Keywords
Appendectomy; Acute appendicitis
Introduction
Appendicitis is the most common surgical disease with appendectomy being the traditional treatment of choice. The diagnosis of Acute Appendicitis (AA) was based on clinical signs and symptoms before the advent of widespread use of sonography and CT scans. Several diagnostic scoring systems such as Alvarado score, AIR-Appendicitis Inflammatory Response (Andersson score), World Society of Emergency Surgery (WSES) AA grading system have been described [1].
Obstruction of the lumen of appendix triggers a series of events that leads to Acute Appendicitis. Fecalith is the most common cause of obstruction, others being lymphoid hyperplasia, oedema, stricture, gallstones, adhesions etc. [2]. Emergency Appendectomy was the choice of treatment for AA initially and any sort of delay in operative intervention was believed to lead to complications like perforation, periappendiceal abscess etc. However, studies have shown that delayed appendectomy though less superior, does not lead to increased morbidity [3].
Different operative procedures exist for appendectomy such as open appendectomy, laparoscopic appendectomy, Single Incision Laparoscopic Surgery (SILS)/ Single Port Laparoscopy (SPL) and via transvaginal route (Notes: Natural Orifice Transluminal Endoscopic Surgery). The idea of minimal access surgery has made laparoscopy a far more attractive option than the open approach. However, many studies have shown conflicting results. Some have demonstrated that laparoscopic route has better clinical outcomes while other has shown marginal or no clinical benefits and higher costs. Thus, there is no single consensus regarding the superiority of laparoscopic route over open [4]. However, there is a growing trend towards minimal access surgery (laparoscopy) due to the reduced magnitude of surgical injury and enhanced rate of patient’s return to homeostasis and recovery.
Open appendectomy is considered safe and effective but associated with complications such as ileus, intestinal obstruction, wound sepsis etc. Laparoscopic appendectomy with high accuracy and low complication rate has emerged as the modus operandi for both diagnosis and treatment of Acute Appendicitis (AA) [5].
Aim
To determine the clinicopathological patterns of AA and retrospectively analyze its operative outcome.
Objectives
• To correlate the different diagnostic features of AA
• To correlate different intra-operative findings during appendectomy
• To analyze the operative outcome in the follow-up period
Material and Methods
This is a retrospective study done between January 2018 till January 2020 in a tertiary care hospital of Central India. A total of 634 patients were analyzed with AA as diagnosis. All patients who were operated for appendectomy, whether laparoscopic or open, were enrolled in the study. Record was obtained from online patient data entry and from offline individual case files.
Demographic data such as age and sex along with clinical features and investigative findings were all collected and compiled. Data regarding patient follow-up for post-op complications like wound sepsis, intra-abdominal abscess, ileus, intestinal obstruction etc. was collected from online record entry.
Following diagnostic criteria was used:
• Migratory right iliac fossa (RIF) pain
• Anorexia
• Nausea and vomiting
• RIF tenderness
• Rebound tenderness
• Elevated temperature
• Leukocytosis
• Shift to left
All routine lab investigations were done along with sonography. Choice of appendectomy, whether laparoscopic or open, was based on clinical judgement of operating surgeon. All samples were sent for histopathological reporting. Final diagnosis was made with the help of intra-operative findings and histopathological reports.
Statistical analysis
Data was analyzed with of Open Epi version 2.3. Continuous variables are presented as mean ± SD, and categorical variables are presented as absolute numbers and percentage. The comparison of normally distributed continuous variables between the groups was performed using Student’s t -test. Nominal categorical data between the groups were compared using Chi- squared test. For all statistical tests, a p-value less than 0.05 were taken to indicate a significant difference.
Results
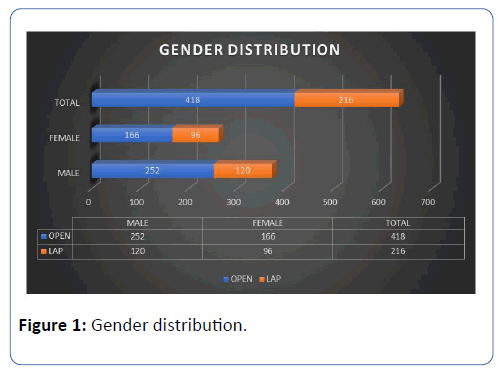
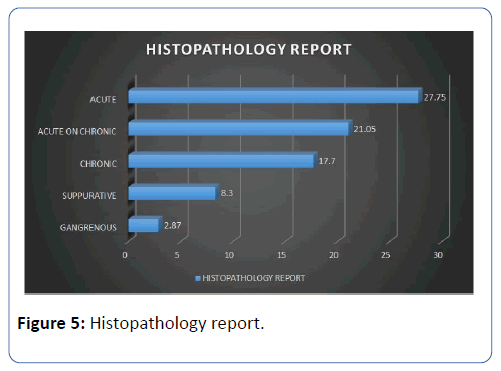
A total of 634 patients were operated for appendectomy out of which 418 were via open approach and 216 were via laparoscopy. In the open appendectomy group, 252 were males and 166 were females, whereas in laparoscopic appendectomy, males and females were 120 and 96 respectively (Figure 1).
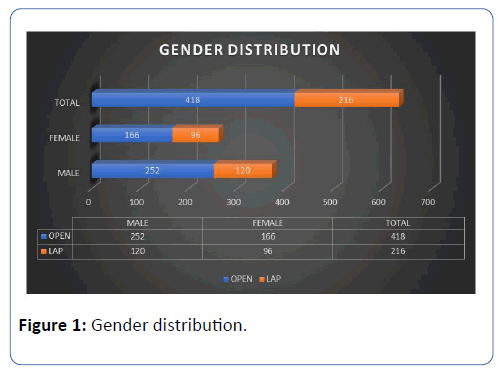
Figure 1: Gender distribution.
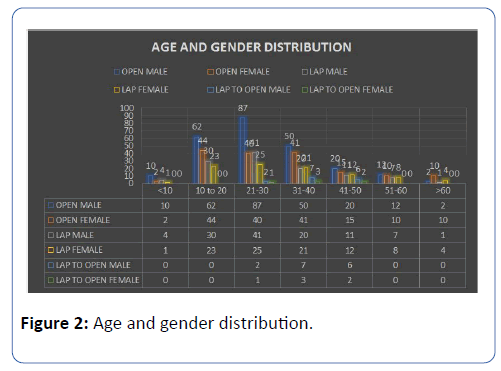
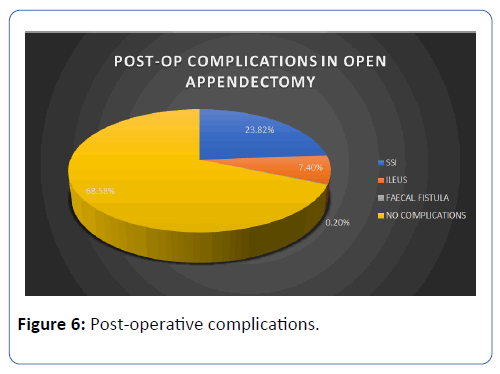
The average age for males and females in open appendectomy was 28.23 ± 12.42 (Mean ± SD) and 31.22 ± 14.77 respectively. In laparoscopic, the average age for males and females was found to be 30.46 ± 11.66 and 32.21 ± 13.33 respectively (Figure 2).
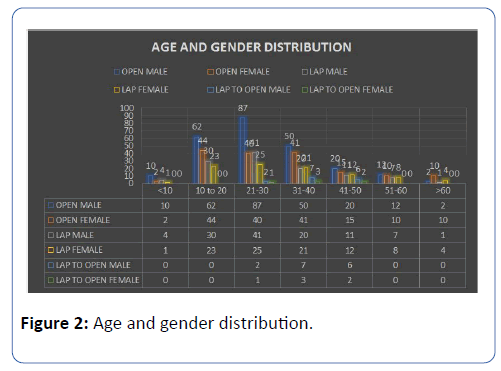
Figure 2: Age and gender distribution.
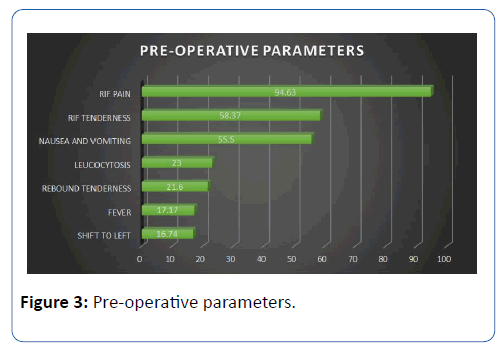
Most common symptom for appendicitis was found to be pain in abdomen in right iliac fossa (94.63%), followed by nausea and vomiting (55.5%). Fever was present in 17.17% patients. Most common sign was tenderness in right iliac fossa (58.37%) followed by rebound tenderness (21.6%).
Amongst the laboratory parameters, leukocytosis was found in 23% followed by shift to left (16.74%) (Figure 3).
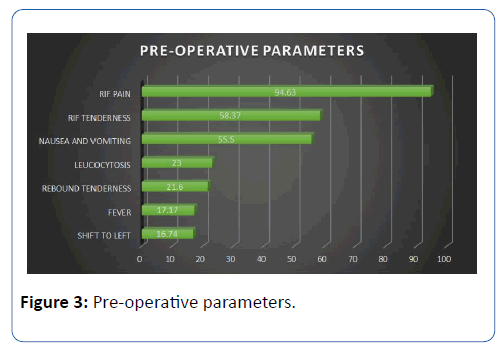
Figure 3: Pre-operative parameters.
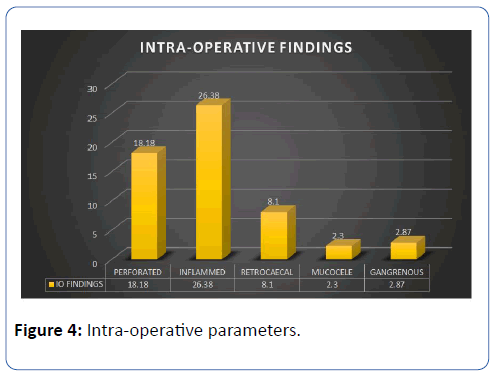
From an intra-operative point of view, 18.18% patients had a perforated appendix, 26.38% had mild to moderately inflamed appendix, 8.1% had retrocaecal appendix and only 2.3% had mucocele appendix (Figure 4).
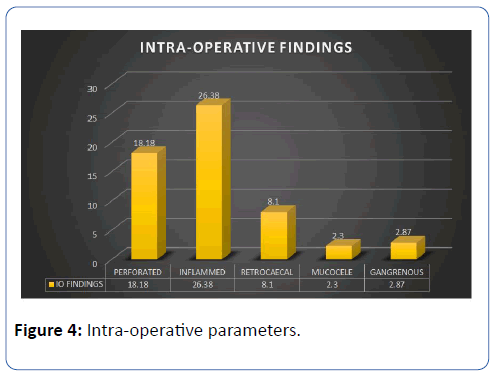
Figure 4: Intra-operative parameters.
Histopathological assessment of all the appendix specimens showed that 27.75% had acute appendicitis, 17.7% had chronic appendicitis, 21.05% had acute on chronic appendicitis, 8.3% had suppurative appendicitis and 2.87% had gangrenous appendicitis (Figure 5).
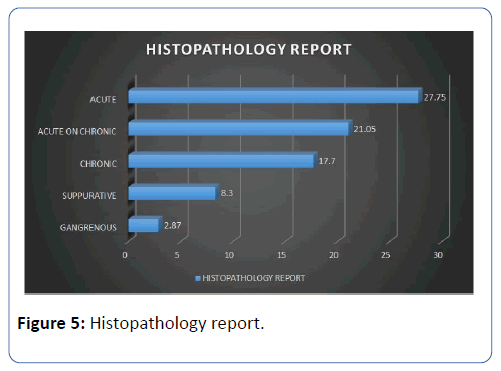
Figure 5: Histopathology report.
287 out of 418 patients who underwent open appendectomy had post-operative complications. 23.82% of the OA cases reported with surgical site infection (SSI) in the form of wound gape in the follow-up period which was then treated with either re-suturing or healing by secondary intention with regular cleaning and dressing. Amongst patients who underwent open appendectomy, post-op ileus was encountered in 7.4% and faecal fistula was reported in only 1 patient (0.2%). No post-op complication was reported in the laparoscopic group (Figure 6).
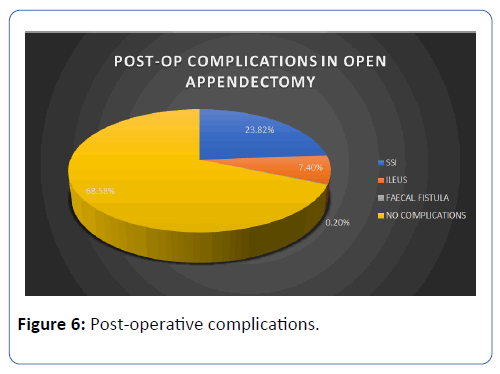
Figure 6: Post-operative complications.
Post-op duration for open and laparoscopic appendectomy was 4.91 ± 0.86 and 2.98 ± 0.76 (p-value=0.04150) and was found to be statistically significant.
Discussion
Dr. Ekka et al. studied the clinical presentation of 125 patients for a period of 2 years [6]. Alvardo scoring in the evaluation of acute appendicitis was studied by Dr. Özsoy et al. [7] amongst 156 patients and by Dr. Mahesh et al. [8] amongst 50 patients. The comparison of their findings with our present study is shown in Table 1.
| Variables |
Present study |
Dr. Ekka et al. |
Ã?zsoy et al. |
Mahesh  et al. |
| Total (n) |
634 |
125 |
156 |
50 |
| RIF pain (%) |
94.63 |
100 |
100 |
100 |
| RIF tenderness (%) |
58.37 |
89.6 |
80.12 |
100 |
| Nausea/ vomiting (%) |
55.5 |
84 |
43.58 |
84 |
| Rebound tenderness (%) |
21.6 |
72.8 |
74.35 |
74 |
| Fever (%) |
17.17 |
68 |
9.61 |
62 |
| Leucocytosis (%) |
23 |
66.4 |
50.64 |
62 |
| Shift to left (%) |
16.74 |
79.2 |
44.87 |
48 |
Table 1: Comparison of pre-operative clinical features of acute appendicitis.
A retrospective study conducted by Ioannis et al. in 2018 showed that although OA is easy and fast, LA becomes more minimal with the one port technique and operative time also reduces after training. LA was recommended as a routine surgical technique [9]. Although operative time was not a parameter evaluated in our current study, it can be concluded that laparoscopic approach fares better than open appendectomy based on other studied factors.
Retrospective data from 593 patients was collected by Biondi et al. in 2016 and was compared for operative time, length of hospital stay, postoperative pain, complication rate, return to normal activity and cost. It was found that in LA, hospital stay was shorter (2.7 ± 2.5 days) with faster return to normal activity (11.5 ± 3.1 days) although total operative time for LA was more (31.36 ± 11.13 min in OA and 54.9 ± 14.2 in LA). Incidence for intra-abdominal abscess was found to be more in LA but it could be reduced with training and experience. Both procedures are still in practice with surgeon’s choice being the decisive factor [10]. No intra-abdominal abscess was reported in our study. However, other post-op complications were present after open appendectomy like surgical site infections (SSI), ileus, fecal fistula etc. whereas none were reported after laparoscopic approach.
Khatana conducted a similar study in 2018. The study concluded that although post-op pain was more in OA, nausea was more pronounced in the laparoscopic group. No significant difference was found in the rest of the post-op complications. Even post-op stay duration was found to be statistically insignificant. Thus, the results of LA were comparable to OA, if not better [11]. In our study, laparoscopic approach was reserved only for elective cases while all the emergency appendicitis cases were treated with open appendectomy. Cases posted electively who had significant guarding and rigidity and had been given a trial of antibiotics were also treated by open appendectomy.
A prospective study was conducted in 2015 amongst 187 patients. No significant difference was found with regards to hospital stay, post-op analgesia, return of bowel sounds and to daily activity. Cost of LA was more than OA. It was concluded that appendicectomy in acute uncomplicated appendicitis was a safe procedure, regardless of the technique involved [12]. Post-op recovery was found to be better after LA in our study while being a government sector, cost was almost equal for both the procedures.
Shimoda et al. conducted a study in 2017 with statistically significant difference found in duration till resuming oral intake, blood loss and surgical site infection. Although operating time is longer with LA, it can be reduced with proper training and further experience [13]. Operating time not only depends upon surgeon experience but also upon the complications that might occur during the procedure. Thus, it is difficult to have a uniform comparison between operative time of two different techniques as it is impossible for every intra-operative encounter to be similar.
763 appendectomies were conducted and studied between 2007-20012 and analyzed by Islam et al. Conversion of lap to open was found in 11 cases (3.4%). Concomitant pathologies were encountered and subsequently managed including 10 cholecystectomies, 4 tubal pregnancies and 6 ovarian cystectomies. No such events were encountered in the present study [14].
70 patients were analyzed for pre-op, intra-op and post-op parameters during 2013-2014 by Subramaniam et al. Operative time and total blood loss was slightly more in OA as compared to LA. Early discharge from hospital was found in LA cases. Zero mortality was found in all the cases. LA was safe and feasible in complicated appendicitis [15].
Shrivastava et al. studied 80 patients in 2019. Intraoperatively, retrocaecal appendix was found in 51 cases. Operative time was more in LA and significant difference was found in post-op complications. 47.5% OA and 25% LA cases had post-op complications. Wound infection was seen in 25% OA and 13.9% LA cases. Almost all LA patients were satisfied with post-op scars and recovery [16]. In the current study as well, patient satisfaction was found to be better with the laparoscopic approach especially when it came to female rural population. Despite giving subcuticular skin stitches in some of the uncomplicated open appendectomy cases, patient’s feedback was less positive in comparison to laparoscopic postop scars. Laparoscopic approach was safer and more feasible according to certain studies with lower 30-day readmission rate, less post-op pain and less hospital stay. Some studies concluded that it was safer than OA. However, according to other studies there was no significant advantage of LA over OA except quality of life at 2 weeks. LA also took longer to perform. Thus, the decision between whether to perform OA or LA depended upon the surgeon or patient or both. [17-20].
In 2018, Patel et al. conducted a study on 88 patients (65 OA and 23 LA). Mean age was found to be 27.83 and 27.28 years respectively. 4 were interval and 19 were emergency appendectomies which were performed on patients with recurrent symptoms. Out of all the OA cases, 27 were acute appendicitis, 20 were recurrent appendicitis and remaining 18 were interval appendectomies [21]. In the present study, 27.75% had acute appendicitis, 17.7% had chronic appendicitis, 21.05% had acute on chronic appendicitis, 8.3% had suppurative appendicitis and 2.87% had gangrenous appendicitis.
Goudar et al. conducted a study in Southern India amongst 240 patients. Post-op pain was stratified into mild, moderate and severe and was found to be less in LA. Wound infection was found to be statistically insignificant between the 2 groups but stump appendicitis was found in one patient who had undergone LA. No case of stump appendicitis was encountered in the present study. 3 patients had negative appendectomies out of which 2 had ovarian torsion and 1 had Meckel ’ s diverticulitis. No negative appendectomies were encountered in our study [22].
In a study done by Mukherjee et al. in a rural district setup in India statistical significance with p-value <0.0001 was found comparative entities such as mean incision length in cm, mean duration of surgery in minutes, mean parenteral analgesic doses, mean oral analgesic doses, time to start oral feeding in hours, time to ambulation, post-op pain after 24 hours, hospital stay in days, patient acceptance likert scale and nonsignificance was found in intra-op and post-op complications [23]. Mehta et al. studied 50 consecutive cases in a rural population. They reported that all the patients presented with complaint of abdominal pain, 64% amongst OA and 80% amongst LA presented with nausea/ vomiting. 28% OA and 20% LA cases complained of fever at the time of admission. All the patients showed tenderness on palpation while guarding/ rigidity was present in 24% OA and 16% LA cases. 80% and 72% of OA and LA patients showed differential count with shift to left [24]. Similarly in our study, RIF pain and tenderness featured prominently amongst patient ’ s chief complaints whereas shift to left was seen in 16.74%.
100 appendicitis patients were studied by Mehta et al. during 2016-2017 out of which 55% LA and 60% OA cases had inflamed appendix, 25% LA and 20% OA had adhesions, 2.5% LA and 5% OA had appendicular lump, 12.5% LA and 6.76% had OA had distended appendix, 10% LA and 8.3% OA had appendicular perforation while the rest were normal [25].
Post-op complications were studied by G. Kumar in 200 cases. 20% and 10% OA and LA cases respectively had vomiting. Abdominal abscess was found to be a complication in 5% OA cases while no such complication had occurred in LA cases. Wound infection occurred in 17% open and 4% of laparoscopic cases. Ileus was found in both but was less in laparoscopic group [26].
820 appendectomies were analyzed over a period of 5 years by Senapati et al. In the laparoscopic group, injury to inferior epigastric artery due to trocar occurred in 2 cases while in 13 cases, the approach became difficult due to dense adhesions and was subsequently converted to open. 21 cases reported with surgical site infection amongst the open group. 6 cases reported with surgical site hernia amongst open cases and 2 laparoscopic cases presented with umbilical port hernia [27].
Conclusion
On the basis of the current study, it can be concluded that laparoscopic appendectomy is a safe and efficient technique for appendicitis. Visualization of abdomen intra-operatively for different pathologies, better cosmesis, patient satisfaction and less post-operative complications are its main advantages. Laparoscopic setup and its maintenance leading to higher costs are their biggest con which has to be bear either by the institute or the patient. Both the procedures are still widely practiced. Laparoscopic approach should be considered as the initial management especially in suspicious cases. Thus, the ultimate operative choice is entrusted to patient decision and the clinical knowledge and skill of the operating surgeon. In the future, laparoscopy has a greater scope and could become the gold standard for appendicitis.
Conflicts of Interests
The authors declare no conflict of interest
Funding
No funding was received.
31018
References
- Kotwal SR, Jadav SJ (2018) Retrospective study of single dose of antibiotic in laparoscopic appendicectomy. Int Surg J 5: 1897.
- Shin CS, Roh YN, Kim JI (2014) Delayed appendectomy versus early appendectomy in the treatment of acute appendicitis: A retrospective study. World J Emerg Surg 9: 1-5.
- Kehagias I, Karamanakos SN, Panagiotopoulos S, Panagopoulos K (2008) Laparoscopic versus open appendectomy: Which way to go ? World J Gastroenterol 14: 4909-4914.
- Islam SR, Pasha K, Rahman S, Nasir E, Hanif E, et al. (2014) Laparoscopic vs. open appendectomy: A comparative study. Bangladesh J Endosurgery 2: 5-8.
- Ekka NMP (2016) A clinicopathological study of acute appendicitis in Eastern India. Int J Med Dent Sci 5: 1145.
- Özsoy Z, Yenidoğan E (2017) Evaluation of the Alvarado scoring system in the management of acute appendicitis. Turk J Surg 200-204.
- Mahesh SV, Hota PK, Sneha P (2016) A study of Alvarado score and its correlation with acute appendicitis. Int Surg J 3: 1950-1953.
- Valioulis I, Constantinos F (2018) Comparison between open and laparoscopic appendectomy: A systematic review. World J Surg Surgical Res 1: 1004.
- Biondi A, Stefano C Di, Ferrara F, Bellia A, Vacante M, et al. (2016) Laparoscopic versus open appendectomy: A retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg 11: 4-9.
- Khatana PS, Kumar J, Aggarwal M (2018) Comparison of open versus laparoscopic appendectomy. Int J Res Med Sci 6: 2133-2137.
- Karatparambil A, Kummankandath SA, Mannarakkal R, Nalakath MR, Babu D (2016) Laparoscopic versus open appendicectomy: A comparative study. Int J Surg Sci 3: 128-134.
- Shimoda M, Maruyama T, Nishida K, Suzuki K (2018) Comparison of clinical outcome of laparoscopic versus open appendectomy, single center experience. Heliyon 4.
- Islam S, Pasha K, Rahman S, Nasir E, Hanif E (2014) Laparoscopic vs. Open Appendectomy: A Comparative Study. Bangladesh Journal of Endosurgery 2: 5-8.
- Ravichandran KS (2018) Surgery Comparative Analysis of Clinical Outcomes of Open Appendectomy and Laparoscopic Appendectomy. International Journal of Contemporary Medical Research 5: 18-20.
- Shrivastava A, Jain A, Jain R (2019) Laparoscopic versus conventional open appendicectomy: A prospective comparative analytical study in a tertiary care set up. Int J Res Med Sci 7: 2536-2541.
- Study APRD (2005) Laparoscopic Versus Open Appendectomy. 242: 439-450.
- Pradhan S, Shakya YR, Batajoo H, Malla B, Joshi HN, et al. (2015) Laparoscopic versus open appendectomy: A prospective comparative study. JSSN 18: 29-32.
- Hospital Q, Univeristy S (2017) Open Appendectomy for Acute Appendicitis in Children.
- Wang C, Tu C, Wang P, Lin H, Wei P (2013) Outcome Comparison between Laparoscopic and Open Appendectomy: Evidence from a Nationwide Population- Based Study. PLoS One 8: 1-7.
- Vishnu Kumar P, Sharma S, Gaharwar APS, Gupta R (2018) A Comparative Study Between Laparoscopic Appendectomy and Conventional Open. J Surg 4: 1-6.
- Goudar BV, Telkar S, Lamani YP, Shirbur SN, Shailesh ME (2011) Laparoscopic versus Open Appendectomy: A Comparison of Primary Outcome Studies from Southern India. J Clin Diagn Res 5: 1606-1609.
- Setup DH (2018) A Comparative Study of Laparoscopic versus open Appendicectomy in a District Hospital Setup. J Med Sci Clin Res 6: 840-845.
- Mehta T, Nerlekar HV (2017) Comparative LA-A. Open Versus Laparoscopic Appendicectomy- A Comparative Study. J Med Sci Clin Res 05: 15795–15808.
- Singh LM, Wadiwa YS (2018) A retrospective comparative study between laparoscopic and open appendectomy in teaching hospital of India. Int Surg J 5: 3034-3037.
- Kumar GS, Rao DN (2018) Open vs. laparoscopic appendicectomy: A comparative study. Int J Surg Sci 2: 19-22.
- Senapati JN, Dash A, Hansa J (2016) Evolvement of Laparoscopic Appendicectomy in a tertiary care Teaching hospital. Bull Env Pharmacol Life Sci 5: 35-39.