Keywords
Bangladesh; 5S-KAIZEN-TQM approach; Hospital; Maternal and newborn health; PDCA cycle; Quality improvement system
Abbreviations
CIPRB: Centre for Injury Prevention and Research; Bangladesh; DGHS: Directorate General of Health Services; DGFP: Directorate General of Family Planning; 5S: Sort-set-shine-sustain-standardize; HNPSP: Health Nutrition and Population Sector Program; U5MR: Under-five mortality rate; MCWC: Maternal and Child Welfare Centre; MDGs: Millennium Development; MNH: Maternal and Newborn Health; PDCA: Plan-Do-Check-Act;
QA: Quality Assurance; QI: Quality Improvement; TQT: Total Quality Management; UN: United Nations;
WHO: World Health Organization
Introduction
Bangladesh is one of the 61 countries with high under-five mortality rate (U5MR) which has already achieved the target of Millennium Development Goal 4 (MDG-4) by reducing two thirds of U5MR between 1990 and 2015. However, neonatal death is still high (28 death per 1000 live births) and it is 61 percent among all under-5 child deaths [1]. The maternal mortality ratio declined from 550 to 170 per 100,000 live births between 1990 and 2013 in Bangladesh. However, this ratio needs to decline further to 143 per 100,000 live births to achieve the target for the Millennium Development Goal 5 (MDG -5) [2].
Although Bangladesh achieved the target MDG-4 and on the track of achieving MDG-5 target, however, the mortality rates, both maternal and under-five children including neonates, are still high in Bangladesh in comparison to developed countries [3,4]. Like other low and middle income countries poor maternal, newborn and child health care remain significant problems in Bangladesh [5].
Bangladesh government has a unique health infrastructure comprises of six tiers namely national, divisional, district, upazila (sub-district), union, and ward [6,7]. District and subdistrict level hospitals play a fundamental role for maternal and newborn health (MNH) services. The sub-district and district level health facilities are primary and secondary level hospitals respectively. From a sub-district hospital patients are referred to a district hospital which provides specialist services in medicine, surgery, obstetrics and gynaecology, newborn and paediatrics, clinical pathology, blood transfusion, and laboratories [8,9]. However, several studies showed that the quality of the health facilities in all six tiers of Bangladesh is not up-to the mark [10,11]. From the evaluation of the Health Nutrition and Population Sector Program (HNPSP) it is evident that the Government of Bangladesh is committed to provide quality health care including MNH care services [12].
To improve the quality of current MNH care, it is essential to establish a quality improvement (QI) system, which is almost non-existent in Bangladesh. Considering the country context the successful models of the high-income-countries could not be implemented in a country like Bangladesh. Therefore, it was crucial to develop a QI model and find out a feasible strategy for implementation which could contribute in reducing maternal and newborn mortality in Bangladesh.
The objective of this paper is to describe the method of developing the QI model and its implementation strategy for MNH services applicable for district (District Hospitals and Maternal and Child Welfare Centre) and sub-district level hospitals (Upazila Health Complexes) in Bangladesh.
Methods
The “Model QI System” and its implementation process were developed through a-five step process. The nationally agreed and recommended mechanism for quality improvement and best practices were considered in all steps of development. Through series of national level consultative workshops the “Model QI System” and its implementation process were gradually finalized. The methods employed to develop the QI model system and its implementation process were as follows: 1. reviewing of evidence based literature, country experience and base line QI survey report [9]; 2. drafting implementation framework, guidelines and tools through consultative process participated by national experts; 3. field testing of the “Model QI System” including implementation framework, guidelines and tools at district, sub-district level hospitals and local level workshops; 4. updating of the model including its implementation framework, guidelines and tools based on the feedback from the health care providers of districts and sub-district level hospitals; and 5. reviewing and updating the “Model QI System”, its implementation framework, guidelines and tools by national level stakeholders and professional experts at national level workshops and approval of the Directorate General of Health Services (DGHS) for piloting in 14 government hospitals of two districts.
Step 1: Reviewing of evidence based literature, country experience and base line QI survey report
The researchers identified relevant documents and articles from journals through electronic search to review evidence based literature related to quality improvement of health services of developed and developing countries. They also contacted with the relevant government and non-government health officials to collect various gray literatures and documents where the experiences on quality improvement of health services of Bangladesh described [13-38]. The base line survey report titled “Baseline assessment for introducing quality improvement system in MNH services in facilities of Thakurgaon and Jamalpur districts of Bangladesh” which was conducted by the Centre for Injury Prevention and Research, Bangladesh (CIPRB) was also used. All these information was recorded in a pre-designed review document. The document was then provided to the national workshop participants, who were experts on the relevant field, prior to workshop. The workshop participants were the researchers, national professionals related to MNH services (paediatricians, gynaecologists and anesthesiologists), the health programmers and administrators of the Directorate General of Health Services and Directorate General of Family Planning, Bangladesh. Each participant was instructed to identify the components of QI systems and its implementation framework. They were also requested to identify the principles and standards for implementation of the QI system through its framework.
Step 2: Drafting implementation framework, guidelines and tools through consultative process participated by national experts
Through series of workshops by utilizing the findings from the review documents and considering the country context, socioeconomic and cultural context of the service recipients, availability of resources including service providers, capacity of the hospitals and patient load the workshop participants drafted the model QI system including implementation framework, guidelines and tools. Each workshop progressed based on the decision of the previous workshop.
Step 3: Field testing of the “Model QI System” including implementation framework, guidelines and tools at district, sub-district level hospitals and local level workshops
The researchers shared the draft “Model QI System” and the implementation framework, guidelines and tools with the local health managers and health care providers including consultants, medical officers, nursing in-charge and ward masters related to MNH care services of the 14 selected hospitals in Thakurgaon and Jamalpur districts where the baseline survey was conducted [9]. After sharing the draft “Model QI System”, the field testing was conducted in two districts and four sub-district level hospitals of the surveyed areas to assess the acceptability and feasibility of the QI system. The feedback of the health care providers was accumulated through local level workshops.
Step 4: Updating of the model including its implementation framework, guidelines and tools based on the feedback from the health care providers of districts and sub-district level hospitals
The researchers updated all the components of the “Model QI System” including its implementation framework, guidelines and tools by incorporating the findings and feedbacks received from the field level managers and health care providers during field testing.
Step 5: Reviewing and updating the “Model QI System”, its implementation framework, guidelines and tools by national level stakeholders and professional experts at national level workshops and approval of the Directorate General of Health Services (DGHS) for piloting in two districts3
Areas needed adjustment, and modifications were done by the national level workshop participants and the researchers.
The field tested “Model QI System” was finalized at a national level consensus meeting with a high-level technical committee comprised of academicians, programme personnel from Directorate General of Health Services (DGHS) and Directorate General of Family Planning (DGFP), Bangladesh, representatives from professional bodies, subject specialists, representatives from UN agencies and researchers from CIPRB. The Directorate General of Health Services, Bangladesh approved the “Model QI System” to pilot in 14 district and sub-district level government hospitals of Thakurgaon and Jamalpur districts where the base line survey was done to assess the quality of MNH services of hospitals in 2011.
This study was conducted from May 2012 to October 2012.
Ethical Issues
The Ethical Review Committee of the Centre for Injury Prevention and Research, Bangladesh (CIPRB) approved the study.
Results
Through documents review, series of workshops and national level consensus meeting an adapted “Model QI System” was developed. The developed model consists of three elements namely: 1) QI implementation framework; 2) QI implementation guidelines; and 3) Tools for QI framework implementation.
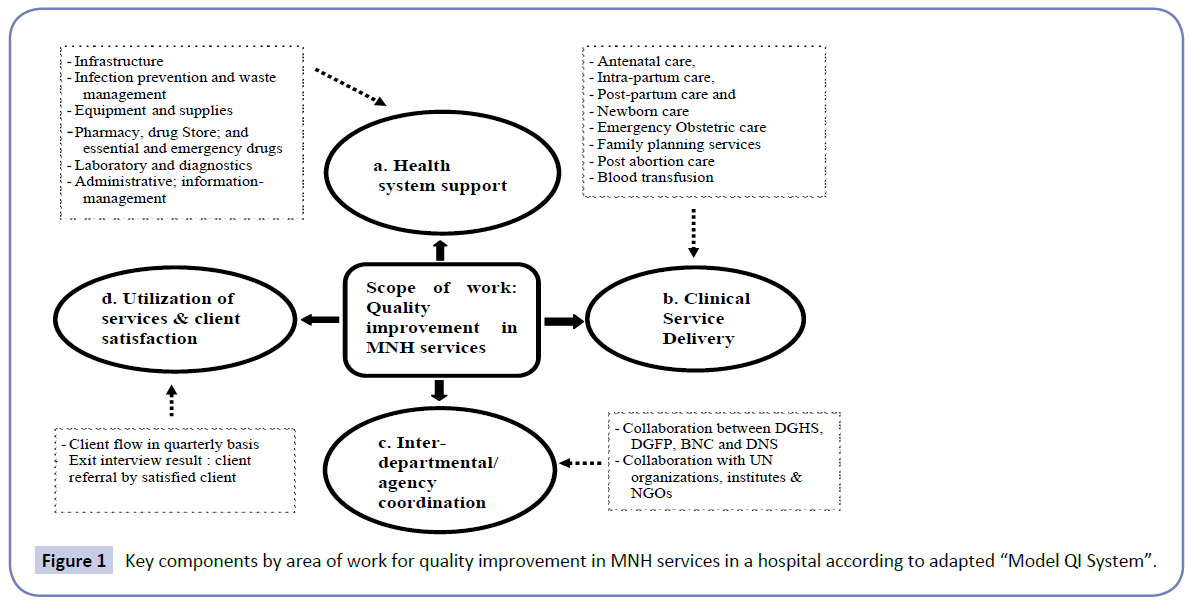
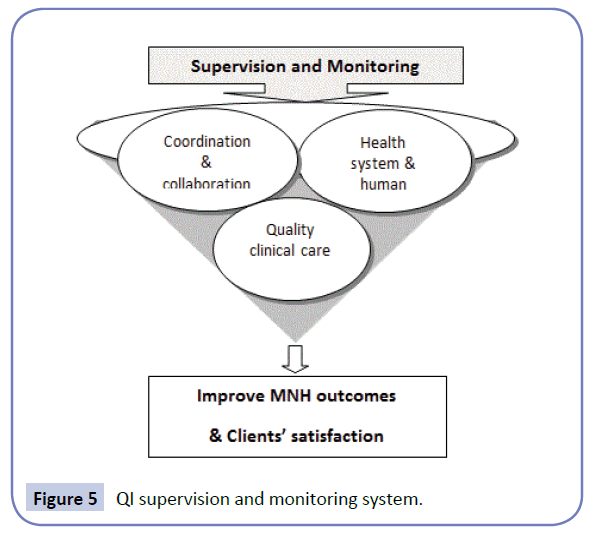
The workshop participants and national consensus meeting members conceived the model considering the continuous capacity-building based on concept of six building blocks of a health system described by WHO which included i) service delivery; ii) health workforce; iii) information; iv) medical products, vaccines and technologies; v) financing; and vi) leadership and governance (stewardship). According to WHO building blocks, health system works for quality improvement through building facility readiness, and providers’ skill improvement, and coordinated actions. Series of consultations held with experts at national and sub national level to identify the key areas of work and the components for quality improvement in MNH services. Based on the WHO building blocks concept the following key components by area of work for quality improvement in MNH services in a hospital were considered: health system support, clinical service delivery, inter-department/agency coordination and utilization of services and client satisfaction (Figure 1). The groups agreed on strengthening of health system components (Figure 1a) to ensure availability and accessibility of equitable, safe and effective MNH care service. The components for site assessment and strengthening of hospitals were adapted from the evidence based and agreed through consensus. Similarly, the clinical standards for necessary clinical care were also identified from National and internationally agreed Standard Operating Procedures under the clinical service component (Figure 1b). As reflected in the objectives, the QI process had also taken in cognizance to stronger coordination and collaboration among actors by level (Figure 1C) aiming at improving quality of care and attaining maximum client satisfaction (Figure 1d).
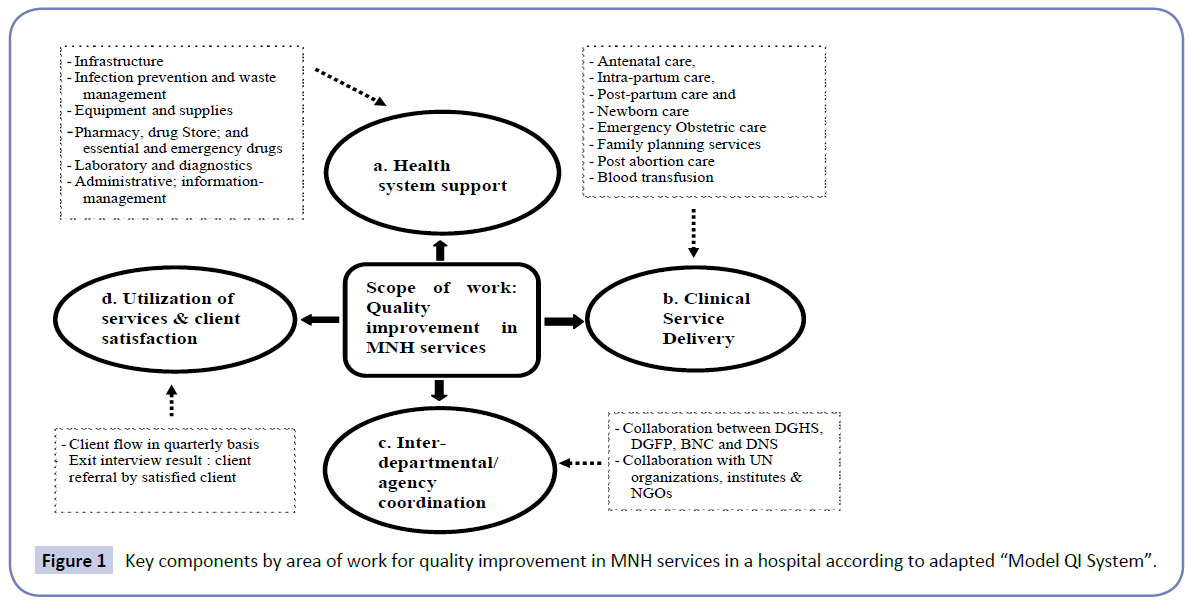
Figure 1: Key components by area of work for quality improvement in MNH services in a hospital according to adapted “Model QI System”.
QI implementation framework
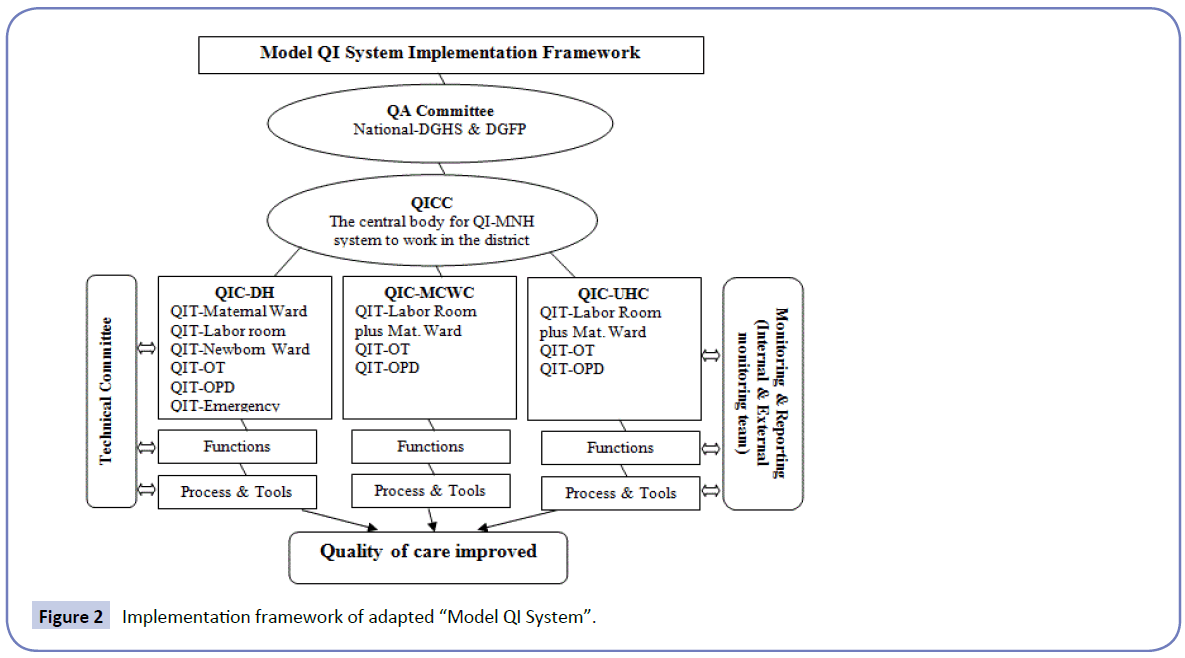
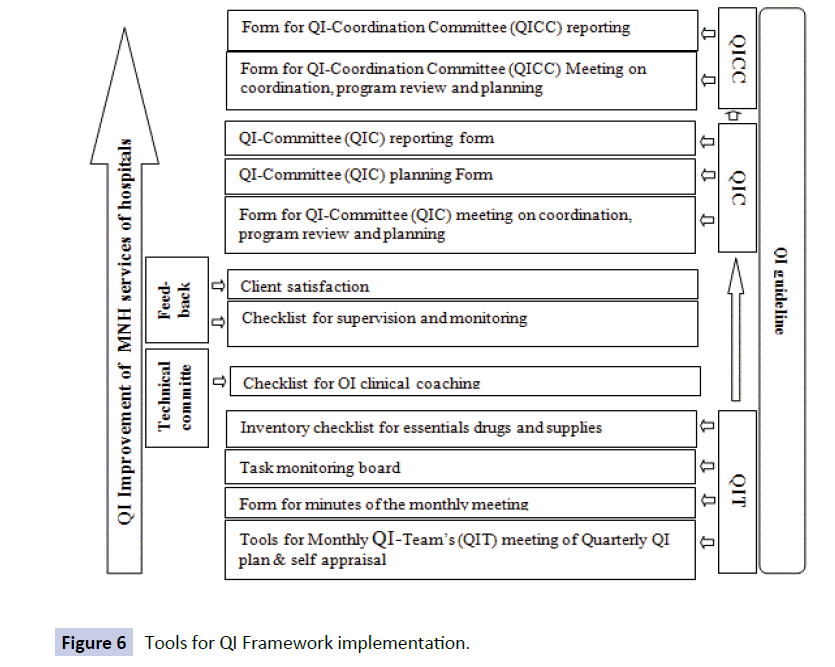
An implementation framework (Figure 2) for the adapted “Model QI System” was formulated and agreed through series of workshops at national and sub-national level. Quality Assurance (QA) Committee established by the Ministry of Health and Family Welfare of the Government of Bangladesh would act as the top level body for coordination, policy support and guidance. For effective implementation of QI process, one QI-Coordination Committee was formed per district to supervise, guide and monitor QI activities in all hospitals under the specified district. One QI-Committee for each hospital and necessary numbers of QI-Teams by key areas of MNH care (like maternity ward, labour room, operation theater, newborn ward etc.) were formed in each hospital with defined composition, roles, responsibilities and functions.
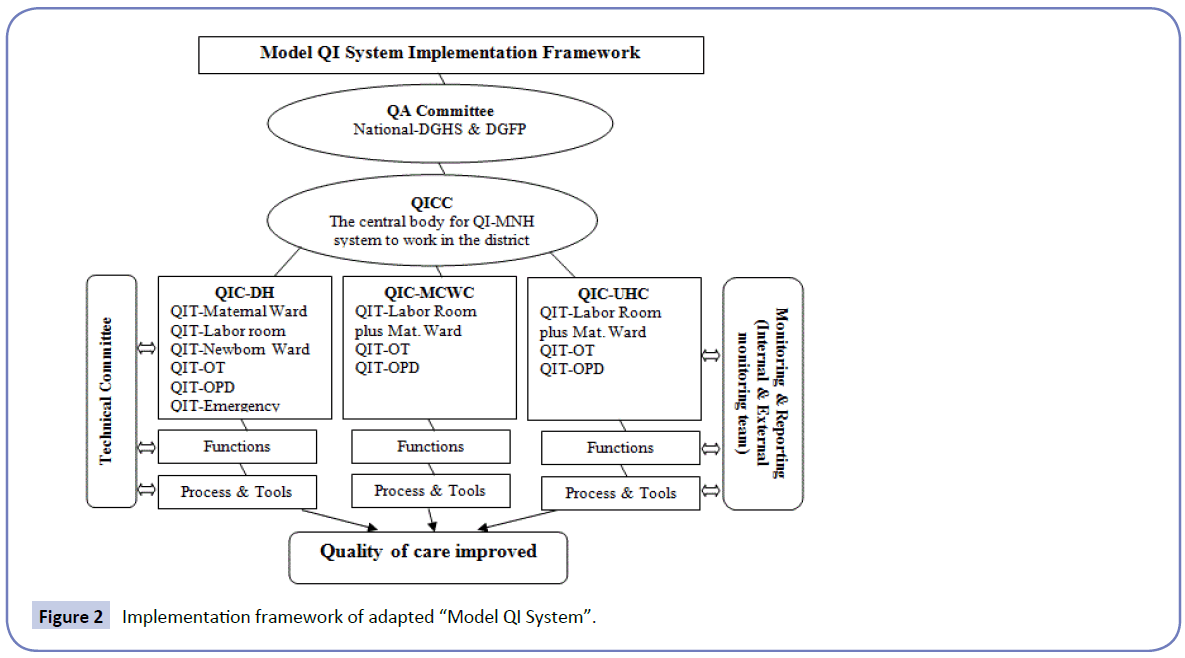
Figure 2: Implementation framework of adapted “Model QI System”.
Partnership was established with peripheral medical institutes/ medical colleges and professional organizations to support technical supervision and monitoring (through technical committee). To depict progress, gaps and challenges in service delivery in regards to health system support, human resource management, ensuring evidence based clinical practices; a vertical supportive supervision and monitoring system (through external and internal monitoring team) were integrated within the QI implementation system. The framework is illustrated in Figure 2.
The whole QI implementation process would follow an evidence based participatory problem-solving mechanism leading to the final stage of total quality management (TQM) through bottom up approach. The QI guideline also includes a clear description of the roles and responsibilities of each teams and members. The QI-Teams of different levels would work by following the agreed principles which was developed on the basis of social and cultural contexts of Bangladesh, availability of human and non-human resources and policy directions (Table 1).
| Improving MNH services with available resources through maximizing utilization. |
| Creating enabling environment to improve clinical services. |
| Focusing very few but vital things |
| Prioritizing doable changes for sustainability |
| Keeping relevance with selected focus areas. |
| Team approach. |
| Relying on local leadership |
| Participatory problem solving and relying on support staff for quality improvement responsibilities. |
Table 1 Key Principles for implementation.
During implementation, the district level QI-Coordination Committee would act as the central body for coordination and control of the QI-system. This committee would be convened by the Civil Surgeon and Co-Chaired by Deputy Director of Family Planning of each district. The health managers of the district and sub-district level hospitals would be the members of the committee. Below the QI-Coordination Committee, each hospital would have a QI-Committee and several quality improvement teams for MNH services. Each QI-Committee would be chaired by the top hospital manager and consultants would be the members of the committee. On the other hand each QI-Team would be formed by the doctors, nurse and support staff working in specific area and focal person would be the Nurse in-charge of the respective wards.
QI-Teams would be the basic unit of QI-system and perform all related activities while QI-Committees would monitor and supervise the functions of QI-Teams. The uniqueness of these QITeams was presence of nurses as focal person to lead all activities.
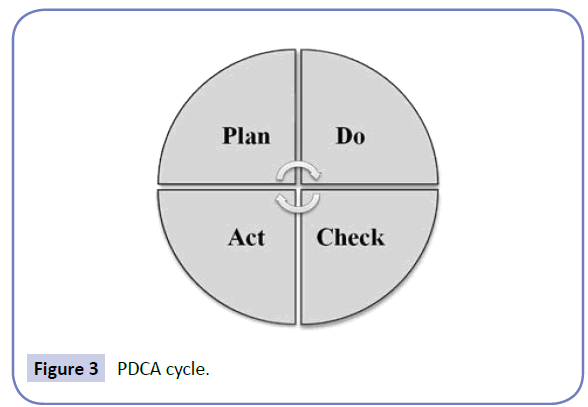
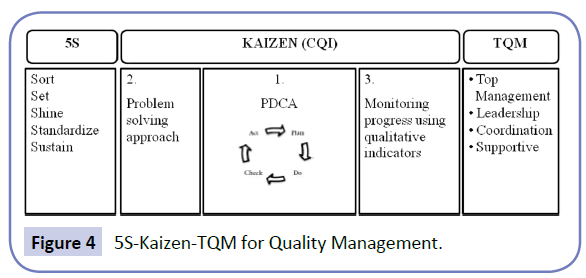
The QI-Teams followed problem solving participatory approaches namely PDCA cycle (Figure 3) and 5S-KAIZEN-TQM approach (Figure 4) for continued quality improvement of the areas. 5S concept (Sort-Set-Shine-Standardize-Sustain) of QI process would be utilized in improving work environment.
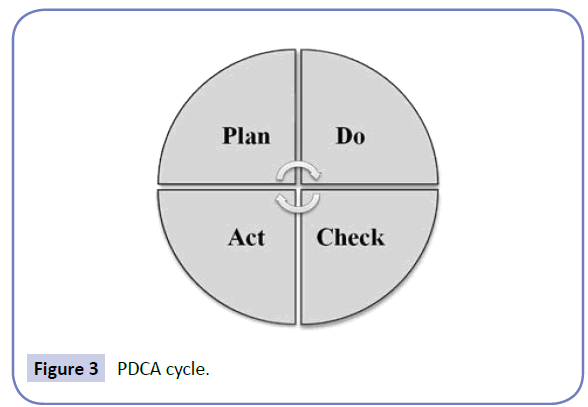
Figure 3: PDCA cycle.
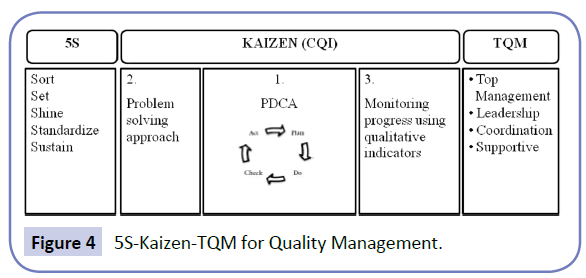
Figure 4: 5S-Kaizen-TQM for Quality Management.
The supervision and monitoring system for this “Model QI System” was developed in such a way, so that from the national to local level, every related person would able to contribute in this quality improvement process (Figure 5).
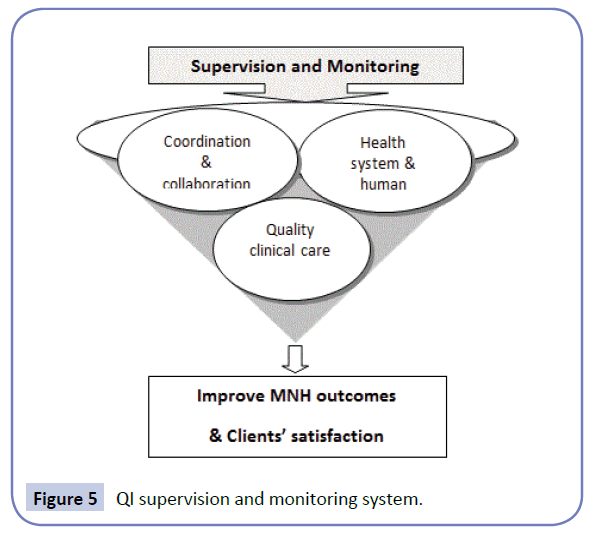
Figure 5: QI supervision and monitoring system.
Directorate General of Health Services (DGHS) and Directorate General of Family Planning (DGFP), Bangladesh and members of QI-Coordination Committee, QI-Committees and QI-Teams would directly be involved in supervision and monitoring process. Constant and close supervision and monitoring would be accomplished through external and internal monitoring teams. Subject specific experts like obstetricians and paediatricians from medical college hospitals would be engaged in periodic clinical monitoring at hospitals and provided simultaneous clinical coaching to the care providers on the spot. Client satisfaction was also considered as one of the important monitoring indicators.
Tools for QI framework implementation and the mechanisms of its utilization
Different types of tools were developed for QI-Teams, QICommittees, QI-Coordination Committees, Technical Committees, External and Internal Supervision and Monitoring Committees and tools for assessment of client satisfaction which would be utilized by following the QI implementation guidelines (Figure 6).
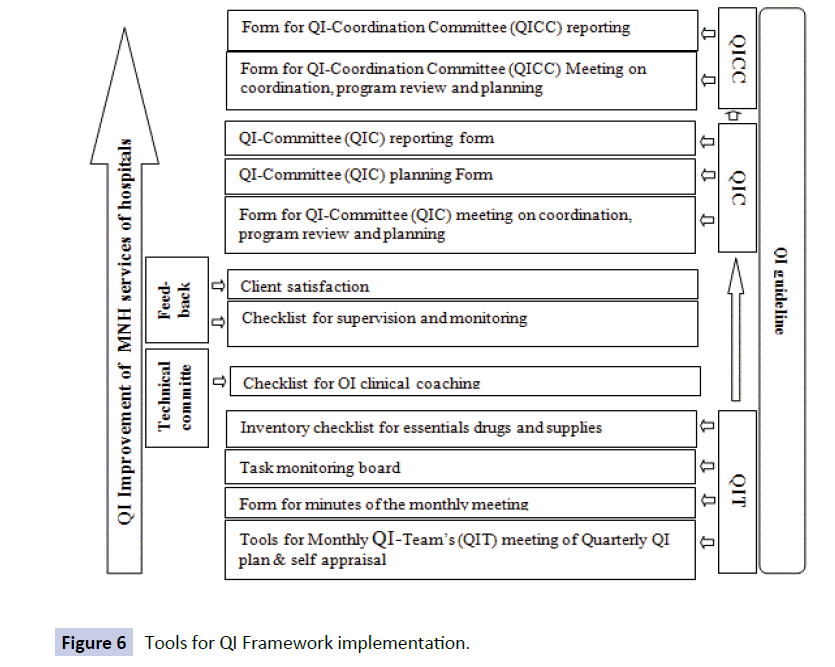
Figure 6: Tools for QI Framework implementation.
According to the developed guidelines the QI-Team members would utilize the tools by following a definite process to operate in cyclic order following plan-do-check-act (PDCA cycle) approach. The members of this team would sit for routine monthly meeting with a set agenda and would go for specific decisions to be accomplished within time frame. The QI-Committee of hospitals would supervise all activities under QI implementation process and would remain reportable to District QI-Coordination Committee. Once in a quarter the QI-Committee would organize a planning and progress review meeting based on problems noticed by QI-Teams to identify the solutions. This committee would take administrative actions needed for QI activities and provide necessary feedback and guidance to QI-Teams of the hospitals. Finally, the QI-Coordination Committee would report to National level. Tools for supervision and monitoring for different tiers were developed in such a way that supervision would be supportive; while monitoring system would function to illustrate progress, gaps and challenges in service delivery in regards to health system support, human resource management, ensuring that the evidence based clinical practices would be applied during clinical care.
Discussion
Through document reviews, baseline survey and workshops and national consensus meeting a “Model QI System” with its implementation framework, guidelines and tools were developed.
Improve the quality of care of health hospitals is a never ending journey. Although it is a subjective, changeable, multifaceted and multi-dimensional concept, however always depends on time and place. Quality of care of hospitals is one of the most vital issues to reduce maternal and newborn morbidity and mortality of Bangladesh [11]. Although there were challenges to choose the definition of QI appropriate for the model QI system, however the experts adopted the definition for our model from the following definitions defined by the US Agency for Healthcare Research and Quality: “doing the right thing to the right person at the right time at the lowest cost” and Avedis Donabedian’s definition about quality of care “that kind of care which is expected to maximize an inclusive measure of patient welfare, after one has taken account the balance of expected gains and losses that attend the process of care in all its parts” [29,30]. Keeping in mind the socio-cultural and economic context of Bangladesh, this QI-MNH system for hospital is developed by modifying those two definitions with 5S-KAIZEN-TQM approach along with PDCA cycle [37].
The current model will be applied in district and sub-district level government hospitals of Bangladesh to improve the quality of MNH care with special attention to HCPs needs and clients satisfaction. This “Model QI System” will work with the following characteristics which will be the key to success of quality improvement: efficiency, efficacy, effectiveness, equity, accessibility, comprehensiveness and acceptability.
Similar to our article, Linsk et al. described in their report about the process development of a quality improvement project to evaluate Ryan White CARE act HIV/AIDS services which has been provided primary care and social support to the people with HIV/ AIDS countrywide in USA since 1990 [39]. In this project they developed guidelines and identified the mechanism to improve the quality of services. The methodological approaches to develop the guidelines and mechanism to improve the service quality were found different from our study. However, the article described the process of development.
Utilizing a similar QI implementation framework at a county hospital and a university hospital of Sweden showed improvement in health care especially in team work among the physicians and patient safety [40]. We have assessed the clients’ needs and satisfaction level before developing the QI system so that the QI system can address the problems properly. There are some intervention studies where the patients’ needs were identified first before structuring a QI intervention package, addressed those findings and implemented. The findings of those studies show that the satisfaction level of the clients increased significantly compared with the base line survey [41].
Asian countries like Bangladesh, Laos and Cambodia often fight with inadequate human resource, shortage of supplies along with the inadequate access to necessary medicines and technologies which resulted a compromise with the quality of care [9,42,43]. However, many of the Asian countries addressed the quality issues by adopting the 5S-KAIZEN-TQM approaches successfully [39,44]. Not only the Asian countries but also the African countries experienced different types of approaches of QI programs to improve quality of health facility care. Although, there were lots of challenges during implementation of these QI approaches, however, the evaluation showed the achievements in improving quality of care [45]. Therefore, we expect that the developed ‘Model QI System” will lead to improve quality of the MNH- services of the hospitals in Bangladesh.
The limitation of the study was that the QI system was developed to implement in district and sub-district hospitals only and it may not be applicable for the tertiary level of hospitals of Bangladesh. This “Model QI System” relies on the human behavior of accomplishing the whole QI process. Therefore, it is unpredictable whether the human resources related to implementation of the process would act as expected. However, to address this issue there is a provision of rewards for the concern persons.
Conclusions
Through document reviews, baseline survey and workshops an adapted “Model QI System” was developed to improve the quality of MNH services of the government hospitals in Bangladesh. Similar types of QI systems are in operations in several countries of Asia and Africa and found effective in improving the quality of care. Therefore, it is expected that the developed “Model QI System” will also be effective to improve the quality of MNH care services of district and sub-district hospitals in Bangladesh.
Authors’ contributions
Farzana Islam has active involvement in generating the concept of the study, drawing the methodology and implementation of the study with Aminur Rahman, Abdul Halim, AKM Fazlur Rahman and Koustuv Dalal. Farzana has coordinated the whole program and planned how to describe the whole process of developing the model for MNH quality improvement system in the paper. She has written the manuscript under the supervision of Fazlur Rahman, Aminur Rahman, Abdul Halim, Charli Eriksson and Koustuv Dalal.
Acknowledgments
We thank WHO-Bangladesh, the Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People’s Republic Bangladesh, the Civil Surgeons and Deputy Directors of Family Planning in Jamalpur and Thakurgaon districts, the healthcare facility managers, service providers, and their clients for their support in the study. We also thank the professional experts including programmers, gynecologists, pediatricians and anesthesiologists who participated in the workshops for developing the “Model QI system”. We gratefully acknowledge Col. AHM Kamal (Retd) for editing the English language of the manuscript.
Funding
The project was funded by World Health Organization.
Competing and conflicting Interests
The authors declare that they have no competing interests.
8813
References
- National Institute of Population Research and Training (NIPORT) (2015) Bangladesh demographic and health survey 2014 key indicators. NIPORT: Dhaka, Bangladesh.
- El Arifeen S, Hill K, Ahsan KZ, Jamil K, Nahar Q, et al. (2014) Maternal mortality in Bangladesh: a Countdown to 2015 country case study. Lancet 384: 1366-1374.
- WHO (2013) Level and trends in child mortality: report Estimates Developed by the UN Inter-agency group for child mortality estimation. Geneva, Switzerland: World Health Organization.
- Zere E, Suehiro Y, Arifeen A, Moonesinghe L, Chanda SK, et al. (2013) Equity in reproductive and maternal health services in Bangladesh. Int J Equity Health 12: 90.
- Lassi ZS, Salam RA, Das JK, Bhutta ZA (2014) Essential interventions for maternal, newborn and child health: background and methodology. Reproductive Health 11: S1.
- Rahman RM (2006) Human rights, health and the state in Bangladesh. BMC Int Health Hum Rights 6: 4.
- Islam MS (2009) People’s Participation in Health Services: a study of Bangladesh’s rural health
- Salam RA, Lassi ZS, Das JK, Bhutta ZA (2014) Evidence from district level inputs to improve quality of care for maternal and newborn health: interventions and findings. Reproductive Health 11: S3.
- Islam F, Rahman A, Halim A, Eriksson C, Rahman F, et al. (2015) Perceptions of health care providers and patients on quality of care in maternal and neonatal health in fourteen Bangladesh government healthcare facilities: a mixed-method study. BMC Health Services Research 15: 237.
- Akter MS, Upal M, Hani U (2008) Service quality perception and satisfaction: a study over sub-urban hospitals in Bangladesh. Journal of Services Research.
- Bangladesh Health, Nutrition and Population Sector Program (HNPSP) (2009) Annual program review (APR).Volume 1. Main consolidated report. Independent review team (IRT).
- WHO (2009) Making Pregnancy Safer: Assessment Tool for the Quality of Hospital Care for Mothers and Newborn Babies, Copenhagen, WHO Regional Office for Europe.
- (2003) Essential Service Package: A Practical Guide for Quality Service Delivery, Client and Provider’s Perspective, BPHC Public NGO Partnership, 3rd edition (draft). Dhaka, Bangladesh.
- Shaw C (2003) How Can Hospital Performance be Measured and Monitored? Copenhagen, WHO Regional Office for Europe (Health Evidence Network Synthesis Report on Hospital Performance.
- (2000) Improving Providers Skills: A discussion paper on Strategies for Assisting Health Workers to Modify and Improve Skills: Developing Quality Health Care- A process of Change. Geneva, Switzerland: WHO.
- (2003) Using Performance and Quality Improvement to Strengthen Skilled Attendance. Baltimore, Maryland, USA: JPIEGO.
- (2004) Site Assessment and Strengthening for Maternal and Newborn Health Programmes. Baltimore, Maryland, USA.
- (2005) Standard-based Management and Recognition: A Field Guide A Practical Approach for Improving the Performance and Quality of Health Services. Baltimore, Maryland, USA.
- (2001) Engender Health’s Quality Improvement Series: COPE for Maternal Health Services- A Process and Tools for Improving the Quality of Maternal Health Services. New York, USA.
- (2003) EngenderHealth’s Quality Improvement Series: COPE a Process for Improving Quality in Health Services. New York, USA.
- WHO (2007) Recommended Interventions for Improving Maternal and Newborn Health, Department of Making Pregnancy Safer. Geneva, Switzerland.
- (2006) Quality of Obstetric Care Observed in 14 Hospitals in Benin, Ecuador, Jamaica and Rwanda: Quality Assurance Project. USAID.
- Chowdhury S, Hossain SA, Halim A (2009) Assessment of quality of care in maternal and newborn health services available in public health care facilities in Bangladesh. Bangladesh Med Res Counc Bull 35: 53-56.
- (2001) The Measure Evaluation Bulletin. Monitoring the Quality of Care in Family Planning. Number 1.
- Martinez J (2001) Assessing Quality, Outcome and Performance Management. Report on the Global Workforce Strategy. Geneva, Switzerland: WHO.
- (2001) Implementing Global Maternal and Neonatal Health Standards of Care. Baltimore, Maryland, USA: JPIEGO;
- Quality Assessment and Improvement Manual: Maternal and Neonatal Health Services in District Hospitals: Developed by Obstetrical and Gynaecological Society of Bangladesh in 2010 and approved by DGHS and DGFP, Bangladesh.
- 2004) Site Assessment and Strengthening for Maternal and Newborn Health Programmes. Baltimore, Maryland, USA.
- Donabedian A (1980) The Definition of Quality and Approaches of its Assessment. Volume 1: Explorations in Quality Assessment and Monitoring. Ann Arbor, MI. Health Administration Press.
- Bruce J (1990) Fundamental elements of the quality of care: a simple framework. Stud FamPlann 21: 61-91.
- World Health Organization (2007) Everybody business: strengthening health systems to improve health outcomes : WHO’s framework for action. Geneva, Switzerland.
- World Health Organization (2010) Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland.
- World Health Organization (2006) Quality of care: a process for making strategic choices in health systems 9-10.
- Bangladesh Health Population & Nutrition Sector Development Programme (HPNSDP) (2011-2016). Program implementation plan (PIP). Volume 1. Planning Wing, Ministry of Health and Family Welfare Government of the People’s Republic of Bangladesh: Bangladesh.
- World Health Organization (2006) Integrated Management of Pregnancy and Childbirth (IMPAC).
- Ferlie EB, Shortell SM (2001) Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 79: 281-315.
- Varkey P, Reller MK, Resar RK (2007) Basics of quality improvement in health care. Mayo ClinProc 82: 735-739.
- Sokovic M, Pavletic D, Pipan KK (2010) Quality Improvement Methodologies – PDCA Cycle, RADAR Matrix, DMAIC and DFSS. Journal of Achievements in Materials and Manufacturing Engineering 43:476-483.
- Withanachchi N, Karandagoda W, Handa Y (2004) A performance improvement programme at a public hospital in Sri Lanka: an introduction. J Health Organ Manag 18: 361-369.
- Linsk NL, Bruce D, Schechtman B, Warnecke R, Tunney K, et al. (2005) Development and implementation of a quality improvement program for Ryan White Title I care services using a stakeholder-based model. AIDS Patient Care STDS 19: 174-185.
- Burstrom L, Letterstal Anna, Engstrom ML, Berglund A, Enlund M. The patient safety culture as perceived by staff at two different emergency departments before and after introducing a flow-oriented working model with team triage and lean principles: a repeated cross-sectional study. BMC Health Services Research. 2014;14:296
- Mehta RH, Montoye CK, Gallogly M, Baker P, Blount A, et al. (2002) Improving quality of care for acute myocardial infarction: The Guidelines Applied in Practice (GAP) Initiative. JAMA 287: 1269-1276.
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH (2004) Improving the quality of health care for chronic conditions. QualSaf Health Care 13: 299-305.
- Hanvoravongchai P, Chavez I, Rudge JW, Touch S, Putthasri W, et al. (2012) An analysis of health system resources in relation to pandemic response capacity in the Greater Mekong Subregion. International Journal of Health Geographics11: 53.