Margarita Peneva1*, Elizabeta Zjogovska1, Sasho Dohchev2, Sotir Stavridis2, Marija Jovanovski Srceva3, Anton Damevski3, Josif Janchulev2, Jelka Masin Spasovska4 and Goce Spasovski4
Plastic and reconstructive surgery clinic, Skopje, Macedonia, The Former Yugoslav Republic
Clinic of urology, Macedonia, The Former Yugoslav Republic
Intensive Care Unit, Macedonia, The Former Yugoslav Republic
Department of Nephrology, Medical Faculty, University of Skopje, Macedonia
Corresponding Author:
Margarita Peneva
Plastic and reconstructive surgery clinic
Skopje, Macedonia, The Former Yugoslav Republicl
Tel: 38970255303
E-mail: mapeneva@yahoo.com
Received date: November 29, 2015; Accepted date: December 08, 2015; Published date: December 15, 2015
Citation: Peneva M, A Successful Kidney Transplantation in a Patient with Multiple Perioperative Renal Transplant Complications. A Case Report. Arch Med. 2015, 8:1.
Keywords
Kidney transplantation, Surgical complications, Wound dehiscence, Plastic surgery
Background
A successful kidney transplant offers enhanced quality and duration of life and is more effective regarding the medical outcome, patient satisfaction and cost-effectiveness than longterm dialysis treatment in patients with end stage chronic kidney disease (CKD) [1]. The first kidney transplantation in our country was performed in 1977 and since then more than 360 adult and around 10 pediatric kidney transplantations have been performed [2,3]. In the last years there were major political, legislative, medical and educational initiatives adopted to improve the kidney transplant program as a routine procedure in our country [4].
Case Report
he aim of this paper is to report a case of a 24-year old male patient with end stage renal disease due to a minimal change glomerulonephritis. He has been treated many times by pulses of methyl prednisolone and maintenance corticosteroid therapy and was presented with small for date constitution (BMI of 18.3).
All pretransplant investigations have been performed and after a couple of months on dialysis he received a transplanted kidney from his father as a living donor. Although there was a slightly mismatched proportion between the donated kidney and recipient’s constitution, the graft was transplanted on the left-side with termino-terminal internal iliac anastomosis and termino-lateral external iliac vein anastomosis in the presence of short vein length. Uretero-vesical anastomosis was created according to the standard Lich-Gregoire procedure.
The postoperative recovery was accompanied by multiple complications. The first day postoperative diuresis was around 2000 ml. The ultrasound investigation showed increasing graft edema each consecutive day and Doppler signals as per insufficient renal vein outflow. The renal CT angiography confirmed partial external iliac vein thrombosis as a consequence of the left femoral vein catheter use for dialysis before transplantation. Trombectomy was performed and an intensive course of anticoagulant therapy was administered. After a couple of days with an improved graft function a gradual increase in daily proteinuria from 1.3 to 13.3 grams and diuresis reduction was noted. The ultrasonography examination showed again an edematous kidney with satisfying arterial perfusion. The graft biopsy was contraindicated because of the enormous bleeding potential and this condition was considered as an acute rejection and/or recurrence of the baseline disease. A 3-day course of methyl prednisolon 10 mg/ kg was administered and 3 plasmapharesis performed. Despite the slow improvement in the graft function and reduction of proteinuria, the parenchymal edema (23-26 mm) persisted. At the 13th postoperative day bleeding around the kidney that required surgical intervention was noted. A small graft rupture near the hillus was detected because of an external iliac vein stenosis that created a new thrombosis of the external iliac vein. Another trombectomy this time coupled with vein plasty was performed and the graft was enveloped in a vicryl mesh bag. In the following days the graft function completely recovered in the presence of insignificant proteinuria <0.5 g/day.
One week after the vascular complications were overcome the patient again decreased diuresis with a progressive and permanent graft pain. This time the CT scan confirmed ureteral necrosis with urinary fistula. The patient was operated and an anastomosis of the ureter of the graft with the contralateral native ureter of the recipient was performed.
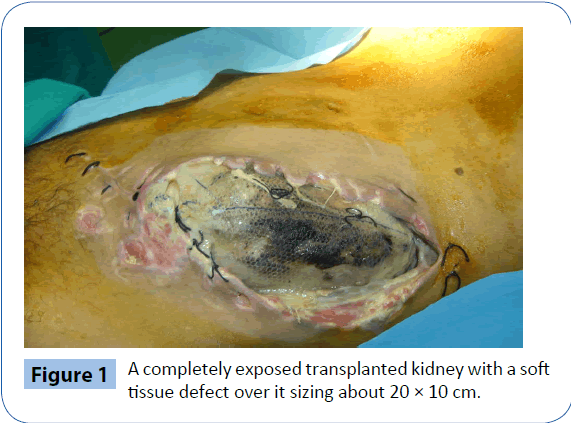
Of note, from the very beginning there was a negative size mismatch between the proportions of the transplanted kidney and the constitution of the recipient thus making the soft tissue cover over the transplanted kidney insufficient. Namely, after the transplantation the only soft tissue cover over the transplanted kidney was the skin sutured under tension. The skin was additionally damaged with every subsequent operation. Under such circumstances secondary soft tissue infection was more than expected. Microbiological examinations of the surgical wound at different time points revealed presence of various microorganisms including even Meticillin resistant staphylococcus aureus (MRSA) and Candida albicans which were successfully treated according to the antibiogram. The soft tissue infection additionally damaged the soft tissue cover [5,6]. Hence, after the last surgery the transplanted kidney was functioning well but it was completely exposed with a soft tissue defect over it sizing about 20 × 10 cm (Figure 1). Then plastic surgeons were included as part of the managing team.
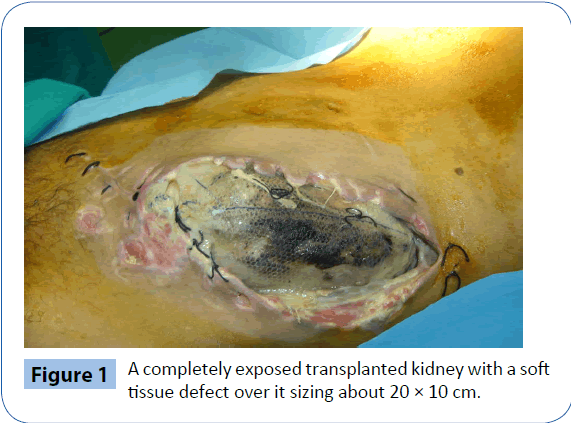
Figure 1: A completely exposed transplanted kidney with a soft tissue defect over it sizing about 20 × 10 cm.
Because of the several operations the local anatomical structures were severely displaced and dense adhesions were present thus making the dissection very difficult and risky. In addition, the patient was previously treated with corticosteroids, he had a long history of CKD with a couple of months on dialysis and he was having serious comorbidities (malnutrition, hypertension, immunocompromised condition). Moreover at that time point he was getting depressed because of the long time spent in hospital along with the plenty of procedures he underwent. That was the rationale why it was decided to cover the soft tissue defect throughout the most simple way.
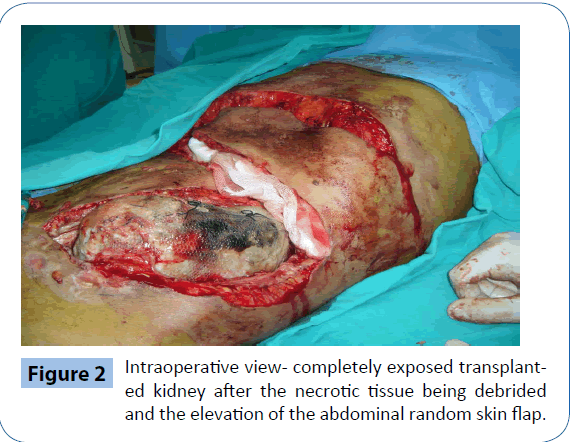
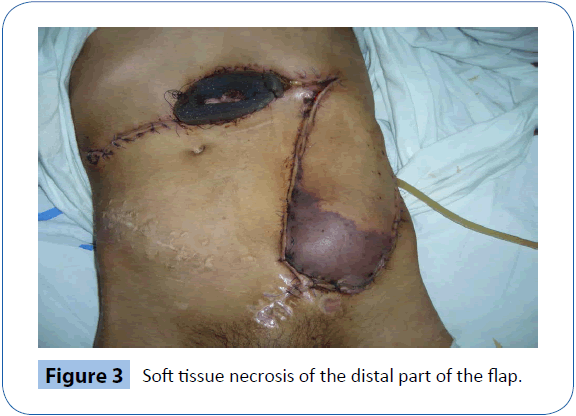
After the necrotic tissue was debrided the overall soft tissue defect became larger (23 × 12 cm). A very long random skin flap from the upper third of the anterior abdomen was used in order to cover the defect (Figure 2). The flap was prepared as a transpositional one. Starting at the first postoperative day there were signs of vascular insufficiency of the distal third of the flap that in the next days progressed to a complete necrosis (Figure 3). This problem was due to both the long flap and the infected recipient bed. At the 5th postoperative day necrectomy was performed when the distal third of the flap was removed. Then the tensor fasciae latae (TFL) fasciomyocutaneous flap was used as a pedicled flap in order to cover the reminder of the defect and as this flap is a thicker and a more vascularised one it was a way to deal with the soft tissue infection [7-9].
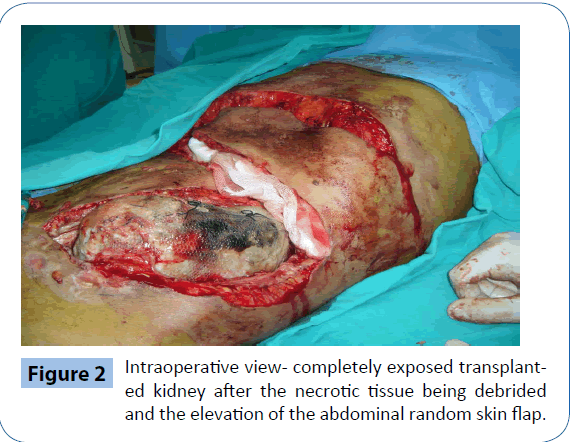
Figure 2: Intraoperative view- completely exposed transplanted kidney after the necrotic tissue being debrided and the elevation of the abdominal random skin flap.
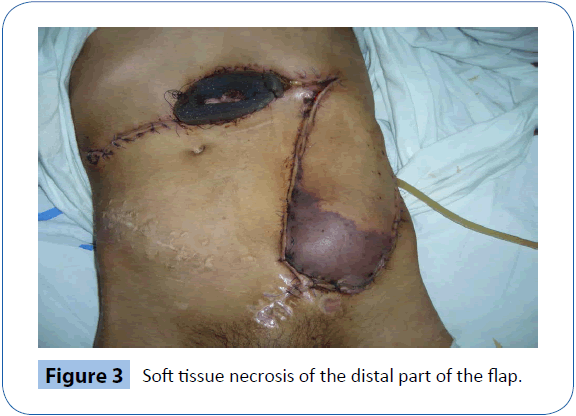
Figure 3: Soft tissue necrosis of the distal part of the flap.
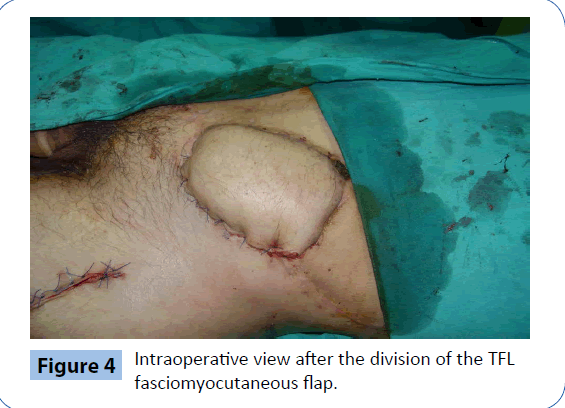
Six weeks after the operation the flap was divided with a satisfying intraoperative result (Figure 4). Yet, two days later signs of vascular insufficiency on the distal part of the flap were noticed. Fortunately, this episode resolved only with partial dehiscence of the flap that healed spontaneously upon repeated dressings.
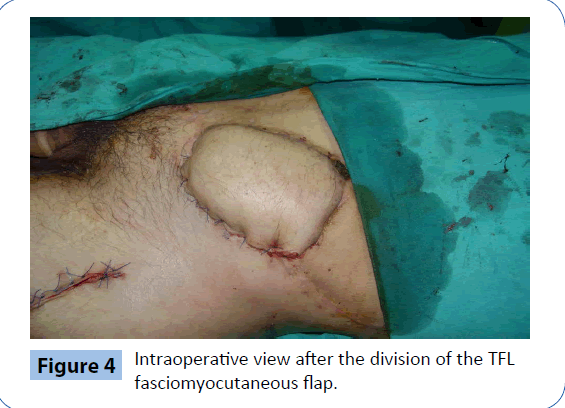
Figure 4: Intraoperative view after the division of the TFL fasciomyocutaneous flap.
The defect was successfully closed combining 2 different local flaps at the same time avoiding the microsurgical anastomosis. As a result the graft was saved and the anterior abdominal wall restored in the manner of function and esthetics. Even now, three years after the transplantation the results remained (Figure 5).

Figure 5: Three years after the transplantation (the flaps setting well over the defect, creatinine levels of 90-100 μmol/l).
Discussion
Kidney transplants have become common surgical procedures that are associated with high success rates. The complication associated with the procedure are low especially compared with other organ transplants. Nevertheless the detection, accurate diagnosis and timely management of surgical complications after kidney transplant are important tasks of the team managing these patients as some of the complications can result in significant morbidity of the recipient, risk of graft loss and mortality [10].
A case that developed a number of different surgical complications including venous thrombosis, wound infection, wound dehiscence and urinary fistula was presented.
Vascular complications despite being rare have devastating consequences particularly arterial and venous thrombosis [10]. Renal vein thrombosis (RVT) is usually seen during the first post transplantation week in 0.3-6.1% of patients. The prognosis of RVT is poor, and hence, its early recognition and treatment is crucial [11].
Approximately two- thirds of the early urologic complications (urine leak or obstruction) occur in the first month after transplantation and are usually successfully treated by the transplantation team. However, the urological complication rates are 4-8% with a very low patient mortality [12].
Surgical site infection have remained as major complication in solid organ transplantation [5,6]. Even worse, in this case there was a surgical site infection along with a completely exteriorized allograft. The allograft was prone to mechanical injury and to infection both of which could have almost inevitably lead to its loss. Covering the wound with well vascularised tissue can facilitated wound healing, struggle against the soft tissue infection and preserve the graft in general [8]. The reconstructive options for extensive lower trunk defects include both free flaps and pediculed flaps each having its own advantages and disadvantages [7]. Using a free flap would have been very difficult because of the very bad local conditions in the presence of soft tissue infection and other patients' comorbidities.
In conclusion, kidney transplant may be associated with various nephrological and surgical complications whose treatment require a multidisciplinary team work. Although at one time point the kidney was supposed to be unsalvageable, the great effort and persistent care invested from all the multidisciplinary team physicians, nurses and with the support from the psychologist and patient's family all complications were successfully overpassed and after a 4 months hospitalization the patient was to discharged with a good graft function.
7938
References
- Kaufman DB (2015) Assessment and management of the renal transplant patient.
- Spasovski G,Dohcev S, Stankov O, Stavridis S, Saidi S, et al. (2013) The improvement in kidney transplant program in R. Macedonia - what are the clues? Prilozi 34: 9-13.
- Spasovski G, MojsovaMiovska M, MasinSpasovska J (2014)The success of South-eastern Europe Health Network (SEEHN) initiative on improvement of the kidney transplant program-facts about Macedonia. TransplInt 27: e63-e64.
- Spasovski G, BusicM, Delmonico F (2015)The improvement in kidney transplantation in the Balkans after Istanbul Declaration - where do we stand today? Clin Kidney J.
- Mehrabi A,Fonouni H, Wente M, Sadeghi M, Eisenbach C, et al. (2006) Wound complications following kidney and liver transplantation. Clin Transplant 20 Suppl 17: 97-110.
- Santangelo M, Clemente M, Spiezia S, Grassia S, Di Capua F, et al. (2009) Wound complications after kidney transplantation in nondiabetic patients. Transplant Proc 41: 1221-1223.
- Rifaat MA, Abdel GawadWS (2005) The use of tensor fascia latapedicled flap in reconstructing full thickness abdominal wall defects and groin defects following tumor ablation. J Egypt Natl Canc Inst 17: 139-148.
- Faizal A, BujangSafawi E, Sundram M, Kueh NS, Normala B (2011) Soft tissue cover for an exposed transplanted kidney with a pedicledmyocutaneous anterolateral thigh perforator and vastuslateralis flap. Urol Int 87: 117-119.
- Saito A,Minakawa H, Saito N, Isu K, Hiraga H, et al. (2014) Clinical experience using a tensor fascia lata flap in oncology patients. Surg Today 44: 1438-1442.
- Parada B, Figueiredo A, Mota A, Furtado A (2003) Surgical complications in 1000 renal transplants. Transplant Proc 35:1085-1086.
- Sezer TO, Hoscoskun C (2015) Vascular complications after renal transplantation.
- Akbar SA, JafriSZH, Amendola MA, Madrazo BL, Salem R (2015) Complications of renal transplantation.