Lim Mei Sin*
Department of Neurosurgery, Queen Elizabeth Hospital, Sabah, Malaysia
*Corresponding Author:
Lim Mei Sin
Department of Neurosurgery, Queen Elizabeth Hospital, Sabah, Malaysia.
Tel: +60162330656
E-mail: meisin85_@hotmail.com
Received Date: July 01, 2017; Accepted Date: July 27, 2017; Published Date: August 04, 2017
Citation: Sin LM (2017) A Variant of Lemierre’s Syndrome – A Case Report. J Neurol Neurosci. Vol. 8 No. 4:211 DOI: 10.21767/2171-6625.1000211
Keywords
Tonsillopharyngitis; Intracranial abscess; Internal jugular vein thrombosis; Lemierre's syndrome
Introduction
A 19-year-old woman presented to the emergency department with a history of high grade fever and pain over the left side of her neck for the past 1 week. She also had intermittent foulsmelling pus discharges from the left ear for 2 months. She was admitted to the ENT department with a diagnosis of chronic suppurative otitis media and was treated with intravenous antibiotics. Subsequently, she complained of acute headache and vomiting episodes. A CT scan of the brain was done showed left otomastoiditis with thin subdural and interhemispheric empyema. CT scan of the neck also shows complete thrombosis of the left jugular vein. The patient underwent mastoidectomy and post operatively, the patient's progress showed a significant improvement. She was also treated with IV Heparin for the IJV thrombosis. She was subsequently discharged home well with oral antibiotics for a total of 6 weeks duration and oral Warfarin.
Case Report
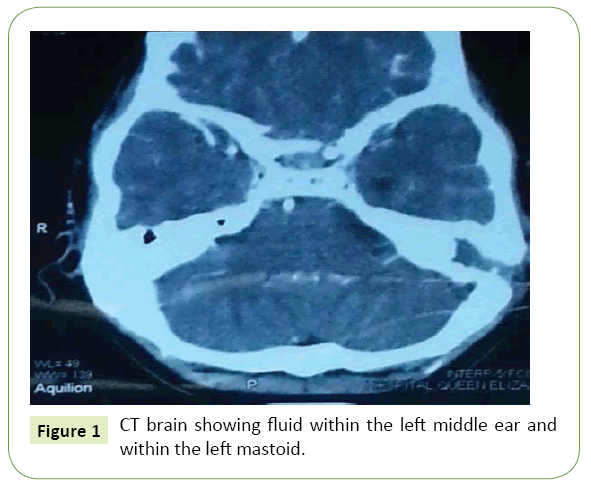
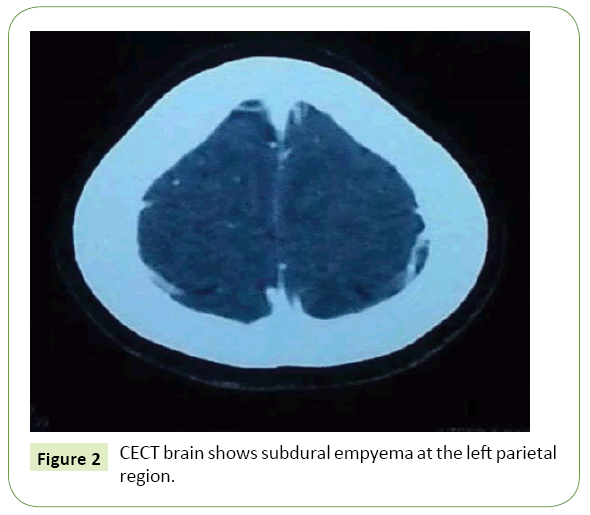
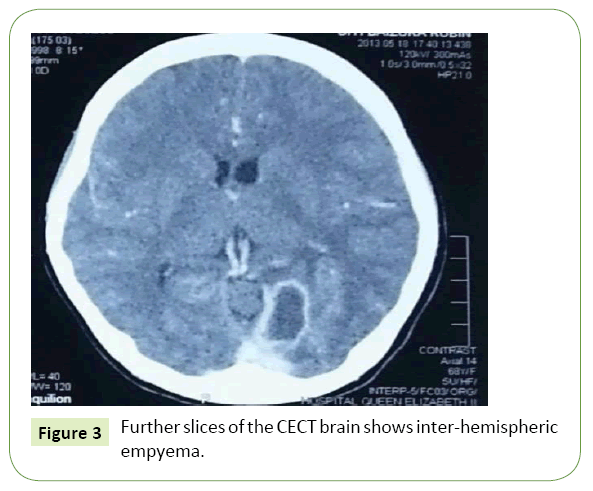
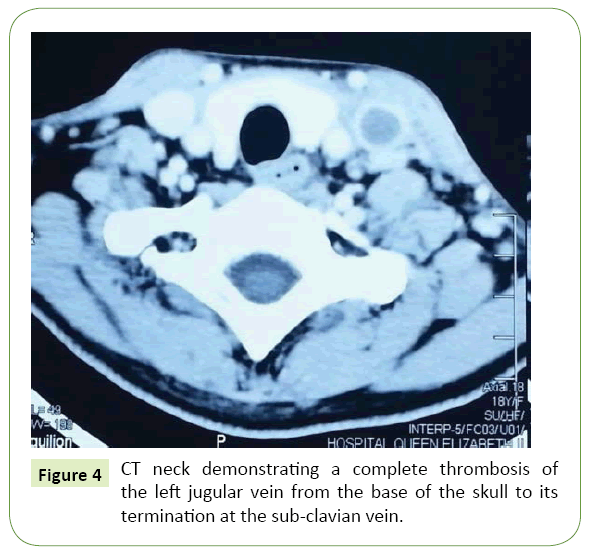
A 19-year-old woman presented to the emergency department with a history of high grade fever and pain over the left side of her neck for the past 1 week. She also had intermittent foul-smelling pus discharges from the left ear that had lasted for 2 months which she did not seek medical attention. Prior to her presentation, she had a history of uncomplicated tooth extraction at a government hospital. Otherwise, her past medical history was unremarkable. On admission, physical examination revealed high grade fever (38.5 degrees) with a diffuse, painful swelling on the left side of her neck near the jugular vein. The oropharyngeal examination was normal. The otoscopic examination demonstrated central perforation of the tympanic membrane in the left ear but no obvious pus discharges. Respiratory examination was however unremarkable. No cardiac murmurs. Neurological examination was also completely normal. Clinically, there was no organ dysfunction. There is no significant family history of malignancies, diabetes or chronic hypertension. Laboratory investigations revealed a white blood cell count of 20,000 with 83% neutrophils and 6% lymphocytes, raised ESR of 99 mm/hour. Otherwise, the blood urea and serum electrolytes as well as coagulation profile were normal. The patient did not have any evidence of sepsis during her course of hospital admission. CT scan of the brain was done which showed fluid within the left middle ear and within the left mastoid in keeping with the diagnosis of a left otomastoiditis (Figure 1) and intracranial extension causing subdural empyema and interhemispheric empyema (Figures 2 and 3). Other significant findings in the CT scan of the neck include a complete thrombosis of the left jugular vein from the base of the skull to its termination at the subclavian vein (Figure 4). The patient underwent mastoidectomy and post operatively, the patient’s progress showed a significant improvement. She was also treated with IV Heparin for the IJV thrombosis. She was subsequently discharged home well with oral antibiotics of cefuroxime for a total of 6 weeks duration as well as oral Warfarin. The patient was followed up in our outpatient clinic whereby a repeated CT brain after 2 weeks of treatment showed near complete resolution of the intracranial empyema and a Doppler Ultrasound also didn’t reveal any propagation of the IJV thrombosis.
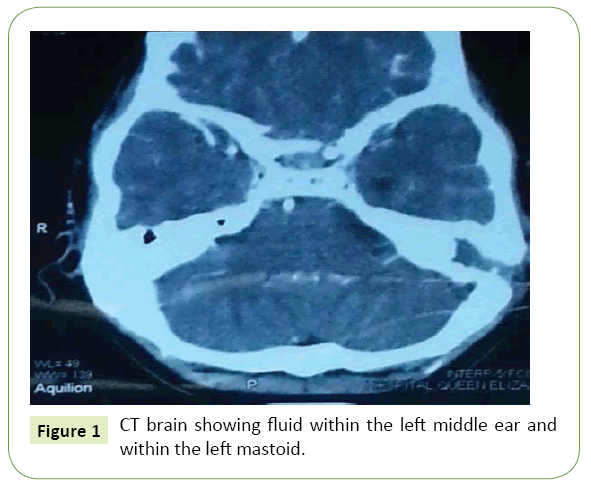
Figure 1: CT brain showing fluid within the left middle ear and within the left mastoid.
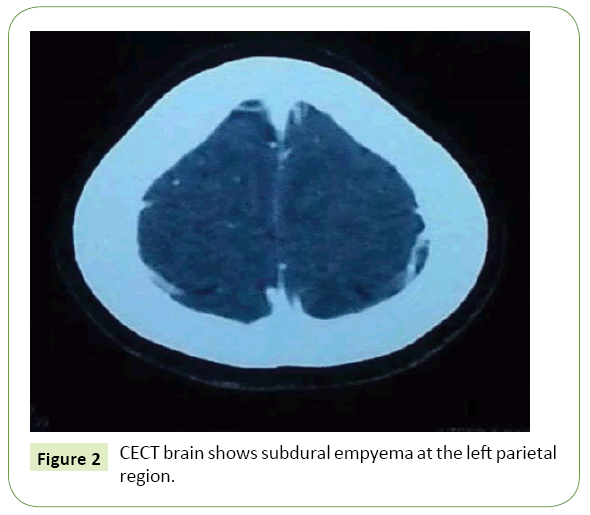
Figure 2: CECT brain shows subdural empyema at the left parietal region.
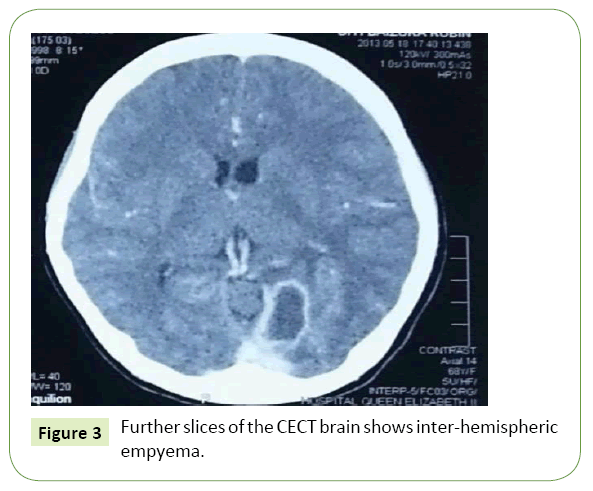
Figure 3: Further slices of the CECT brain shows inter-hemispheric empyema.
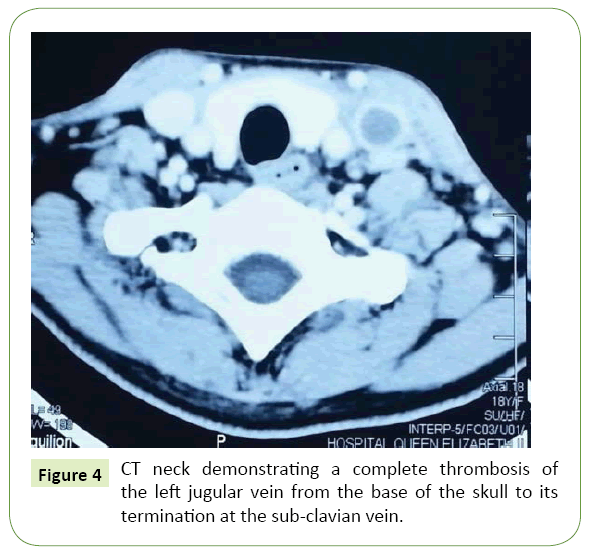
Figure 4: CT neck demonstrating a complete thrombosis of the left jugular vein from the base of the skull to its termination at the sub-clavian vein.
Discussion
Lemierre’s syndrome is a rare but indefinitely severe illness caused by the anaerobic bacterium, Fusobacterium necrophorum [1]. Lemierre’s syndrome remains as a rare disease upon which a prospective study done between 1998 and 2001 in Denmark detected an annual incidence of 1.5 and 0.8 per million persons. In fact, the prevalence of this disease has been reported to be of only 0.6-2.3 per 1,000,000 populations and a mortality rate between 4% to 18% in the world [2].
It typically occurs in healthy teenagers and young adults who usually start as a throat infection which spreads via a septic thrombophlebitis of the tonsillar vein and internal jugular vein. Furthermore, the spread of infection is complicated by septic emboli to other sites such as lung, joints, and bones. Most commonly, it is an infection that manifests as a pharyngotonsillitis or peritonsillar abscess and subsequently seen as a swelling and tenderness in the cervical region due to septic thrombophlebitis of the internal jugular vein (IJV). However, it is important to note that there are cases of this syndrome which is described in association with otitis or otomastoiditis as well which is portrayed in this patient. No doubt that, acute otomastoiditis frequently results in complications such as lateral sinus thrombosis or sagittal sinus thrombosis due to a spread through the bone and dura into the Dural venous sinuses, but in this case, there’s IJV thrombosis which is rather unusual. This pattern of retrograde infection or propagation of venous thrombosis is more frequently due to Lemierre’s syndrome as described in literatures instead of a mere complication from the acute mastoiditis. Hence, this syndrome is highly considered in my patient. In fact, there are other authors who do not feel that the pathogen must necessarily be isolated at all, which is again clearly seen in this patient. The worst outcome from this septic embolus includes the development of internal jugular vein thrombosis due to the retrograde propagation which involves cranial venous sinuses such as the cavernous and sigmoid sinuses. In this variant of the Lemierre’s syndrome, the patient is a previously fit young adult with a history of otomastoiditis which has further caused an extension of infection intracranially; a cerebral abscess which does not require surgical excision. In most cases, these young adults would present with fever, pharyngitis and subsequent signs of internal jugular venous thrombosis (30% to 40%), dry cough and pleuritic chest pains [3]. Chest radiograph might show multiple nodular lesions and bilateral pleural effusions. Other features of metastatic abscess might also occur-for example, empyema or septic arthritis or skin/soft tissue abscess. However, complications of necrobacillosis such as purulent meningitis or cerebral abscesses as seen in this case are rare but possible [4]. Mostly, CT scan with contrast or magnetic resonance (MR) will play an essential role as an imaging modality in the diagnosis as they can help to assess the thromboses seen in the internal jugular vein. The outcome of internal jugular venous thrombosis is usually due to the retrograde propagation which involves the cranial sinuses such as cavernous and sigmoid sinuses. Antibiotic therapy especially which covers this anaerobic infection proves to be the mainstay of treatment. However, drainage of the peri tonsillar abscess might also be necessary. On the other hand, the commencement of anticoagulation for the internal jugular vein thrombosis remains controversial as it has been said to increase the risk of disseminating the infection. Fortunately, this patient responded well to only antibiotics treatment and resulted in a resolution in the intracranial abscess.
Conclusion
Lemierre’s syndrome is a rare disease but nonetheless with severe clinical implications and hence should be highlighted to the public as well as health care profession regarding the possibility of such differential diagnosis during the approach of patients with such clinical presentation. It is usually seen as an oropharyngeal infection, and rarely manifests as otitis media and subsequently complicated with thrombosis of the internal jugular vein. Most importantly is to recognise that central nervous system complications are rare from this syndrome but a known and reported case in some countries.
20081
References
- Raymund R, Razonable M, Rahman AE (2003) Lemierre syndrome variant: Necrobacillosis associated with inferior vena cava thrombosis and pulmonary abscesses after trauma-induced leg abscess. Mayo ClinProc 78:1153-1156.
- Williams M, Kerber C, Tergin H (2003) Unusual presentation of Lemierre's syndrome due to Fusobacteriumnucleatum. J ClinMicrobiol 41:3445-3448.
- Meis JF, Polder TW, Van De Kar P (1993) Multiple brain abscesses and bacteremia in a child due to Fusobacteriumnecrophorum. Infection 21:174-176.