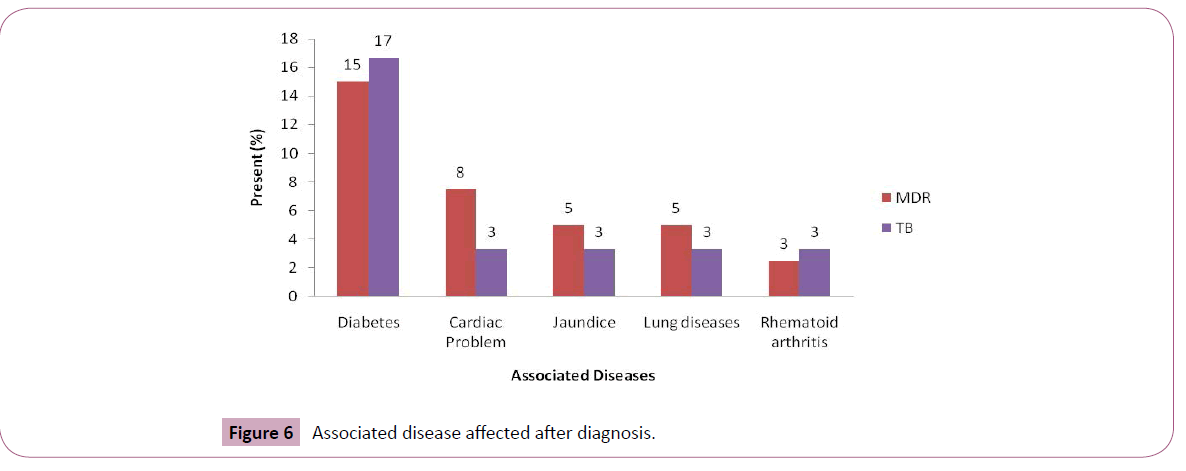
Figure 6: Associated disease affected after diagnosis
Vertigo was seen 33% of MDR-TB and 20% of TB patients. Skin allergy was seen 18% of MDR-TB and 13% of TB patients after treatment with tuberculosis drug (Figure 7).
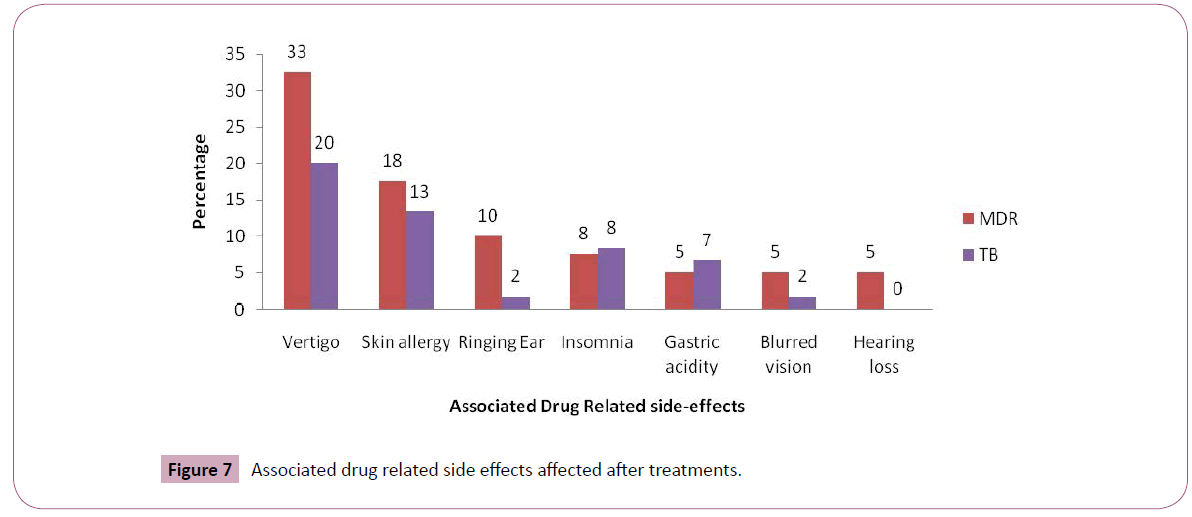
Figure 7: Associated drug related side effects affected after treatments.
Discussion
Tuberculosis (TB) especially affects the economically most productive age group and low income professionals. In the current study the mean age of the patients was 40-50 years ranging from 21-60+ years those are similar to other reported studies [8-10].
The prevalence was higher among the rural population compared to urban areas. Over the last several years, media initiatives, which are more commonly viewed by the urban population, advocated seeking appropriate care for symptoms of tuberculosis.
In this study Among Newly diagnosed and relapse TB patients 82% were male and 18% were female. Among MDR-TB patients 78% were male and 23% were female. One of the underlying causes for high rate of MDR-TB among males is believed to be the reduced adherence of males to treatment compared to females. Another important finding of our study was the higher incidence of MDRTB among the patients between the ages of 40-49 years. This is possibly due to the exposure of elderly persons to the organisms in the past, when the circulating bacilli were susceptible, and during the process of treatment, resistance was acquired while young patients are more likely to have acquired the bacilli more recently when they were more likely to be resistant. However, to confirm the findings of this study it is important to perform a molecular epidemiological study with a larger sample size.
Recently one study found that supplementation with vitamin E (140 mg alpha-tocopherol) and selenium (200 μg) reduces oxidative stress and enhances total antioxidant status in patients with pulmonary TB treated with standard chemotherapy. A link between tuberculosis and vitamin D deficiency has been postulated and fish liver oils and sunlight were sometimes used to treat tuberculosis before the advent of antimicrobial drug treatment. Low serum vitamin D levels are associated with higher risk of active tuberculosis and vitamin D deficiency has been postulated. A study from Rwanda reported vitamin A deficiency among adults with tuberculosis. Concentration of vitamin A was found to be lower in tuberculosis patients than that in controls in many studies [11]. In Ethiopians, concentrations of antioxidant vitamin C, vitamin E, and vitamin A were significantly lower in tuberculosis patients and high malonaldehyde concentration was associated with clinical severity [12]. B-complex vitamins help metabolize carbohydrates, proteins and fats into energy that can be utilized by the body. Low levels of B vitamins can cause excess fatigue. The UMMC advises patients taking tuberculosis medications to increase intake of foods rich in B vitamins. Patients should also take a multivitamin and 1 tablet of B-complex vitamin daily. In this study most of the patients took vitamin B complex as vitamin and among them very few are getting re-treatment.
Another study showed that roots, leaf and flower of Lantana camara L. and root of Clerodendrum indicum (L.) Kuntze can be used in the treatment of tuberculosis. In folklore, healing with garlic has been documented as far back as the 1920's (long before the advent of modern drugs) for helping with Tuberculosis. Another study tells that stem of Tinospora sinensis is used to treat Tuberculosis in South Sahapur, Noakhali district [13-15]. In this study, some patients are found taking folk medicines like Homeopathic syrup, Homeopathic purya, Neem leaf extract, Basil leaf extract etc to treat tuberculosis though the outcome is not that significant.
The weight of the patient taken at different time points during treatment is an important component to assess the progress of patients. Weight loss, a symptom that is considered immunosuppressive and a major determinant of severity and disease outcome (Vasantha et al.,). An earlier report showed that 39 (6%) of 676 TB patients died during the treatment period, and that higher death rates were independently associated with base line body weight <35 kgs and a history of previous treatment for TB [16,17]. Weight loss is associated with impaired physical function as well as increased mortality in patients with TB. In tuberculosis, there is a sudden dip in the appetite of an individual. Vomiting becomes common too, one of the factors responsible for triggering dramatic weight loss. If an individual experiences weight loss circumstance before diagnosis and treatment, the likelihood of relapse becomes significantly high. In this study most of the patients lost their body weight. Another finding of this study is that the first time infected patients are more likely to lose weight.
Most of the patients in our study with Multidrug drug resistant and recurrences did not complete the course of anti-TB treatment. Recurrences in patients without curative therapy of their primary TB are expected to be due to reactivations of the same strain, which cannot be assumed to have been eliminated from the organism. It is difficult to explain reinfection in patients in whom primary TB has not been efficiently treated. The strain involved in the first episode may not have been eliminated by therapy, but could have been displaced after competition with the new strain, if the new strain showed higher biological fitness or more efficient interactions with host factors. Another explanation for reinfection in patients who did not adhere to anti-TB therapy could be the occurrence of co-infection with more than 1 strain and the selective growth of different strains for the first and second episodes. (In this study patients having reinfection lose less weight.
Vitamins play very important role in the treatment of tuberculosis. This study shows that, most patients who took vitamin did not get re-infected. Role of folk medicines in the prevention of tuberculosis is still in experimental phase. In this study, we also did not find any remarkable role of folk medicines in the treatment or recurrence of tuberculosis. The population size of this study was limited and further studies are needed to establish our findings more accurately.
7982
References
- Ahsan, G, Ahmed J, Singhasivanon P (2004) Gender difference in treatment seeking behaviours of tuberculosis cases in rural communities of Bangladesh. Southeast Asian Journal of Tropical Medicine and Public Health 35:126-135.
- Vasantha M, Gopi PG, Subramani R (2009) Weight gain in patients with tuberculosis treated under directly observed treatment short-course (DOTS). Indian J Tuberc 56: 5-9.
- Jereb JA (2002) Progressing toward tuberculosis elimination in low-incidence areas of the United States. Recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep 51: 1-14.
- Nair N, Wares F, Sahu S (2010) Tuberculosis in the WHO South-East Asia Region. Bull World Health Organ 88: 164.
- Rahman KA, Kamsrichan W, Keiwkarnka B (2008) Factors Related To Acceptance Of Tuberculosis Case Detection Among Urban Slum Population In Mohammadpur, Dhaka City Corporation, Bangladesh. Journal of Public Health and Development 1: 81-90.
- Banu S, Mahmud AM, Rahman MT, Hossain A, Uddin MK, et al. (2012) Multidrug-resistant tuberculosis in admitted patients at a tertiary referral hospital of Bangladesh. PLoS One 7: e40545.
- (2003) Guidelines for surveillance of drug resistance in tuberculosis. 2nd edn, Geneva: WHO.
- Nationwide tuberculosis prevalence survey in Bangladesh, 2007-2009. ICDDR, B Health and Science Bulletin 8: 4.
- Ganapathy S, Thomas BE, Jawahar MS, Selvi KJ, Sivasubramaniam, et al. (2008) Perceptions of gender and tuberculosis in a south Indian urban community. Indian J Tuberc 55: 9-14.
- Ahsan G, Ahmed J, Singhasivanon P, Kaewkungwal J, Okanurak K, et al. (2004) Gender difference in treatment seeking behaviors of tuberculosis cases in rural communities of Bangladesh. Southeast Asian J Trop Med Public Health 35: 126-135.
- Karim F, Islam MA, Chowdhury AM, Johansson E, Diwan VK (2007) Gender differences in delays in diagnosis and treatment of tuberculosis. Health Policy Plan 22: 329-334.
- Madebo T, Lindtjørn B, Aukrust P, Berge RK (2003) Circulating antioxidants and lipid peroxidation products in untreated tuberculosis patients in Ethiopia. Am J ClinNutr 78: 117-122.
- Rahmatullah M, Jahan R, Azam FM, Hossan S, Mollik MA, et al. (2011) Folk medicinal uses of Verbenaceae family plants in Bangladesh. Afr J Tradit Complement Altern Med 8: 53-65.
- Jahan R, Khatun MA, Nahar N, Jahan FI, Chowdhury AR, et al. (2010) Use of Menispermaceae family plants in folk medicine of Bangladesh.Adv in Nat ApplSci 4: 1-9.
- Vasantha M, Gopi PG, Subramani R (2009) Weight gain in patients with tuberculosis treated under directly observed treatment short-course (DOTS). Indian J Tuberc 56: 5-9.
- Santha T, Garg R, Frieden TR, Chandrasekaran V, Subramani R, et al. (2000) Risk factors associated with default, failure and death among tuberculosis patients treated in a DOTS programme in Tiruvallur District, South India. Int J Tuberc Lung Dis 6: 780-788.