Ravishankar, SN1*, Madhuvan, HS2, Vishal3, Thimma Reddy2, Vijaya Prabha2, Dinesh, S R1
1 Associate Professor, Dept. of Medicine, Department of General Medicine, Akash Institute of Medical Sciences and Research Centre, Devanahalli, Bengaluru.
2 Assistant Professor, Dept. of Medicine,Department of General Medicine, Akash Institute of Medical Sciences and Research Centre, Devanahalli, Bengaluru.
3 Assistant Professor, Dept. of Psychiatry Department of General Medicine, Akash Institute of Medical Sciences and Research Centre, Devanahalli, Bengaluru.
- *Corresponding Author:
- Ravishankar, SN
Associate Professor, Dept. of Medicine
Department of General Medicine, Akash Institute of Medical Sciences and Research Centre
Devanahalli, Bengaluru
E-mail: dr.ravishankar.sn@gmail.com
Keywords
Diabetes Mellitus, Montgomery Asberg Depression Scale -MADRS, Depression, Co morbidity.
Introduction
Diabetes Mellitus is one of the most devastating chronicediseases and affects virtually each and every organ of the human body. The prevalence of Diabetes worldwide is projected to rise from 2.8% in 2000 to 4.4% in 2030. India has the largest number of diabetic patients making it a capital for Diabetes. The rising prevalence has mainly been attributed to the rapid urbanization and economic development. Indians have the phenotype characterized by low BMI and high upper body adiposity, high body fat, high level of Insulin resistance, increasing their proneness for Diabetes.
Depression is a major public health problem associated with substantial suffering, reduced functioning, decreased quality of life along with higher health care utilization and costs and disability. In general, depression I associated with chronic illness and in Diabetes in particular. WHO survey has shown that co morbid state of depression with chronic illness incrementally worsens the health.
The co existence of Diabetes and depression is associated with significantly increases risk of morbidity and mortality. Therefore the co-occurrence of these two dreaded diseases has caused a heavy burden to the society.
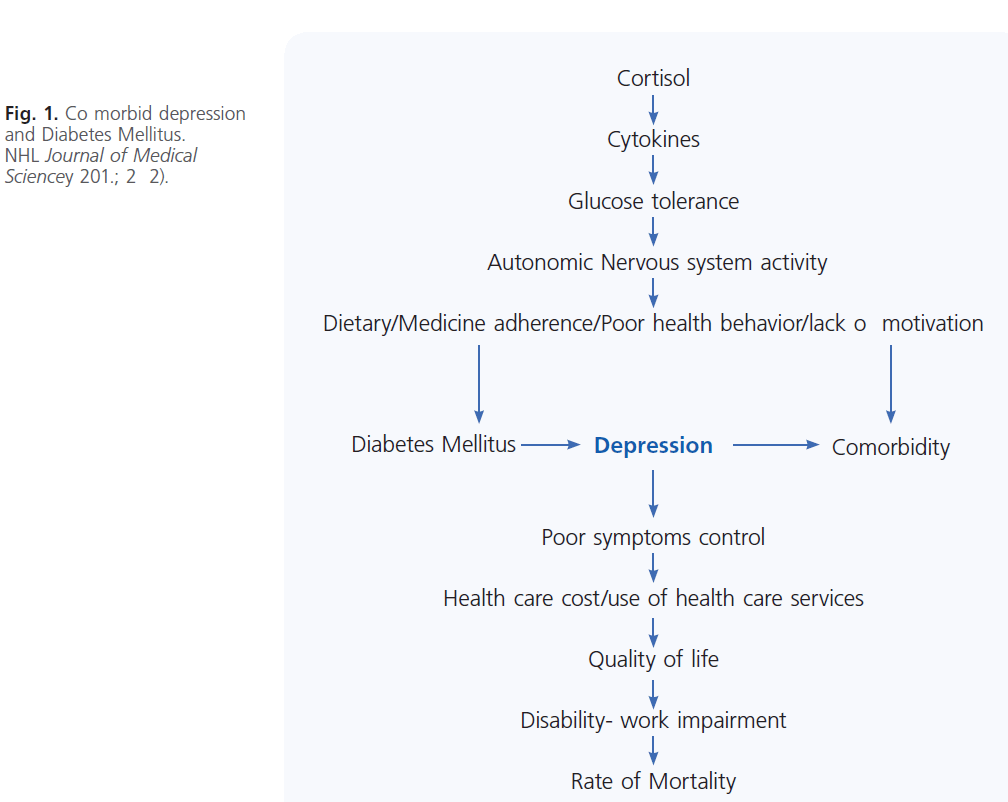
The relationship between Diabetes and depression has been argued to be essentially bidirectiona. Fig. 1.
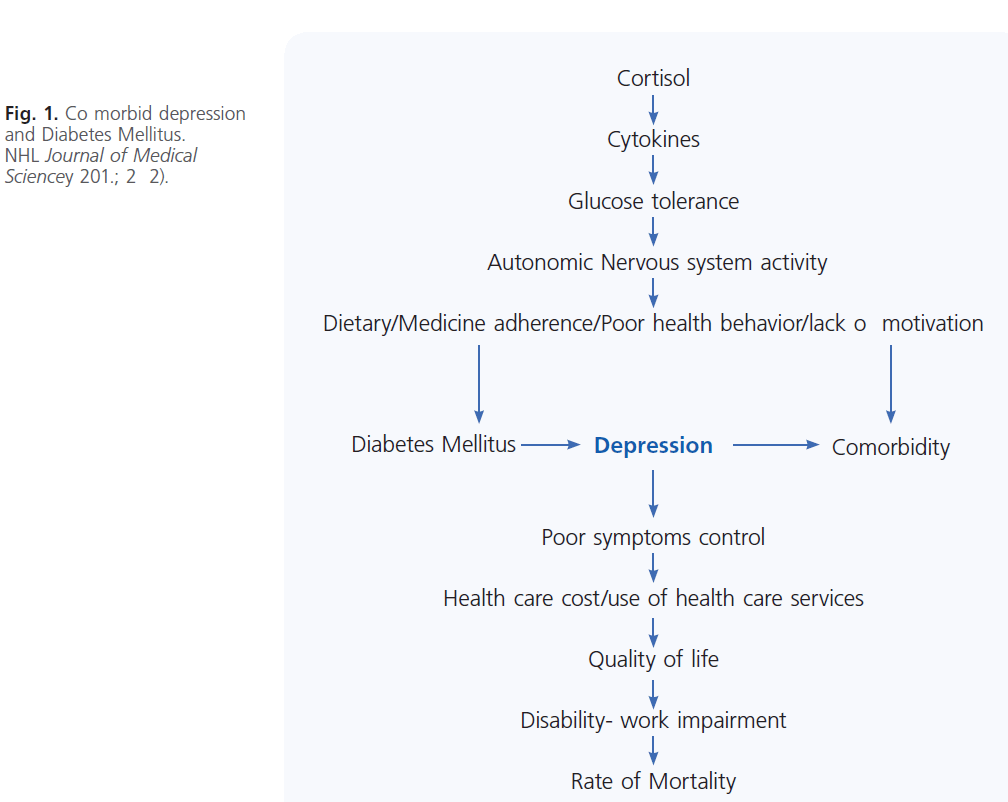
Figure 1: Representative example of a successfully implanted CRT system with four leads. Fluoroscopic image in anteriorposterior view showing a single right atrial appendage lead (RAA); two right ventricular leads (right ventricular septal close to His Bundle [RVH] and right ventricular apex [RVA]) and lateral left ventricular lead (LV).
Depression associated with hyperglycemia and persistent elevation of HbA1C, may not be due to the direct effect on glycemic control, rather the relationship is indirect via self care behaviors.
The development of depression has often been considered as a secondary response to the onset of complications, but depression might also play a primary role in the development of Diabetic complications.
Effective treatment for depression by psychological/ pharmacological methods not only improve the depression symptoms but also has a positive impact on the glycemic control, behavioral risk factors which can drastically improve health and reduce the rate of morbidity and mortality due to Diabetes.
Materials and Methods
The prevalence study was conducted in Akash Hospital (AIMS& RC), Dept of Medicine, Devanahalli, including both IP/OP Diabetic patients. The total study sample comprised of 500 patients aged 30- 70 years with majority of the cases between 50 to 60 years. Selected by means of simple random sampling method. The study was conducted with getting the detailed history of Diabetes and examination of the patient and the laboratory report of blood sugars. The co morbidities and any Diabetic complications were taken into consideration. After obtaining consent from the patient they were given the MADRS questionnaire which was 10 items self report instrument intended to assess the existence and the severity of symptoms of depression. The score up to 15 was normal; 15-24 suggests mild depression, 25-30 as moderate depression, > 30 as severe depression.
Results
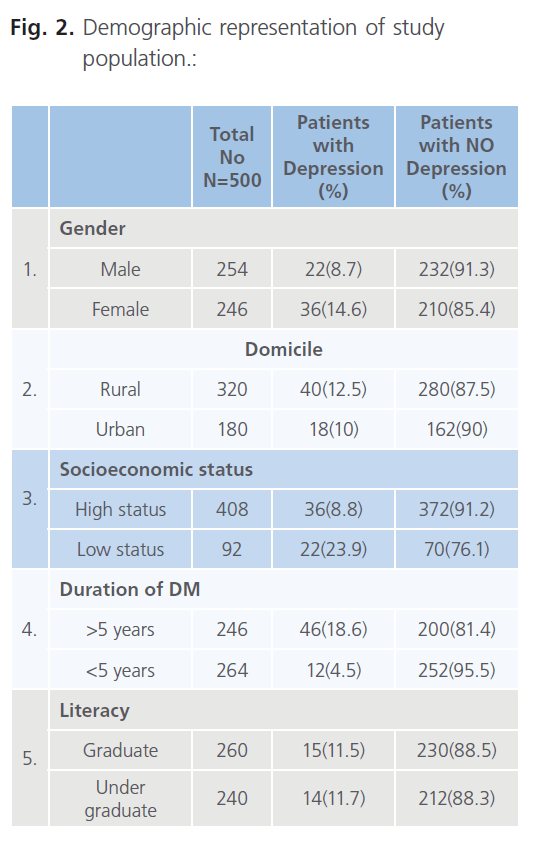
Five hundred patients suffering from Type 2 DM completed questionnaire were analysed. The prevalence of depression as per MADR scale was 11.6% according to the age group of 30-70 years with majority of cases between 50-60., i.e 58 patients out of 500 as shown in the table Fig. 2.
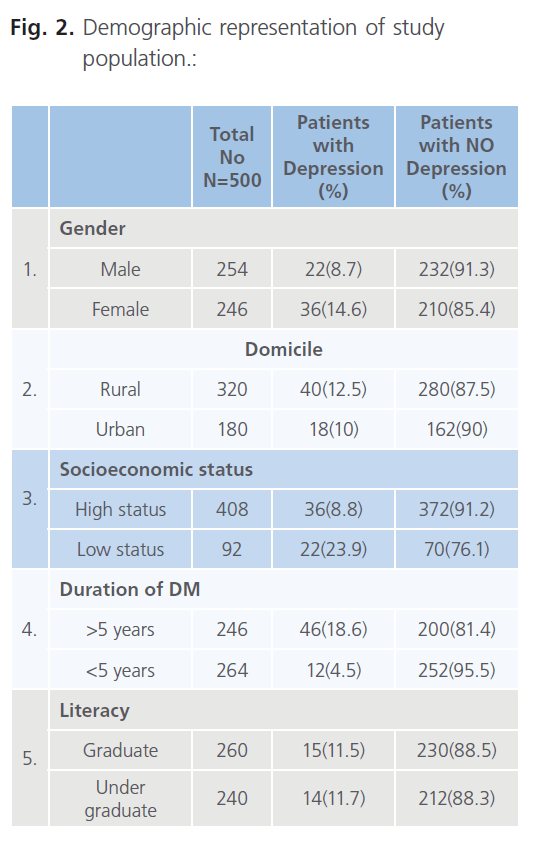
Figure 2: Demographic representation of study population.:
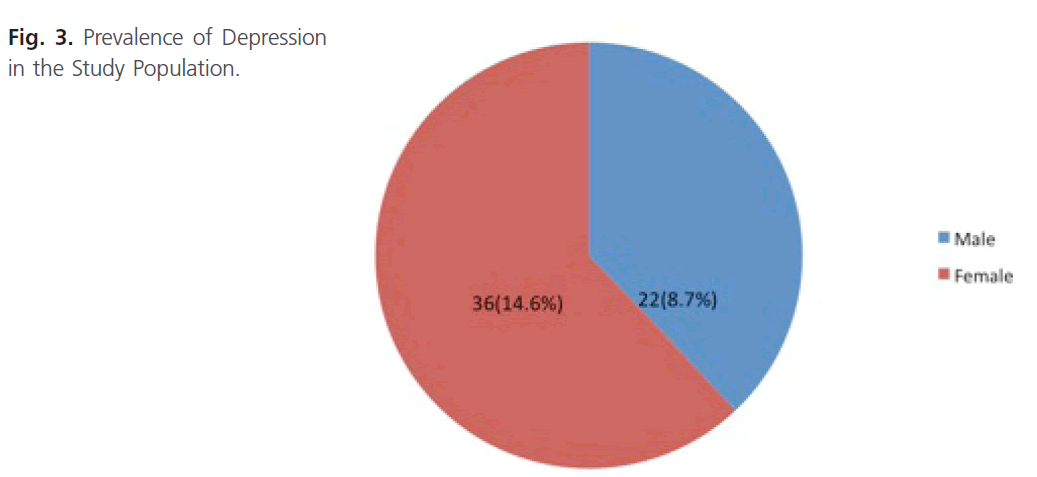
The study included 254 male pts, 246 female pts, out of which 22 (8.7%) male and 36 (14.6%) female were found to have co morbid depressio. Fig. 3).
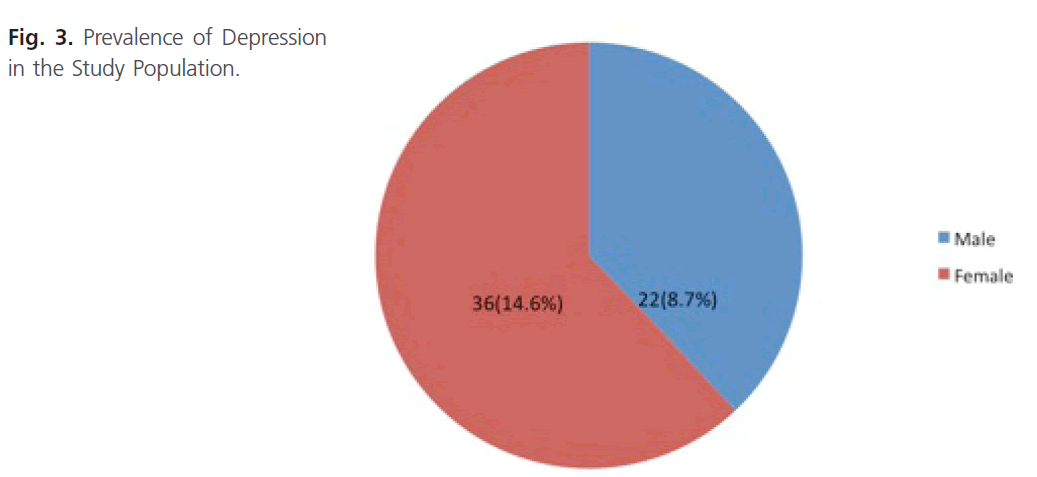
Figure 3: Prevalence of Depression in the Study Population.
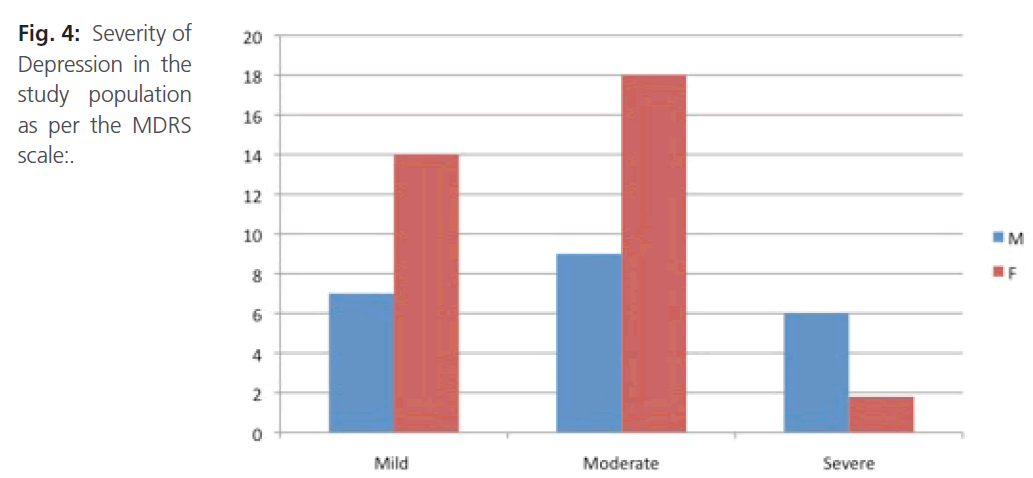
In the analysis, on the grounds of parameters of gender the frequency of depression was more in females (14.6%), when compared to men (8.7%). As per domicile stratification, out of 320 rural pts 40 (12.5%) were detected as depression, out of 180 urban pts 18 (10%) had depression. Depression was more prevalent among low socioeconomic status where the no of pts were 92, out of which 22 (23.9%) suffered from depression. In high socioeconomic population out of 408, 36 (8.8%) were found to have co morbid depression. The prevalence of depression significantly increased with increase in the duration of Diabetes. Out of 58 pts 46 (79.3%) pts were of duration of more than 5 yrs had depression; wher as 12 (20.7%) had depression but the duration of Diabetes was less than 5 year. (Fig. 4).
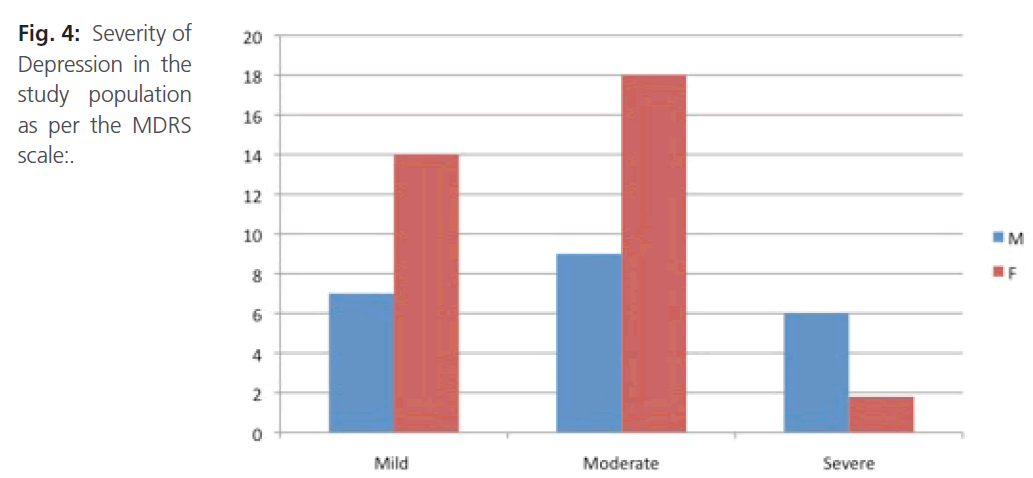
Figure 4: Severity of Depression in the study population as per the MDRS scale:.
Discussion
Diabetes Mellitus and Depression, the duo of chronic disorders are interlinked with one another where depression may contribute to the poor Diabetes control and decreased outcomes. Diabetes and its complication may also contribute to the poor management of depression.
In India, the capital for Diabetes the co morbid depression also adds on t the burden on socioeconomic status of the patient and the country. Our study aims at the finding out the prevalence of depression in Diabetic patients and to highlight the importance of detection of the co morbid state depression and to improve the patient health and socioeconomic status.
The results of the study show that more than 10% of the total study population had co morbid depression. This prevalence rate has to alert the treating Physician. It has also revealed rate of depression is higher in females than males, higher among rural population than urban, the low socioeconomic status has emerged as one of the important parameter with high prevalence of depression the duration of Diabetes increases the risk of depression. However the other physiological parameters such as BMI, Metabolic risk factors, smoking, alcohol consumption, Blood pressure were not taken into consideration.
Conclusion
The study confirms the link between Diabetes and depression where the prevalence of depression was inevitable as a co morbid condition with Diabetes. Therefore detection and management of depression in Diabetes can improve the patient’s health and decrease the economic burden on the patient and the country.
327
References
- International Diabetes Federation. The human social and economic impact of Diabetes, 2008. Available from: https:// www.idf.org/sites/default/files/Diabetes_and_Depression.pdf.
- King, H., Aubert, RE., Herman, WH. Global burden of Diabetes, 1995-2025: Prevalence, numerical estimates and projections. Diabetes care 1998; 21: 1414-31.
- World Health Organisation. Revised global burden of disease (GBD) 2002 estimates, 2005. Avialable from https://www.who. int/healthinfo/global_burden_disease/en/index.html.
- Weber, B., Schweiger, U., Deusche, M., Heuser, I. Major depression and impaired glucose tolerance. Exp Clin Endocrinol Diabetes 2000;108:187-90.
- Anderson, RJ., Freedland, KE., Clouse, RE., Lustman, PJ. The prevalence of comorbid depression in adults with diabetes: a meta analysis. Diabetes Care 2001; 24: 1069-1078.
- Egede, LE., Zheng, D. Independent factors associated with major depressive disorder in a national sample of individuals with diabetes. Diabetes Care 2003; 26: 104-111.