Keywords
Epilepsy; Pregnancy; Fetal distress; Peripartum; Preconception
Abbreviations
AEDS: Antiepileptic Drugs; WWE: Women with Epilepsy; IQ: Intelligent Quotient; MCM: Major Congenital Malformation; IGE: Idiopathic Generalized Epilepsy; IUGR: Intrauterine Growth Retardation; IUD: Intrauterine Death; SLE: Systemic Lupus Erythmatosis; APGAR score: Appearance, Pulse, Grimace, Activity, Respiration
Introduction
Epilepsy is one of the most common and serious central nervous system disorders worldwide without any respect for the age, race, social class, or geographic boundary. Its observed global prevalence is 5 to 10 cases per 1000 persons with the disease burden of 40-50 million sufferers worldwide today [1,2]. About 85% of these sufferers live in the developing countries and 60% to 90% out of them could not get asses to the standard treatment facilities. Health care systems in developing countries are unable to tackle the magnitude of the problem encountered in this regard and also there is threat that it is going to get worse over the time due to limited resources available [1].
One of the important issues linked to epilepsy that arises in young female patients is the interactions of epilepsy and Anti- Epileptic Drugs (AEDS) with the reproductive health issues [3]. There may be worsening seizure frequency during pregnancy and postpartum period also do seizures effect the maternal and fetal outcomes if not managed properly. Finding from several studies demonstrated that about 60-70% of the epileptic females had unchanged seizure frequency during the entire pregnancy. About 16% had a worsening of the seizure control and 12% had a reduction in seizures frequency. Occurrence of status epilepticus in pregnancy was reported in 0.6% of the epilepsy cases [4]. According to the literature approximately one quarter of all patients with active epilepsy are in childbearing age and awareness among the target population about the potential teratogenic effects of AEDS is below the expected level [5].
Various issues regarding to the effects of epilepsy on reproductive health that needs to be addressed include changes in pharmacokinetics, volume of distribution and the hepatic metabolism of AEDs besides the matters related to the long-term effects of in-utero exposure to AEDs on cognitive functioning and neurodevelopment. It has been observed in some studies that the mean intelligence quotient (IQ) was significantly lower in children born to the women having epilepsy. Also, Other the hemorrhagic disease in the newborn, the increased rates of fetal loss and reduced growth parameters have also been observed in fetuses being exposed to the enzyme inducing AEDs [6]. In the peripartum period, it was noted that the females with epilepsy were up to four times more likely to have an induced labor and twice as likely to have a caesarean section, although the most could have a normal delivery [7]. The teratogenic potential of various AEDS vary, and it increases further with the combination of AED,S. Some of the adverse events reported in literature include Major congenital malformation (MCM), occurring in 2-3% to 4-7% [8,9] of the cases while being on the monotherapy [8].
Due the ethical issues involved randomized controlled trials on pregnant women is not possible, so we have to rely on the observational data to establish the future management of epilepsy in pregnancy [9]. For this purpose, various pregnancy registries have been established that helped in collecting the prospective data, of the pregnant epileptic patients exposed to AEDs [10,11]. There is no such registry available in Pakistan. This registry marks our initial steps in this direction that will not only help to understand the course and the outcomes of pregnant epileptic women in Pakistan but also to provide guidelines for making amendments in the health system related to epilepsy and reproductive health services.
Objective and Purpose of the Registry
To collect the epidemiological and clinical data of the pregnant epileptic patients presenting to neurology centre.
Methodology
This study was done at Neurology Clinic and Neurology In-patient Services at Shifa International Hospital, Islamabad. This is an ongoing prospective registry, so all identified pregnant women with epilepsy were enrolled after informed consent. This is the initial analysis at the end of first year and second analysis will be carried at the end of 2nd year of enrolment. Approval was taken from the hospital’s ethical committee. Informed written consent was taken from all patients/next of kin for enrolment. Confidentiality was maintained throughout the registry and only the project director and her assigned people had access to the data.
Inclusion criteria
• All pregnant women with epilepsy at the time of conception.
Exclusion criteria
• Women on antiepileptic drugs for other causes exclusive of epilepsy (e.g. bipolar disorder, trigeminal neuralgia, headache).
• Women who had first seizure during pregnancy due to any identifiable provoked cause, e.g. eclampsia.
• Women with severe co-morbid conditions like hypertension, diabetes mellitus, Systemic Lupus Erythmatosis (SLE), rheumatoid arthritis, if their severity can independently alter the outcomes of pregnancy.
Data collection
The data about the variables of interest was collected by using a questionnaire designed for this purpose that included the information about the basic demographics like age, education level, socioeconomic status, occupation and any other comorbids. They were asked about the time since the onset of the epilepsy, average number of the seizures/month, type of the seizures, any family history of epilepsy and fetal malformations. Also, the data on number of previous pregnancies and any maternal and fetal complications related to them were obtained from the patients themselves and the records. Also, information on access to the preconceptual counseling facilities, use of contraceptives and planning before pregnancies was collected from patients and records.
The AEDs used as a monotherapy or in combination were also recorded along with the duration and doses and any previous AEDs that were used as depicted by patient records or selfrecalled by the patient. The patients were followed over phone and the routine follow-ups in clinic or in patient services regularly till the delivery to document information on any maternal and fetal complications during pregnancy and peripartum period, mode of delivery and the treatment taken.
Statistical Methods
All data was entered and analyzed using standard statistical software SPSS version 20. The descriptive statistics including the frequencies, means and standard deviation were calculated for the variables mentioned above. The monotherapy and polytherapy groups were compared with each other regarding the maternal and fetal complications during the pregnancy and perinatal period and the mode of delivery in two groups were also compared. Chi square test was applied to determine any significant difference in two groups using the value of p<0.05.
Results
There were 65 epileptic patients with pregnancy presenting to us. Mean age was 27 ± 5. Majority of them were housewives and despite most of them being educated up to graduation, nearly none being working currently. It was seen equally common in fair to good socioeconomic class. Because most females of the productive age are young, cardiovascular and other co-morbid were seen only in 3 patients. The basic demographic features of the participants are given in Table 1.
| Variables |
n (%) |
| Total (n) |
65 |
| Age (n) |
65 |
| Mean |
27.5 ± 5.02 |
| Education (n) |
65 |
| Missing |
29 |
| Uneducated |
5 |
| Primary |
7 |
| Intermediate |
8 |
| Graduation |
11 |
| Post graduate |
5 |
| Occupation |
65 |
| Missing |
20 |
| House wife |
41 |
| Not working |
2 |
| Others |
2 |
| Socio-economic condition |
65 |
| Missing |
40 |
| Good |
10 |
| Fair |
11 |
| Poor |
4 |
| Co-morbids |
65 |
| Missing |
6 |
| None |
56 |
| HTN |
2 |
| MDD |
1 |
Table 1: The basic demographics of the participants.
Most common type of epilepsy was Idiopathic or genetic Generalized Epilepsy (IGE), while genetic focal epilepsy was second common epilepsy observed in our epilepsy. Symptomatic epilepsy was seen only in 5 patients. The most common age of onset of epilepsy was 16-25, as IGE usually start in second to third decade, followed by age 4-15 the typical age for genetic epilepsies. About 1/3 had positive family history of epilepsy. Most had seizure frequency less than 5/month with most being quite adherent and compliant, only 10% of the participants being noncompliant. The most common trigger of the seizure was missing the dose of AED.
Regarding the findings related to reproductive health, contraception was used by only 7 participants. About 25 had unplanned pregnancy, only 20 patients opted to take preconception counseling, almost all took folic acid except the 6 patients. Statistics of preconception related issues are shown below. About 29 patients had first pregnancy at presentation. In those with previous pregnancies and childbirths only, 1 had history of fetal malformation, while 3 had family history of congenital malformations. Details are shown in Table 2.
| Variables |
n (%) |
| Contraception (n) |
65 |
| Missing |
9 |
| Yes |
7 |
| No |
49 |
| Type of contraceptives |
| None |
50 |
| Barrier method |
4 |
| Combined oral contraceptives |
1 |
| Other |
15 |
| Pregnancy planned (n) |
65 |
| Missing |
9 |
| Yes |
34 |
| No |
25 |
| Pre-conception counseling (n) |
65 |
| Missing |
11 |
| Yes |
20 |
| No |
34 |
| Use of folic acid |
| Yes |
55 |
| No |
10 |
Table 2: The demographics of pre-conceptual matters.
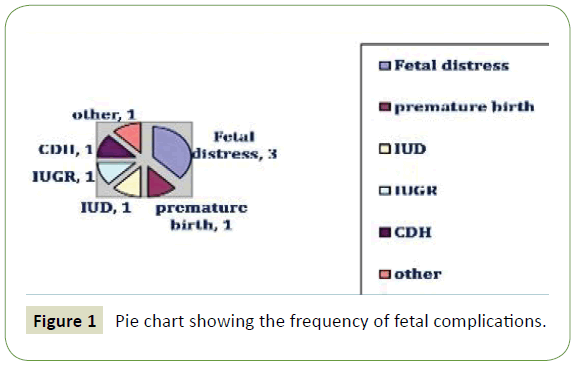
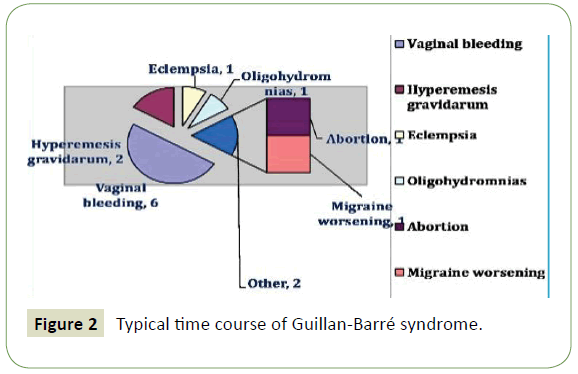
Events related to birth showed 13 abortions, 18 had complicate pregnancy with most common issue being fetal distress. Other issues observed were vaginal bleed, hyperemesis gravidarum, intrauterine growth retardation, intrauterine death, eclempsia, oligohydromnias, and premature birth. Majority of the female epileptic underwent cesarean section or had episiotomy with only 9 undergoing normal vaginal delivery. In 8 cases there were complications related to labor. Details are shown in Figures 1 and 2.
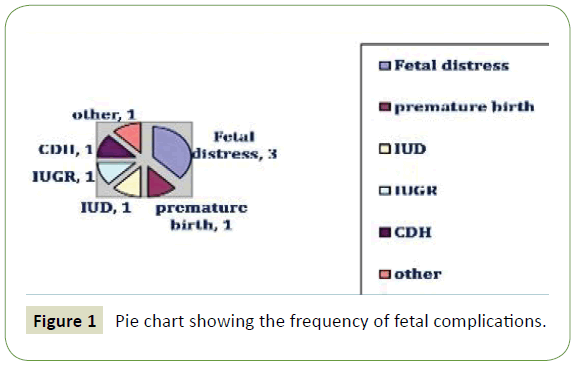
Figure 1: Pie chart showing the frequency of fetal complications.
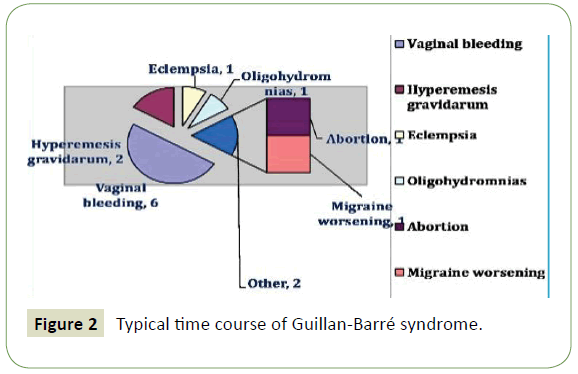
Figure 2: Typical time course of Guillan-Barré syndrome.
Regarding the fetus, majority 41 had APGAR (Airway, pulse, grimaces, activity, respiration) score above 7 at 5 and 10 minutes. 1 patient had APGAR score of 6 at 5 minutes which improved to score of 7 at 10 minutes. In 30 neonates APGAR sore increased from 5-10 minutes by score of 1. 1 patient had drop in APGAR score of 1 from 5 to 10 minute but remained uneventful. 11 participants have unchanged APGAR score at 5-10 minutes. Mean APGAR score at 5 minutes was 7 ± 0.5 and mean APGAR sore at 10 minutes was 8 ± 0.7. Table 3 shows the details of APGAR scores.
| Variables |
n |
| Total (n) |
42 |
| Missing |
23 |
| Mean APGAR score at 5 minutes |
7 ± 0.5 |
| Mean APGAR score at 10 minutes |
8 ± 7.0 |
| APGAR score less than 7 |
1 |
| APGAR score 7 or more |
41 |
| Increase in APGAR score from 5-10 minutes |
30 |
| Unchanged APGAR score from 5-10 minutes |
11 |
| Decrease in APGAR score from 5-10 minutes |
1 |
Table 3: APGAR score of the neonates born to epileptic mothers at and 10 minutes after the birth.
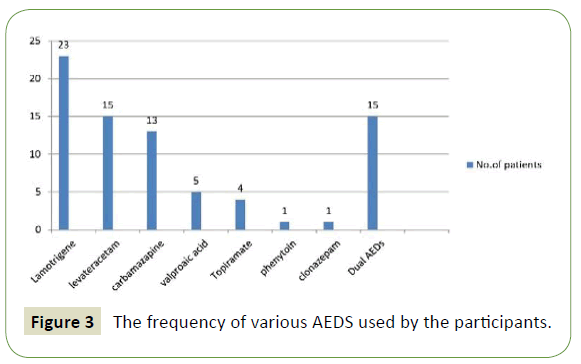
Most common drug was Lamotrigene followed by Levateracetam and Carbamazapine. Valproic acid, Topiramate, Phenytoin and Clonazepam were less commonly used by the participants. About 15 of the patients were on polytherapy. Statistics are shown in Figure 3.
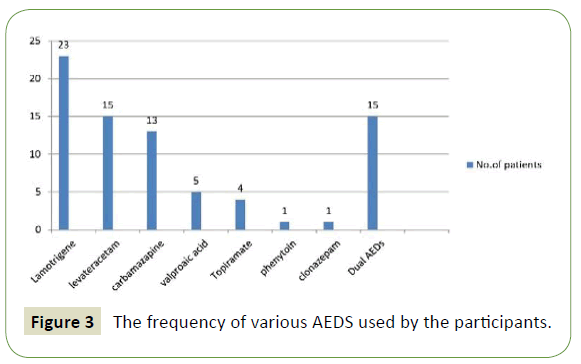
Figure 3: The frequency of various AEDS used by the participants.
When participants in the monotherapy group were compared with those in polytherapy group, polytherapy group was found to have higher rate of abortions (33 vs. 14). Similarly, the birth defects in the offspring of the previous pregnancies were high in polytherapy group (13 vs. 2). There was high rate of cesarean section in polytherapy group compared to all monotherapies combined (53 vs. 48).
Vaginal bleed, IUD (Intrauterine death), oligohydromnias, congenital diaphragmatic hernia was high in polytherapy group while fetal distress, IUGR (Intrauterine growth retardation), hyperemesis gravidarum, preeclempsia and migraine worsening were seen commonly in monotherapy group. Table 4 shows the comparison of monotherapy vs. polytherapy group.
| Variables |
Monotherapy |
Polytherapy |
| Previous abortion |
14% |
33% |
| Complications of pregnancy |
28% |
26% |
| Complications of labor |
16% |
0% |
| History of birth defects |
2% |
13% |
| Normal delivery |
16% |
6% |
| Episiotomy |
12% |
6% |
| Cesarean |
48% |
53% |
Table 4: The comparison of monotherapy vs. polytherapy on the basis of pregnancy related complications.
Discussion
As the most female having epilepsy are those with age in first two decades. Many of them are in the reproductive period or soon have to go through this phase. Not only epilepsy itself but also the medications used for treating it may pose several threats to the fetus as well as mother. It may result in dire complications during pregnancy and perinatal period [12].
In our study only very, few participants were using any contraceptives and nearly half of the pregnancies were unplanned. Preconceptual counseling was not considered by most of the patients. About half of the participants had their first pregnancy at the presentation, while those with history of previous pregnancies about 13 had previous history of abortions, 3 had family history of malformations while malformation among the fetuses of the participants were seen only in one case. Most of the participants were using folic acid in our study. According a previous study Fifty-one percent of women between the ages of 16 and 55 stated they had not received any advice about the possible interactions between contraception and AEDs. In regard to pregnancy, 34% of women stated they had not received any advice from any health care professionals [13]. There were (66.8%) unplanned pregnancies and (33.2%) of the pregnancies were planned in advanced. The risk for spontaneous Fetal loss among the 653 unaborted pregnancies in women with epilepsy was greater for unplanned (35.0%) than planned (16.4%) pregnancies (RR, 2.14) [14].
It has been reported that women with epilepsy who were undergoing the pregnancy compared to the pregnant females without having epilepsy had increased odds of spontaneous miscarriage (OR 1.54), antepartum haemorrhage (1.49), postpartum haemorrhage (1.29), hypertensive disorders (1.37), need for the induction of labor (1.67), caesarean section (1·40), preterm birth (<37 weeks of gestation) about (1.16) and fetal growth restriction (1.26) [15].
In our study events related to birth showed 13 abortions, 18 had complicated pregnancy with most common issue being fetal distress. Other issues observed were vaginal bleed, hyperemesis gravidarum, intrauterine growth retardation, intrauterine death, eclempsia, oligohydromnias, and premature birth. Majority of the participants underwent cesarean section with only 9 having Normal vaginal delivery. In about 8 cases, the perinatal complications were observed in our study.
In our study most common AED used was Lamotrigene followed by Levateracetam and Carbamazapine. While other AEDS like Valproic acid, Topiramate, Phenytoin and Clonazepam were less commonly used by the participants. About 15 patients were using the polytherapy due to uncontrolled seizures while rests were on monotherapy.
When compared to the data available, one of the studies, reported that among the 349 pregnancies about 79.6% of the participants were exposed to AED monotherapy and 5.8% to polytherapy during pregnancy. About 14.6% discontinued AED prior to pregnancy. The most commonly used AEDs in their study were Carbamazepine (29.9%) and Valproic acid (19.7%); the most common AED polytherapy combination was Carbamazepine combined with Clobazam (2.5%) [15].
In another study, among the patients on monotherapy, 111 deliveries took place and about 9.9% were born with major congenital malformations while in those using polytherapy, 19.0% of babies had major congenital malformations. Highest incidence of fetal malformations was seen in those who discontinued AEDs prior to pregnancy (20.0%) [16].
In our study patients on polytherapy had history of high abortion rate in previous pregnancies (33 vs. 14), and history of birth defects (13 vs. 2). There was high rate of caesarian section in polytherapy (53 vs. 48). There was no difference in pregnancy related complications between the monotherapy and polytherapy group. None of the individual AED category’s differed significantly from the no AED category regarding the spontaneous fetal loss frequency [17].
Considering the less prevalent trend of preconceptual counseling and very high frequency of unplanned pregnancies and less frequent contraception uses show that the awareness among the epileptic patients regarding the interaction of epilepsy and AEDS with the mother and fetal health. Role of the health care system in making a separate clinic for such patients where obstetrical care is combined with the staff having expertise in neurology or epilepsy care are combined at a single clinic.
Important aspects that need to be addressed in this respect include the facilities of preconceptual counseling, adjustment of the AEDS doses and increase provision of information about the important issues and also giving an advice on schedule of follow up routine during the pregnancy and perinatal period. Besides above given measures increase awareness in media, newspaper and at primary health care level might be vital in improving maternal and fetal care in pregnant epileptic patients.
Conclusion
Since epilepsy is quite a stigmatized illness, many patients may hide it so that they may avoid the social, occupational consequences related to it in our society. In this regard female epileptics who are in the reproductive age are of special concern because they might not be able to assess the health care facilities and the awareness about the effects of epilepsy and AEDS on the health of not only mother but also the offspring may be insufficient. Due to lack of epilepsy related reproductive health care services low rate of preconceptual counseling, high rate of unplanned pregnancies and high rate of pregnancy and peripartum complication and fetal malformation may result. Improvement in reproductive health services and close communication between neurology and obstetrical services may help to better control the seizures and tailor the treatment adjusts it during pregnancy and labor may lead to better outcomes.
Conflict of Interest
It is stated that this study did not required any funding. It is acknowledged that none of the authors have any conflict of interest and there is nothing to disclose.
24682
References
- Khatria A, Iannacconea ST, Ilyasb MS, Abdullahb M, Saleemc S (2003) Epidemiology of Epilepsy in Pakistan: Review of literature. JPMA 53: 594.
- Luz V, John A, Cheong-See F, Arroyo-Manzano D, Dougall M, et al. (2015) Epilepsy in pregnancy and reproductive outcomes: A systematic review and meta-analysis. Lancet 386: 1845-1852.
- Delgado-Escuta AV, Janz D (1992) Consensus guidelines: Preconception counselling, management, and care of the pregnant woman with epilepsy. Neurology 42: 149-160.
- Battino D, Tomson T, Bonizzoni E, Craig J, Lindhout D, et al. (2013) Seizure control and treatment changes in pregnancy: Observations from the EURAP Epilepsy Pregnancy Registry. Epilepsia 54: 1621-1627.
- Lindhout D, Rene JE, Hoppener A, Meinardi H (1984) Teratogenicity of antiepileptic drug combinations with special emphasis on epoxidation of carbamazepine. Epilepsia 25: 77-83.
- Devinsky O, Feldmann E, Hainline B (1994) Advances in neurology. Neurological complications of pregnancy. Epilepsy and pregnancy. Raven Press, USA.
- Hiilesmaa VK, Bardy AH, Teramo K (1985) Obstetrical outcome in women with epilepsy. Am J Obstet Gynaecol 152: 499-504.
- Campbell E, Kennedy F, Russell A, Smithson WH, Parsons L, et al. (2014) Malformation risks of antiepileptic drug monotherapies in pregnancy: updated results from the UK and Ireland Epilepsy and Pregnancy Registers. J Neurol Neurosurg Psychiatry 85: 1029-1034.
- Hernández-Díaz S, Smith CR, Shen A, Mittendorf R, Hauser WA, et al. (2012) Comparative safety of antiepileptic drugs during pregnancy. Neurology 78: 1692-1699.
- Tomson T, Battino D, Bonizzoni E, Craig J, Lindhout D, et al. (2011) Dose-dependent risk of malformations with antiepileptic drugs: An analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol 10: 609- 617.
- Cunnington MC, Weil JG, Messenheimer JA, Ferber S, Yerby M, et al. (2011) Final results from 18 years of the International Lamotrigine Pregnancy Registry. Neurology 76: 1817-1823.
- Kinney MO, Craig JJ (2017) Pregnancy and epilepsy: Meeting the challenges over the last 25 years: The rise of the pregnancy registries 44: 162-168.
- Leonardi M, Ustun TB (2002) The global burden of epilepsy. Epilepsia 43: 21-25.
- Robert E, Guibaud P (1982) Maternal valproic acid and congenital neural-tube defects. Lancet 2: 937.
- Tomson T, Battino D, Bonizzoni E, Craig J, Lindhout D, et al. (2011) EURAP study group. Dose-dependent risk of malformations with antiepileptic drugs: An analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol 10: 609-617.
- Herzog AG, Mandle HB, MacEachern DB (2019) Association of unintended pregnancy with spontaneous fetal Loss in women with epilepsy: Findings of the Epilepsy Birth Control Registry. JAMA Neurol 76: 50-55.