Nahar Alruwaili1*, Ziad N Kazzi2 and Brent Morgan2
1Department of Emergency Medicine, Alfaisal University, Riydah, Saudi Arabia
2Department of Emergency Medicine, Emory University, Georgia Poison Center, Atlanta, Georgia, USA
Corresponding Author:
Nahar Alruwaili
Department of Emergency Medicine, Alfaisal University
Riydah, Saudi Arabia
Tel: 96614424425
Email: nalrowaily@kfshrc.edu.sa
Received date: January 11, 2016; Accepted date: February 24, 2016; Published date: March 3, 2016
Copyright: © 2016 Alruwaili N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Alruwaili N, Kazzi NZ, Morgan B, A Descriptive Cross Sectional Survey of Medical Toxicology Rotations at US Allopathic and Osteopathic Emergency Medicine Residency Programs. Arch Med. 2016, 8:2
Keywords
Medical toxicology; Rotation; Medicine
Introduction
The characteristics of medical toxicology training of United States (US) emergency medicine residents vary between different residency programs [1]. However, medical toxicology is an important component of the emergency medicine curriculum and clinical practice [2,3]. Emergency medicine programs in the United States that are classified as allopathic, osteopathic, or dual (combined allopathic/osteopathic accreditation). These programs teach the core content of emergency medicine using a variety of rotations and educational methods. We describe the current state of medical toxicology rotations US emergency medicine residency programs.
Methods
The study consisted of a cross-sectional survey that was sent electronically to the program directors of US allopathic and osteopathic emergency medicine residency programs that were identified using the Society of Academic Emergency Medicine web portal as well as the American Osteopathic Association web portal [4,5]. Responding residency programs were entered in a raffle to win one of 3 toxicology textbooks that was mailed to them after the completion of the survey data collection. The toxicology rotation was defined as a clinical rotation that involves patient care (bedside, phone consult, or poison center-based) and was categorized as mandatory, offered as an elective, or not offered at all. Mandatory and elective rotations could be offered onsite or at another institution. The study was deemed IRB exempt from review at our institution.
The data was analyzed using the Statistical Package for Social Science (SPSS) version 17.0. The relation between the availability of a mandatory rotation and the type of residency program (allopathic or osteopathic), length of training, and the availability of medical toxicology faculty on staff was analyzed using chi square. This was followed by a binary logistic regression.
Results
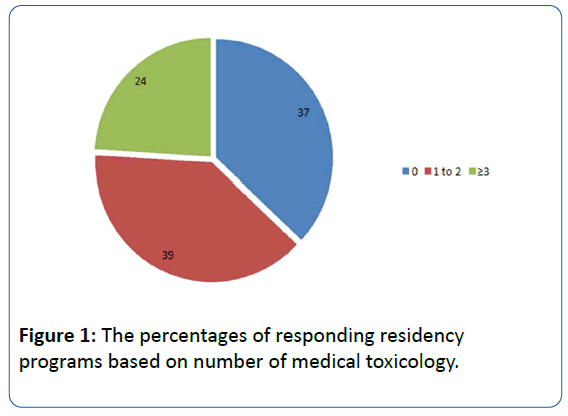
The survey was sent to 197 programs out of which 113 (57%) responded. The responding residencies were composed of 84 (74%) allopathic, 25 (22%) osteopathic and 4 (4%) dual programs. The length of the emergency medicine residency training was 3 years in the majority of respondents (62%) while it was 4 and 2 years in 37% and 1% of respondents respectively. Forty-two (37%) responding programs had no affiliated toxicologists on faculty, while 44 (39%), 23 (20%) and 4 (4%) had 1-2, 3-5 and greater than 5 respectively (Figure 1) faculty on staff.
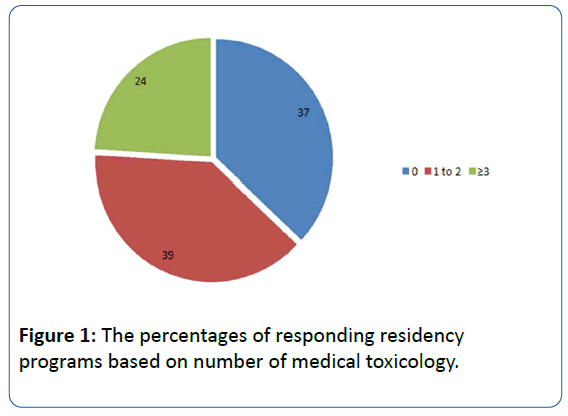
Figure 1: The percentages of responding residency programs based on number of medical toxicology.
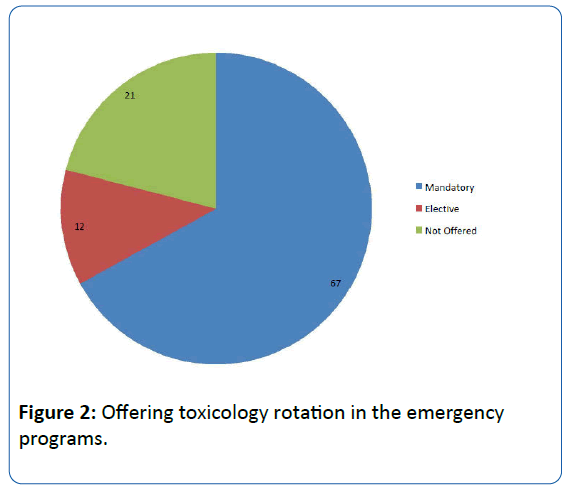
The toxicology rotation was mandatory in 75 (67%) and offered as an elective in 14 (12%) of responding programs. Twenty-four (21%) of responding programs did not offer a toxicology rotation (Figure 2). Among the eighty-nine programs that offer a rotation, 36 (40%) do so onsite while 53 (60%) relied on other institutions to provide the clinical experience.
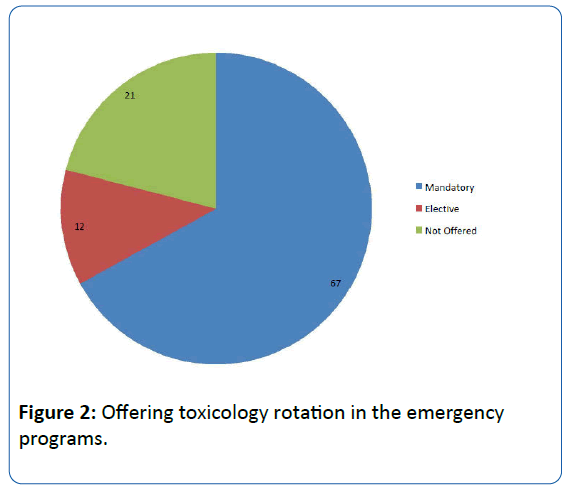
Figure 2: Offering toxicology rotation in the emergency programs.
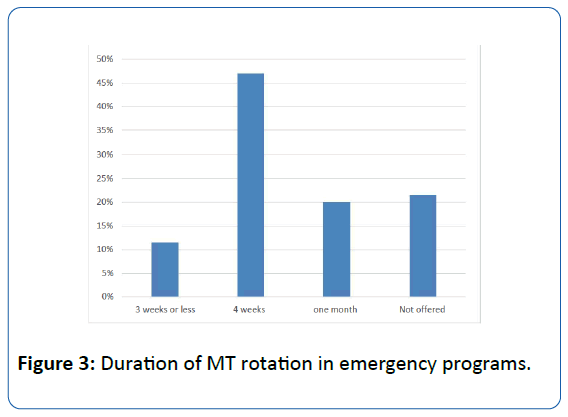
The structure of the rotation varied between programs: 82 (92%) programs had a poison center component while 63 (71%) had a bedside consult service and 51 (57%) had home call duties. The majority of rotations (85%) were 1 month or 4 weeks in length while 23 (15%) of the rotations were 3 weeks or less (Figure 3).
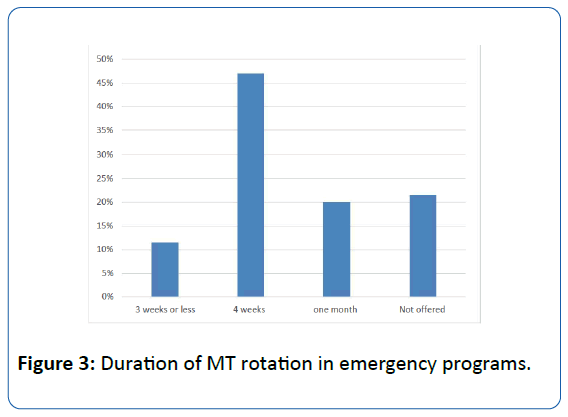
Figure 3: Duration of MT rotation in emergency programs.
Core content medical toxicology lectures were given by affiliated toxicologists in 71 (63%), visiting toxicologists in 41 (36%), and emergency medicine faculty in 67 (59%) of responding programs (the overlap reflects the option to list multiple lecturers). Online lectures were used by 13 (12%) programs and 6 (5%) programs utilized other methods. A vast majority of respondents (94%) were amenable to online educational methods.
A majority of the fourteen programs that responded that they offered an elective rotation (71%) reported that less than 50% of their residents elected to do a toxicology rotation. On other hand, the majority of the twenty-four programs that did not offer a toxicology rotation (88%) allowed their residents to pursue an away rotation on their own.
Regression modeling found that programs with a mandatory rotation were more likely to be longer, 4-5 years in length than programs with an elective rotation or programs that did not offer a rotation. Similarly, programs with a mandatory rotation were more likely to have 1 to 2 medical toxicology faculty members, compared with programs that had an elective or those that did not offer a rotation. Finally, the type of program (osteopathic or allopathic) was not found to affect the toxicology rotation availability (mandatory, elective, or none).
Limitations
The study is limited by the moderate response rate and the inherent problems with survey-based research such as the potential for inaccurate comprehension of the survey questions that can lead to incorrect answers. Programs with toxicology rotations might be more likely to participate suggesting these reported results are ‘best-case’ scenario.
Discussion
In 2000, Hantsche et al. surveyed US emergency medicine residency programs and found, based on a 51% response rate, that a MT rotation was required at 76% of the responding programs, was an elective in 19% and not available at 5% of the programs [1]. Our results, based on a slightly higher response rate, showed a higher percentage of programs that do not offer a medical toxicology clinical rotation during the training (21%). The cause of this apparent increase in the number of programs that do not offer a rotation is unknown and does not seem to be due to a change in the number of available toxicologists on faculty in these programs. Hantsche et al. reported that only 63% of residency programs that responded to his survey had a toxicologist on faculty [1]. This percent appears to be identical to our result (Figure 1). Interestingly, the increase in the number of available toxicology faculty at a program did not appear to increase the number of programs with a mandatory rotation. However, our finding that programs that offered a mandatory rotation were more likely to have 1-2 toxicology faculty can be explained by the fact that the majority of responding programs have 1-2 toxicology faculty (39%) compared with programs that have greater or equal to 3 (29%). On the other hand, the increase in the length of the residency program did appear to increase the number of programs that offer a mandatory rotation. This is likely to be due to the additional year of training that allows for more rotations and electives. Other factors that can explain the decrease in mandatory and elective toxicology rotations reported in our study include the introduction of other rotations such as emergency ultrasound and administration that compete with regards to time allotments.
Furthermore, the structure of toxicology rotations varies greatly: a majority of programs have offsite rotations and a large majority of programs have a poison center component. In contrast, a bedside clinical consult or home-call components were present in a relatively lower percentage of programs. Dependence on a poison center may not be an optimal design because there are only 57 poison centers in the United States and their resources are currently challenged by funding cuts. Additionally, off site rotations are difficult due to funding issues and Accreditation Council of Graduate Medical Education (ACGME) duty hours and rotation requirements. A uniformly structured medical toxicology rotation could be advantageous and could be created through collaboration between emergency medicine and medical toxicology specialty organizations.
In a similar manner, medical toxicology lectures are delivered primary by a variety of specialists including affiliated or visiting medical toxicologists and emergency medicine faculty. A relatively small percentage of programs utilize online lectures even though a majority of programs stated they were agreeable to utilizing online tools. In view of the lack of sufficient number of medical toxicologists at emergency medicine training programs, training curricula should include a high quality and comprehensive online education component composed of audiovisual modules, reading materials, interactive case-studies as well as pre-tests and post-tests to evaluate the students.
Conclusion
Our study revealed heterogeneity in the structure of MT training in US emergency medicine training programs. The proportion of programs not offering a MT rotation appears to have increased over the past decades. A majority of programs which offer a MT rotation do so at a poison center. While longer programs are more likely to have a MT rotation, the presence of extra MT faculty does not change that figure. The wide variation in MT educational formats combined with the current uncertainties in poison centers’ funding makes the idea of a national MT, computer-based learning instrument interesting.
9126
References
- Hantsche CE, Mullins ME, Pledger D, Bexdicek KM (2000) Medical toxicology experience during emergency medicine residency. AcadEmerg Med7:1170.
- Hockberger RS, Binder LS, Chisholm CD, Cushman JT, Hayden SR, et al. (2005) The model of the clinical practice of emergency medicine: a 2-year update. Ann Emerg Med 45:659-674.