Mayur Chalia* and Thyagarajan Subramanian
Department of Neurology, Penn State Health Milton S. Hershey Medical Center, Hershey, PA, USA
*Corresponding Author:
Mayur Chalia
Department of Neurology, Penn State Milton S. Hershey Medical Center
500 University Drive, Hershey, PA, USA
Tel: +61 (0) 428 688 800
E-mail: mayurchalia@gmail.com
Received Date: September 21, 2018; Accepted Date: October 22, 2018; Published Date: October 26, 2018
Citation: Chalia M, Subramanian T (2018) A Rare Case of Acute Hemichorea with Conduction Aphasia due to Cavernous Malformation. J Neurol Neurosci Vol.9 No.5:272. DOI: 10.21767/2171-6625.1000272
Chorea secondary to cavernous malformation (CM) is uncommon and deficits can vary depending on the degree of involvement of surrounding structures. Unlike other vascular malformations, CM is not encapsulated. Therefore, hemorrhages from a CM can extend to involve adjacent brain structures. We present here a rare case of acute hemichorea with conduction aphasia due to hemorrhagic conversion of a CM, its diagnostic work up, and successful therapy. We demonstrate lesion-behavior mapping, combining both structural and functional data to elucidate the pathophysiology of this presentation.
Keywords
Movement disorders; Basal Ganglia; Involuntary movements; Language disorder; Lesionbehavior mapping
Introduction
Chorea secondary to cavernous malformation (CM) is uncommon and deficits can vary depending on the degree of involvement of surrounding structures [1]. Unlike other vascular malformations, CM is not encapsulated. Therefore, hemorrhages from a CM can extend to involve adjacent brain structures [2]. We present here a rare case of acute hemichorea with conduction aphasia due to hemorrhagic conversion of a CM, its diagnostic work up, and successful therapy. We demonstrate lesion-behavior mapping, combining both structural and functional data to elucidate the pathophysiology of this presentation.
Case Report
A 78-year-old right-handed woman with history of hypertension presented with involuntary movements of right hemibody and speech difficulty without changes in her level of consciousness for 6 weeks duration. On presentation, she had slight afluency and difficulty with repetition, but intact naming and comprehension. Her involuntary movements in the right upper extremity and to a lesser extent in the right lower extremity were consistent with hemichorea. The rest of her neurologic examination was normal. Laboratory work up including CBC, BMP, HbA1C and blood smear for acanthocytes were all normal. Urine 24 hour assessments for heavy metals and full ophthalmological work up was negative.
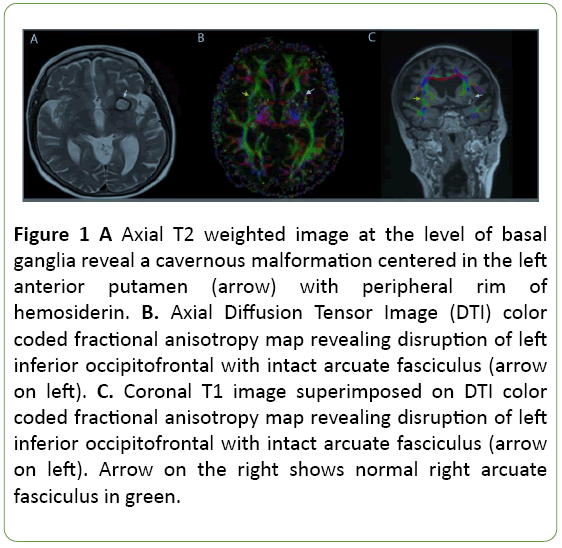
T2-weighted MR imaging showed a hemorrhagic lesion in the left anterior putamen (Figure 1A) explaining hemichorea, but not aphasia. To evaluate immediate adjacent white matter, we obtained Diffusion Tensor Imaging (DTI) sequence and tractography which showed disruption of left inferior frontooccipital fasciculus (IFOF) with intact arcuate fasciculus (Figures 1B and 1C). Treatment with risperidone 0.25mg twice daily resulted in resolution of hemichorea in 3 weeks and was not associated with any side effects such as parkinsonism or tardive dyskinesias.
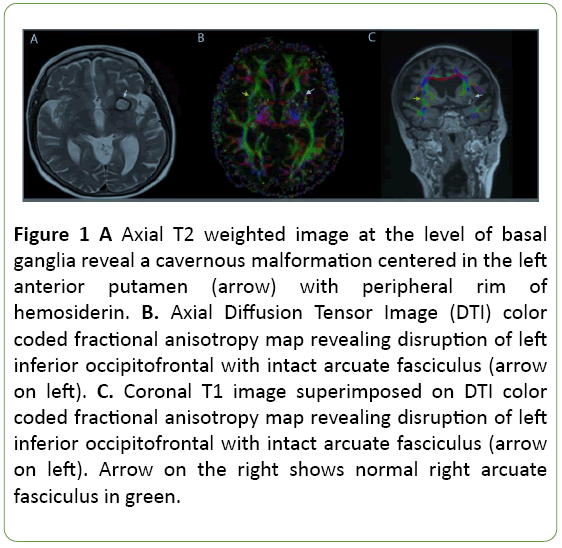
Figure 1: A Axial T2 weighted image at the level of basal ganglia reveal a cavernous malformation centered in the left anterior putamen (arrow) with peripheral rim of hemosiderin. B. Axial Diffusion Tensor Image (DTI) color coded fractional anisotropy map revealing disruption of left inferior occipitofrontal with intact arcuate fasciculus (arrow on left). C. Coronal T1 image superimposed on DTI color coded fractional anisotropy map revealing disruption of left inferior occipitofrontal with intact arcuate fasciculus (arrow on left). Arrow on the right shows normal right arcuate fasciculus in green.
Discussion
Intracranial cavernous malformations are a group of dilated blood vessels with loss of elastin fibers in the vessel walls, which predisposes them to bleed [1]. Cavernous malformation (CM), unlike other vascular malformations, is not encapsulated. Therefore, hemorrhages in CMs can extend into surrounding structures [1]. Involvement of CMs in basal ganglia can lead to movement disorders including chorea [2-6]. Pathophysiology of choreiform movements in basal ganglia disorders have been implicated on excessive activity in the D1- receptor mediated direct pathway and under activity in the D2- receptor mediated indirect pathway. However, recent studies using lesion network mapping show that 90% of vascular causes for chorea localize to the posterolateral putamen where the CM was located in our patient. This putaminal overlap site is connected to the broader motor network that includes the supplemental motor area and the premotor cortex, suggesting that pathophysiology of chorea may be mediated by a larger disruption of the motor network [7]. Axial T2 weighted image at the level of basal ganglia reveal a cavernous malformation centered in the left anterior putamen with peripheral rim of hemosiderin (Figure 1A). DTI is an advanced MR imaging sequence, which delineates details of white matter tracts that are not readily visible on routine sequences like T2 and FLAIR. DTI revealed discontinuity of left inferior fronto-occipital fasciculus (IFOF) with intact arcuate fasciculus (Figures 1B and 1C). Role of the inferior frontooccipital fasciculus (IFOF) in language has been reported in the literature [8,9]. This accurate depiction of white matter involvement helps explain neurological symptoms precisely.
Conclusion
To our knowledge, the acute presentation of hemichorea with aphasia is unique and never previously reported. Lesionbehavior mapping combining both structural and functional data is a powerful tool to study brain function. This case demonstrates that careful clinical examination combined with modern neuroimaging can provide accurate pathophysiological explanations for even rare presentations of a relatively common movement disorder.
23559
References
- Taslimi S, Modabbernia A, Amin-Hanjani S, Barker FG, Macdonald RL (2016) Natural history of cavernous malformation: A systematic review and meta-analysis of 25 studies. Neurology 86: 1984-1991.
- Kobayashi K, Aoyama N, Sasaki J (2011) MRI appearance of a cerebral cavernous malformation in the caudate nucleus before and after chorea onset. J Clin Neurosci 18: 719-721.
- Carella F, Caraceni T, Girotti F (1992) Hemichorea due to a cavernous angioma of the caudate. A case report of an aged patient. Ital J Neurol Sci 13: 783-785.
- Carpay HA, Arts WF, Kloet A, Hoogland PH, Van Duinen SG (1994) Hemichorea reversible after operation in a boy with cavernous angioma in the head of the caudate nucleus. J Neurol Neurosurg Psychiatry 57: 1547-1548.
- Hidaka M, Shimoda M, Sato O, Watabe T, Tsugane R (1989) Hemiballism due to a putaminal cavernous hemangioma. No To Shinkei 41: 1135-1139.
- Lopez-Valdes E, Posada IJ, Munoz A, Bermejo F (1998) Acute hemichorea caused by a cavernous angioma in the caudate. Neurologia 13: 205-206.
- Laganiere S, Boes AD, Fox MD (2016) Network localization of hemichorea-hemiballismus. Neurology 86: 2187-2195.
- Martino J, Brogna C, Robles SG, Vergani F, Duffau H (2010) Anatomic dissection of the inferior fronto-occipital fasciculus revisited in the lights of brain stimulation data. Cortex 46: 691-699.
- Mandonnet E, Nouet A, Gatignol P, Capelle L, Duffau H (2007) Does the left inferior longitudinal fasciculus play a role in language? A brain stimulation study. Brain 3: 623-629.