Key words
Type 2 Diabetes Mellitus, sub-clinical hypothyroidism, hyperthyroidism.
Introduction
Among all the endocrinal metabolic diseases, Diabetes Mellitus is the most common disorder seen. The impact of this disease on the quality of life, and on morbidity and mortality through the complications that affect the small and large vessels resulting in retinopathy, nephropathy, neuropathy, IHD, and large vessel obstruction has been emphasized by the findings of the national commission (USA) on diabetes and DCCT trial.
Diabetes being the most common endocrine metabolic disorder, there was curiosity to understand and learn the association of this with another common endocrine gland function that is thyroid gland.
The association between these two disorders has long been recognized although the prevalence of thyroid dysfunction in diabetic population varies widely between studies. With insulin and thyroid hormone being intimately involved in cellular metabolism and thus excess or deficit of these hormones result in functional derangement of the other. Enhanced sensitivity and specificity of TSH has greatly enhanced assessment of thyroid functions.
There are numerous lines of evidence to suggest that Type 1 DM is a autoimmune disorder. These include the presence of insulitis, presence of antibodies, auto-reactive T- cell’s against islet antigens, an association with some other known organ specific autoimmune diseases (thyroid disorders and pernicious anemia) and a strong association between HLA genes and lastly remission of the disease with immune-modulator therapy. Thus association between thyroid and Type 1 diabetics may be a auto- immune process.
Association of poorly controlled diabetes and thyroid results in a low T3 state and loss of TSH response to TRH. Regardless of glycemic control there is an absence of nocturnal THS peak.
The aim of this study is to establish the relationship between the diabetes and thyroid dysfunction probably affected as a consequence to the auto immune pathology. The thyroid dysfunction was assessed on the basis of clinical findings and laboratory estimation of serum T3 and T4 and TSH levels and structural disturbances were made out by FNAC of thyroid gland. The present study was taken up to note the prevalence of thyroid dysfunction in Type 2 diabetics and spectrum of thyroid dysfunction.
Aims and objectives of the study
1) To study the thyroid functions in diabetes mellitus.
2) To know the spectrum of thyroid dysfunction in diabetes mellitus.
Methodology
Study group
The study includes all type 2 diabetics from OPD’S and IPD’S of all the departments of MVJ MC & RH, HOSKOTE.
100 patients of type 2 are selected from OPD and IPD in a random fashion,studied and followed up for 2 years.
Inclusion Criteria
1) All patients with Type 2 diabetes aged more than 30 years.
2) All diabetics irrespective of glucose control.
3) All diabetics irrespective of treatment(OHA/insulin).
Exclusions criteria
1) Type 1 DM
2) Patients with:
a) Gestational diabetes mellitus.
b) Fibrocalculouspancreatitis.
c) Pancreatitis.
d) Steroid induced Diabetes, would be excluded.
3) All those who had proven thyroid disorder and on treatment.
A detailed history was taken and examination done as per the proforma. All patients in addition to haematological and routine urine work up underwent target organ evaluation for diabetes. All patients were evaluated for thyroid status; assessment of T3, T4 and TSH levels and as required FNAC and biopsy was done by our pathologist in MVJ Hospital.
The laboratory evaluation of thyroid functions was done by estimation of serum T3, T4 and TSH levels by chemi-lumiscence assay method. Two ml of blood was drawn and centrifuged and serum (500microml) collected from that and incubated with the reagent (separate for T3, T4 and TSH) for about 1 hour at room temperature. Later the readings were taken from the instrument COBAS 6000.
The normal readings are
T3 – 0.7- 2.0 ng/ml
T4 – 4.5- 11.0 microg/dl
TSH- 0.4- 5.0 microIU/ml
The method employed for FNAC thyroid was under aseptic precaution, using 10ml sterile syringe and 22-24G needle aspiration were taken from two different sites of the thyroid gland. The aspirates were smeared over the glass slide and covered by a cover slip of 0.4mm thickness. The slide dipped in the container containing the fixative 70-90% ethanol. Later the slide was studied under the high power microscope. The reporting was done by the pathologist.
Diabetic states of the patients were estimated by analyzing RBS/PPBS/FBS by glucose oxides wherein 1ml of blood was drawn and centrifuged to collect the serum, 10mu of serum is incubated with 1ml of reagent at room temperature for 15min. Later the reading taken from the instrument.
Patients were diagnosed based on the ADA criteria for diabetes.
• Symptoms of diabetes plus random blood glucose concentration of 11.1 mmol/L (200 mg/dL)
or
• Fasting plasma glucose of 7.0 mmol/L (126 mg/dL)
or
Two-hour plasma glucose of 11.1 mmol/L (200 mg/dL) during an oral glucose tolerance test.
Results
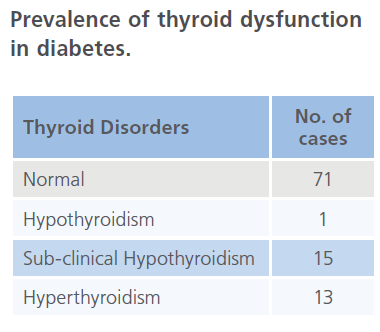
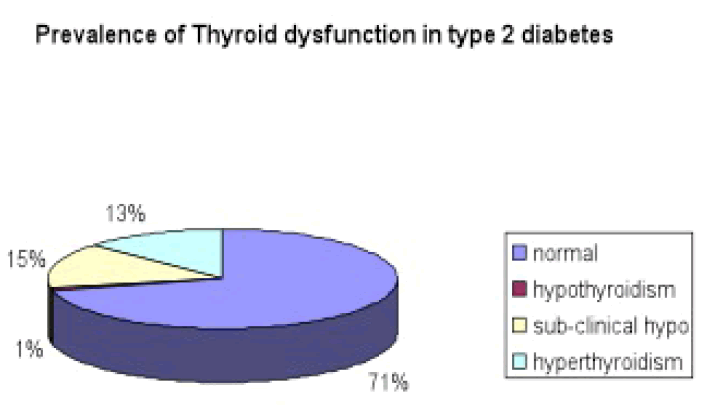
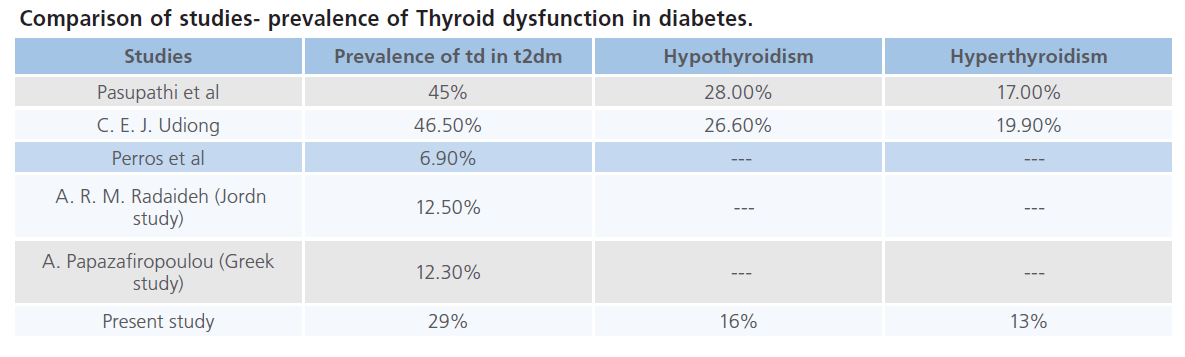
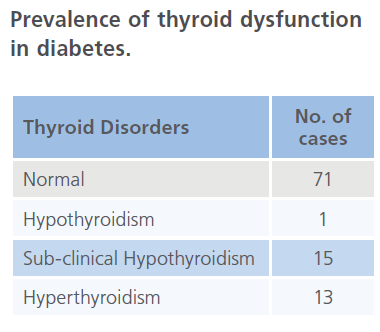
1) In this study, 100 established diabetics were screened for thyroid disorders by TFT. Abnormal thyroid function was found in 29 T2DM cases and remaining diabetics had normal thyroid function. Among 29 cases low thyroid function was noted in 16 patients and 13 subjects had Sub-clinical hypothyroidism. Hyperthyroidism was noted in 13 people.
2) Out of the 16 Hypothyroid subjects 1 had overt hypothyroidism and 15 had Sub-clinical hypothyroidism. Hyperthyroidism was noted in 13 people.
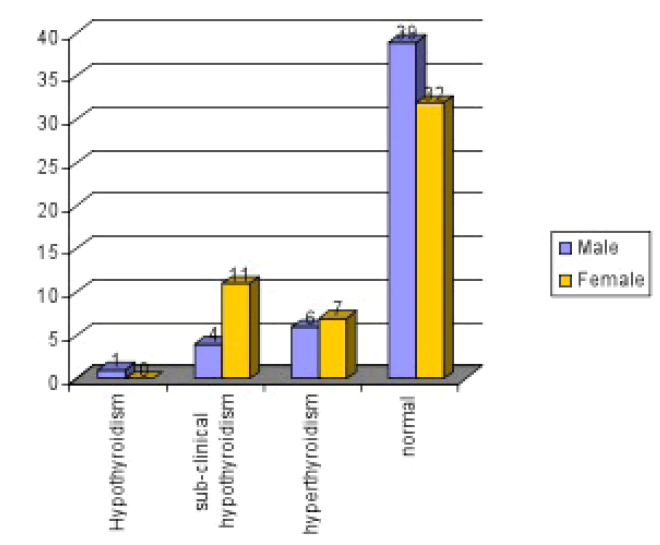
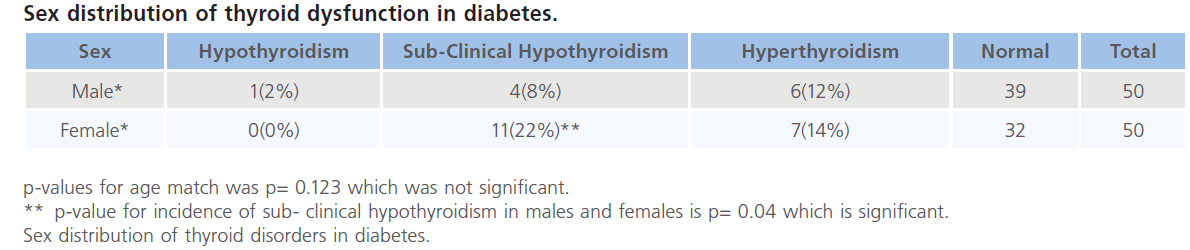
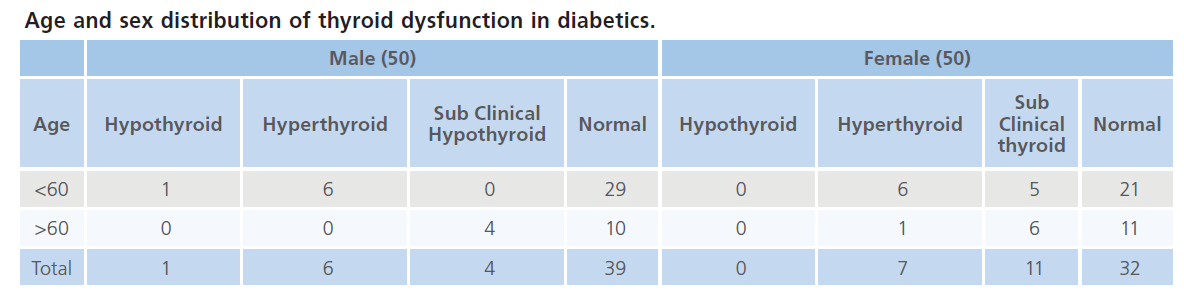
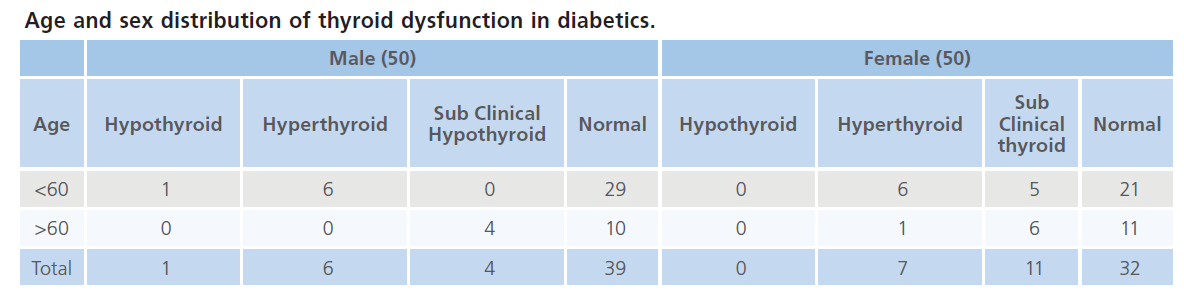
3) In the present study of 100 patients with Type 2 diabetes, 50 were males and 50 were females. We have found that prevalence of thyroid dysfunction was more among females than in males. 11 out of 50 male patients had thyroid dysfunction where as 18 of the 50 females were suffering from thyroid disorders.
The spectrum of thyroid disorders varied among the either sex. Hypothyroidism was present in one male patient where as none of the females had hypothyroidism in this study. Sub- clinical hypothyroidism was present in 4 out of 50 male patients and 11 out of 50 females where p-value was significant. Hyperthyroidism was more among females compared to males but no statistical difference (6 and 7 out of 50 males and females) was noted.
In this study prevalence of thyroid disorders in male and female were 22% and 36%, of which 22% females had subclinical hypothyroidism, 14% had hyperthyroidism. Among males Sub-clinical hypothyroidism was seen in 8%, hypothyroidism in 2% and hyperthyroidism in 12%.
4) In this study we had 68 people with type 2 diabetes below the age of < 60 years (adult and middle age) and 32 people over the age of 60 years (elderly). The spectrum of thyroid disorders among this groups were as follows – Out of the 68 patients below the age of 60 years 5 had sub- clinical hypothyroidism, 1 hypothyroid and 12 of them where hyperthyroid and out of 32 elderly patients we found 10 with sub- clinical hypothyroidism and 1 had hyperthyroidism. No hypothyroid cases where noted in elderly people.
In this study prevalence of sub-clinical hypothyroidism (31.25%) was more in elderly compared to 7.36% in adult and middle age group, where as 17.65% below the age of 59 years had hyperthyroidism to that of 3.12% among elderly. Hypothyroidism was present in 1.47% of people below the age of 59 yrs where as none of the elderly had hypothyroidism.
In this study we also found that Sub-clinical hypothyroidism is more in elderly people with type 2 Diabetes where as hyperthyroidism was more among the adult and middle age group.
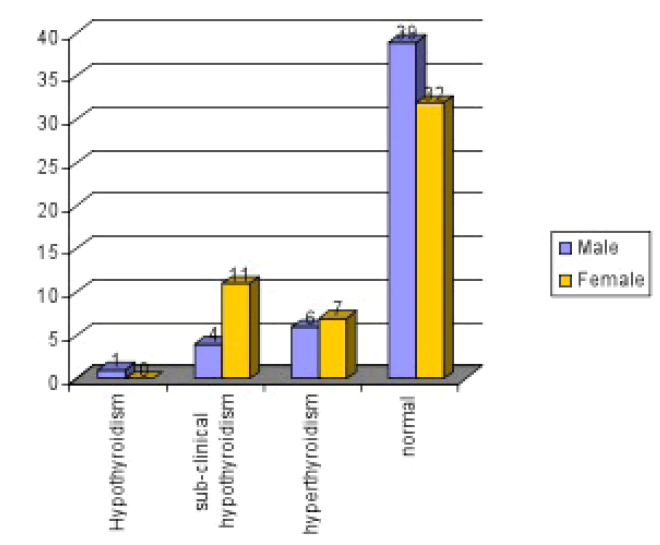
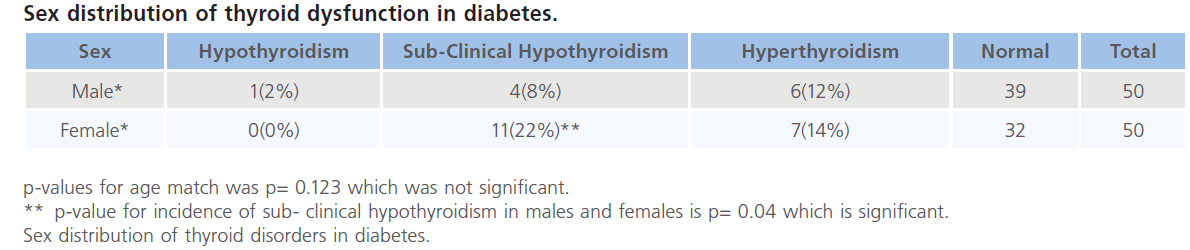
In this study sub-clinical hypothyroidism is more among females (22%) than males (8%). Hyperthyroidism showed no much difference in females (14%) and males (12%).
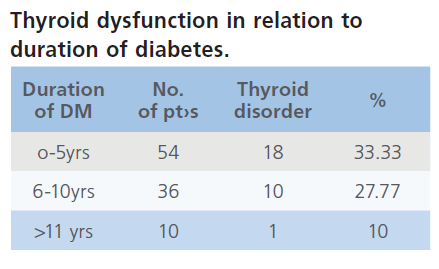
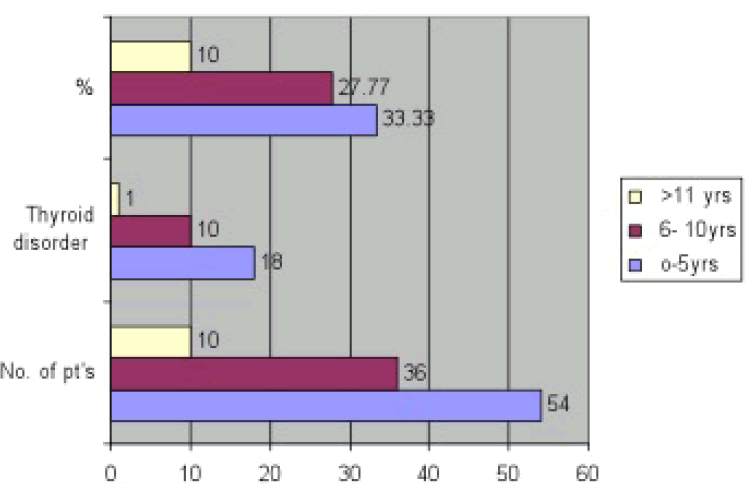
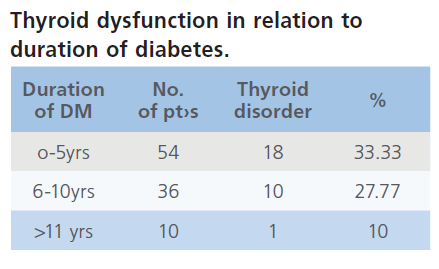
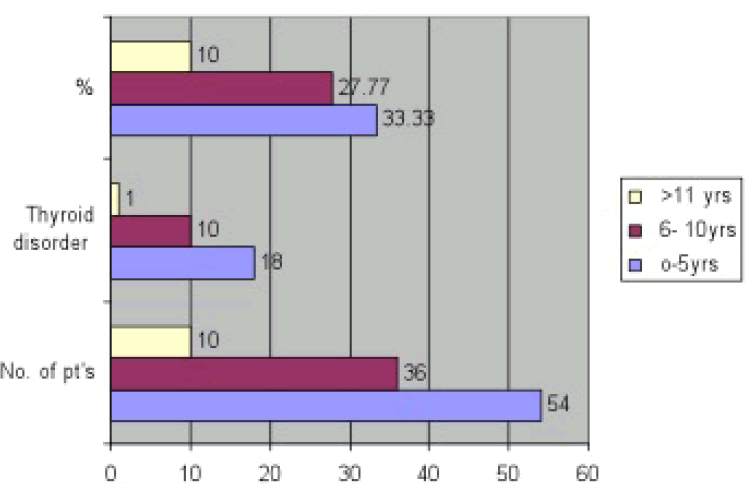
5) We have divided the 100 diabetics in this study into three groups according to the duration of diabetes.
54 people where in the duration of 0-5 yrs and 36 where 6-10 yrs and the remaining 10 had more than 10 years duration of diabetes. p-value (chi-square value) was highly significant 0.0012. Increased duration of diabetes had no significance with relation to increase in thyroid dysfunction in this study (p=0.0012).
6) Out of 100 patients with diabetes, symptoms of thyroid disorder were present in 8 patients.
All the 8 patients with symptoms of thyroid disorder where hyperthyroid remaining cases had no symptoms of thyroid disease. Even the diabetic with overt hypothyroidism had no symptoms or signs of thyroid disease.
The symptoms with which the patients with hyperthyroidism presented where heat intolerance, sweating, palpitations, fatigue/weakness, increased appetite and menstrual disturbances.
These symptoms can also be mistaken for diabetes except for heat intolerance and palpitations.
All of these patients had fatigue/weakness, sweating and heat intolerance along with menstrual irregularities in females. Two had palpitations and increased appetite. Only sign noted was fine tremors in 3 patients.
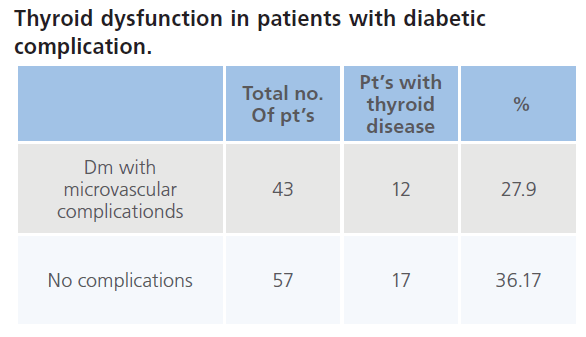
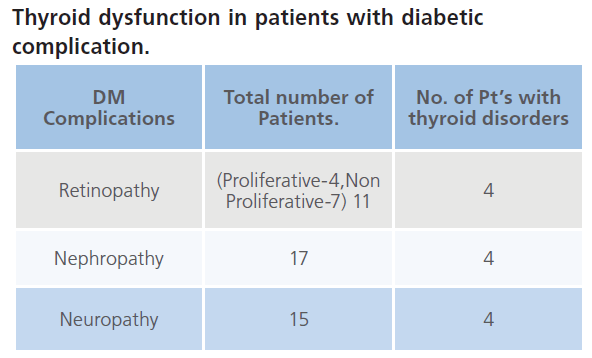
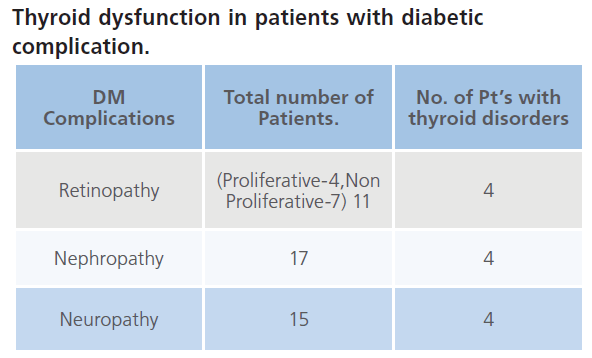
7) In this study, out of 100 patients with Type 2 diabetes 43 patients had complications of diabetes in the form of retinopathy, nephropathy and neuropathy based on clinical and laboratory evidences. 12 out of 43 patients had thyroid- disorders.
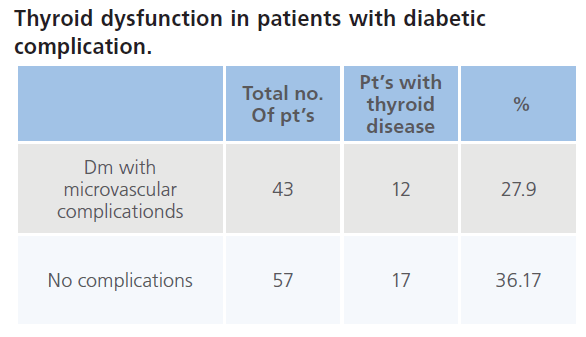
Out of the 43 patients with complications retinopathy was present in 11(non- proliferative stage in 4 and proliferative in 7), nephropathy in 17 and neuropathy.
2 patients out of them had all the three complications where as 9 had retinopathy and nephropathy. Retinopathy and neuropathy were seen in 2 patients and 4 had neuropathy and nephropathy. Two patients had history of IHD.
Out of 11 patients with retinopathy in this study 4 had thyroid disorders of which 3 had sub-clinical hypothyroidism and 1 had hyperthyroidism. Nephropathy was diagnosed in 17 patients but thyroid dysfunction was present in 4 patients out of which 3 had sub-clinical hypothyroidism and 1 had hyperthyroidism. Neuropathy was seen in 15 patients with thyroid disorders out of which 2 had hyperthyroidism.
Discussion
Among the endocrinal metabolic diseases diabetes occupies the major share. India has the dubious distinction of being home to the largest number of people suffering from diabetes in any country. The disease is responsible for significant mortality and morbidity due to the complications
This study was conducted at MVJ medical college, Thyroid functions where studied in type 2 Diabetes Mellitus patients attending the OPD and IPD of MVJ hospital.
A total of 100 type 2 diabetics were studied. All were confirmed diabetics who previously had plasma glucose levels of >126 mg/ dl or RBS of >199 on more than one occasion and were receiving treatment such as Insulin, OHA’s or physical exercise therapy. All these patients comprised of rural population.
Prevalence and spectrum of thyroid disorders in type 2 diabetics.
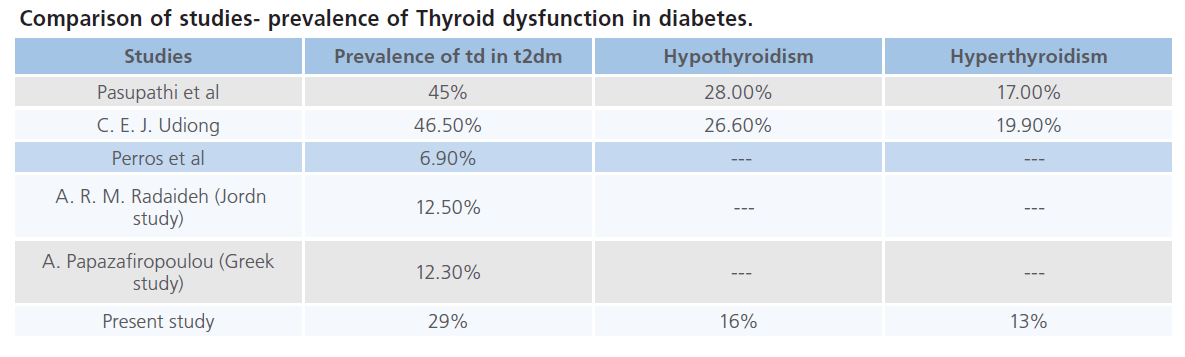
In this study of 100 patients with type 2 diabetes 50 where males and 50 females. We have found 29 patients with thyroid disorders that are 29%, and number of reports have also indicated higher than normal prevalence of thyroid disorders.
Pasupathi et al in their study found that prevalence of thyroid disorder was 45% among type 2 diabetics. Hypothyroidism was present in 28% and 17% had hyperthyroidism.
A prevalence of 12.3% was reported among Greek diabetic patients and 16% of Saudi patients with type 2 diabetes were found to have thyroid dysfunction. In Jordan, A study reported that thyroid dysfunction was present in 12.5% of Type 2 diabetic patients.
Perros et al. demonstrated an overall prevalence of 13.4% of thyroid diseases in diabetics with the highest prevalence in type 1 female diabetics (31.4%) and lowest prevalence in type 2 male diabetics (6.9%).
In this study out of the 29 patients with thyroid dysfunction 15 had hypothyroidism, 1 had overt hypothyroidism and 13 had hyperthyroidism.
It is noted that there is a lower incidence of Thyroid dysfunction in diabetics among Europeans as compared to that of Indians as per the Indian studies.
In this study sub-clinical hypothyroidism was more among females 22% compared to males 8%. Sub-clinical hypothyroidism was more common among elderly females 12%. Hyperthyroidism was almost equal in either sex with 12% in males and 14% in females. Overt hypothyroidism was present in one male patient in our study.
Many studies have shown increased incidence of sub-clinical hypothyroidism in elderly females compared to males. Hyperthyroidism was more common in males than in females.
The presence of both high and low levels of thyroid hormones in diabetics in this study may be due to modified TRH synthesis and release, and may depend on the glycemic status of the diabetics studied. Glycemic status is influenced by insulin, which is known to modulate TRH and TSH levels.
Thyroid dysfunction in diabetics in relation to age
In this study we have found 34.4% patients with thyroid disorders over the age of 60 years compared to that of 26.4% below the age of 60 years. Sub-clinical hypothyroidism was 31.2% in patients above 60 years.
Flatau and Trougoubof have also observed similar findings. They have reported 38% with sub- clinical hypothyroidism after the age of 60 years. Diabetes mellitus and thyroid disorders are common in the elderly.
The prevalence of hypothyroidism was 14% (9.7% in males and 18.2% in females) and that of DM was 11.5% (12.1% in males and 11.1% in females). In 74% of the diabetics the diagnosis was made after the age of 60 years. Subclinical hypothyroidism (serum TSH levels above 4.5 mU/L with normal FT4 levels) was detected in 38% of all the hypothyroid subjects.
Flatau and Trougouboff have concluded that diabetes mellitus and primary hypothyroidism are common disorders in elderly subjects. DM in the elderly can usually be handled with diet and oral hypoglycemic drugs. Since the clinical features of hypothyroidism in the elderly are often atypical, we suggest that elderly subjects should be screened for hypothyroidism.
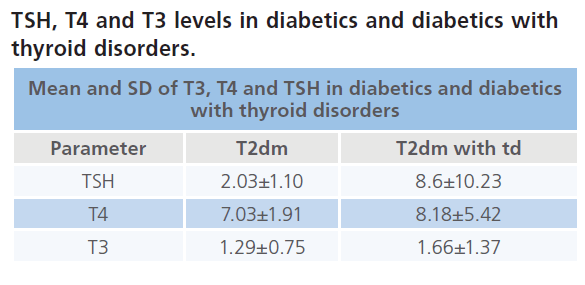
In this study we have found that there is variation in the TSH levels and T3, T4 levels found in diabetics and diabetics with thyroid disorders. Patients with thyroid disorders had higher levels of TSH compared to those without thyroid disorders where as there was no much difference in T4 and T3 levels. Findings in our study are similar to that of Pasupathi et al and Shalini Gupta et al.
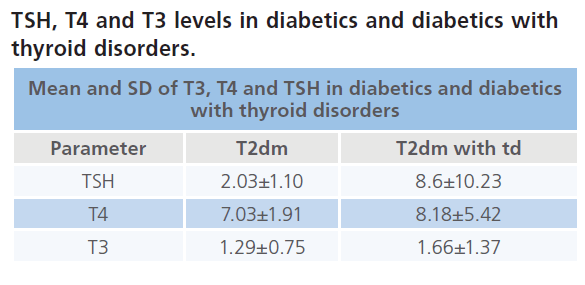
The guidelines of American thyroid association and American association of clinical endocrinology recommend serum TSH measurement as single most relevant test to diagnose all forms of hypo and hyperthyroidism.
TPO antibodies and thyroid disorders
TPO antibodies was positive in 29.4% of patients and the others where negative. Other studies have reported higher prevalence of TPO-Ab both in general population and diabetics and opined that they have a 90% negative predictive value. The association of positive TPO-Ab and future development of hypothyroidism is known. Hence this cannot be used as the diagnostic tool because of the high negative predictive value
Clinical features of thyroid disorders in diabetics
In this study we have found that patients with hyperthyroidism presented with clinical features compared to that of hypothyroidism. Hyperthyroid patients presented with heat intolerance, sweating, palpitations, fatigue/weakness, increased appetite and menstrual disturbances. All of these patients had fatigue/ weakness, sweating and heat intolerance along with menstrual irregularities in females. Two had palpitations and increased appetite. Only sign noted was fine tremors in 3 patients.
Not many papers regarding clinical features of thyroid disorders in T2DM are present. Udiong et al. [1] have reported similar observation in their study on clinical examination. We have found that 61% of the hyperthyroid patients with type 2 diabetics had presented with clinical features of hyperthyroidism.
Effect of thyroid disorder on diabetes
In this study we have found that 17% hyperthyroid patients had a poor glycemic control compared to that of hypothyroid patients. We did not find hypoglycaemia in any of our patients with sub-clinical hypothyroidism.
Hyperthyroidism impairs glycemic control in diabetic subjects, while hypothyroidism may increase susceptibility to hypoglycaemia thus complicating diabetes management. Furthermore, it seems that unidentified thyroid dysfunction could negatively impact diabetes and its complications. A higher frequency of retinopathy and nephropathy was observed in diabetic patients with sub-clinical hypothyroidism, and more severe retinopathy was noted as well. Therefore, management of sub-clinical hypothyroidism in patients with diabetes may prove beneficial.
Diabetic complications where present in 43 patients of which 12 patients had thyroid disorders. Four had retinopathy of which 3 where sub- clinical hypothyroid and 1 had hyperthyroid. All the 3 patients with sub-clinical hypothyroidism had proliferative retinopathy and 1 hyperthyroid patient had NPDR. All the 4 patients who had retinopathy also had nephropathy.
Our findings of diabetic complications like retinopathy (proliferative) and nephropathy where more among sub- clinical hypothyroid patients. These findings where similar to those observed by Mirella Hage in their study. The reason for this could not be explained.
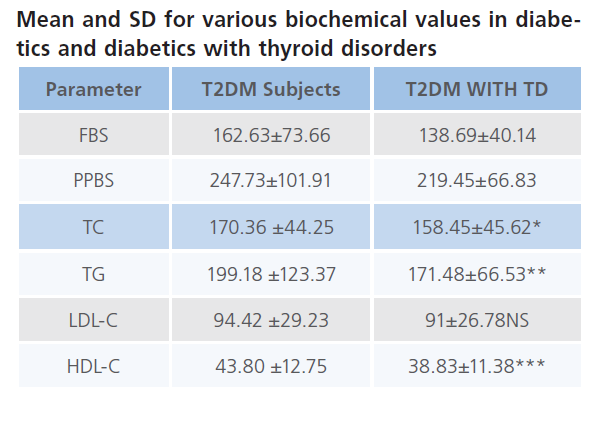
Dyslipidemias in diabetics and thyroid disorders
In this study we have also seen for disturbances in lipid profile in patients with thyroid dysfunction. We have noticed increased levels of triglycerides in patients with thyroid dysfunction. HDL, VLDL and Cholesterol where in normal ranges.
Pasupathi et al. in their study found that there were increased levels of HbAIC, triglycerides and VLDL-C and reduced level of HDL-C in diabetics. In our study we have found a similar pattern of biochemical disturbances was found.
Diabetes has been shown to be associated with numerous thrombotic, atherosclerotic, and cardiovascular diseases. Cholesterol has been singled out as the cause of atherosclerosis. However, other lipids, such as triglycerides and phospholipids, also show similar correlations. Pasupathi et al. in his study, found levels of serum lipids to be elevated in diabetic patients. The abnormally high concentration of serum lipids in diabetes is mainly a result of the increase in mobilization of free fatty acids from peripheral depots. This happens because reduced insulin levels increase the activity of the hormone sensitive lipase. On the other hand, glucagons, catecholamines, and other hormones enhance lipolysis. The marked hyperlipedemia that characterizes the diabetic state may therefore be regarded as a consequence of the uninhibited actions of lipolytic hormones on fat depots. The increase and fall in the individual lipoprotein levels is a reflection of the total serum cholesterol levels; that is, the levels of VLDL-C, LDL-C, and HDL-C increase or decrease with the level of total serum cholesterol, and it is their ratio that determines the pathophysiology of lipoprotein metabolism.
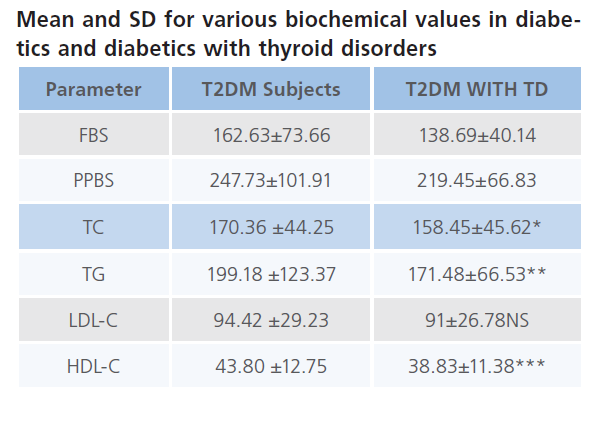
The p-value was significant as shown below in the table for TC, TG and HDL-C in Diabetics.
Conclusion
• Prevalence of thyroid dysfunction was seen in 29% of diabetics studied.
• Sub-clinical hypothyroidism was more common than other conditions which constituted 22% of the thyroid dysfunction in the Diabetics.
• Elderly patients had higher incidence (34.4%) of thyroid dysfunction.
• Thyroid disorders are more in females (36%) than males 22%.
• Patients with hyperthyroidism presented with clinical features of thyroid disorders (61%) where as hypothyroid patients did not have any signs and symptoms.
• Thirty six percent of people with thyroid dysfunction had poor glycemic control even with treatment.
• Severe forms of diabetic complications where noted in subclinical hypothyroidism. Hence, patients with sub-clinical hypothyroidism must undergo frequent ophthalmic checkup’s to rule out retinopathy and also renal function test for nephropathy,
• There is no relation of thyroid disorders with duration of diabetes
• A serum TSH within euthyroid range almost always eliminates the diagnosis of hypo or hyperthyroidism. This shows that TSH is preferred screening test for thyroid dysfunction in diabetics.
• Heat intolerance and palpitations are specific symptoms of hyperthyroidism in Diabetes.
• One must have strong suspicion of thyroid dysfunction in patients with uncontrolled glycemic levels and must be evaluated for hyperthyroidism especially in young and middle aged diabetics with poor glycemic control.
330
References
- Udiong, C.E.J., Udoh, A.E., Etukudoh, M.E. Evaluation of thyroid function in diabetes mellitus in Calabar, Nigeria. Indian Journal of Clinical Biochemistry 2007; 22 (2): 74-78.
- Tunbridge, W.M.G., Evered, D.C., Hall, R. The spectrum of thyroid disease in a community: the Whickham survey. Clinical Endocrinology 1977; 7 (6): 481-493.
- Canaris, G.J., Manowitz, N. R., Mayor, N.R., Ridgway, E.C. The colorado thyroid disease prevalence study. Archives of Internal Medicine 2000; 160 (4): 526-534.
- Hollowell, J. G., Staehling, N. W., Flanders, W. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). Journal of Clinical Endocrinology and Metabolism 2002; 87 (2): 489- 499.
- Perros, P., McCrimmon, R. J., Shaw, G., Frier, B.M. Frequency of thyroid dysfunction in diabetic patients: value of annual screening. Diabetic Medicine 1995; 12 (7): 622- 627.
- Papazafiropoulou, A. Prevalence of thyroid dysfunction among Greek Type 2 diabetic patients attending an outpatient clinic. Journal of Clinical Medicine Research 2010; 2 (2): 75-78.
- Akbar, D.H., Ahmed, M. M., Al-Mughales, J. Thyroid dysfunction and thyroid autoimmunity in Saudi type 2 diabetics. Acta Diabetologica 2006; 43 (1): 14-18.
- Radaideh, A. R. M., Nusier, M. K., Amari, F. L. et al. Thyroid dysfunction in patients with type 2 diabetes mellitus in Jordan. Saudi Medical Journal 2004; 25 (8): 1046-1050.
- Kordonouri, O., Charpentier, N., Hartmann, R. GADA positivity at onset of type 1 diabetes is a risk factor for the development of autoimmune thyroiditis. Pediatric Diabetes 2011; 12 (1): 31-33.