Rajesh Chaudhary*, Ramesh Bharti and Ankit Shukla
Department of Surgery, Dr. R.P. Govt. Medical College Kangra at Tanda HP, India
*Corresponding Author:
Dr. Rajesh Chaudhary
MS, Senior Resident, Department of Surgery, Dr. RP Govt. Medical College Kangra at Tanda HP, India
E-mail: topgun.chaudhary@gmail.com
Received Date: Feb 24, 2016; Accepted Date: Mar 04, 2016; Published Date: Mar 10, 2016
Citation: Chaudhary R, Bharti R, Shukla A. Abdominal Wall Abscess Harbouring Gall Stones and Adenocarcinoma after Laparoscopic Cholecystectomy: A Rare Case Report. Transl Biomed. 2016, 7:1. DOI: 10.21767/2172-0479.100052
Keywords
Gall bladder perforation; Port site malignancy; Parietal wall abscess; Laparoscopic cholecystectomy
Introduction
Throughout the world cholecystectomy is probably the most commonly performed elective operation. Open cholecystectomy by Langenbuch in 1882 remained the treatment standard for gall stones for more than a century when came the era of laparoscopic cholecystectomy which soon became the gold standard treatment of gall stone disease [1]. It is better cosmetically, causes less pain, makes the patient mobile early as compared to the open approach but the rate of complications is high. Bile duct injuries, gall bladder perforation, gall stone spillage, are the most frequent complications [2]. Gall bladder perforation can occur while dissection or while it’s removal from the umbilical or the epigastric ports [3].
Case Report
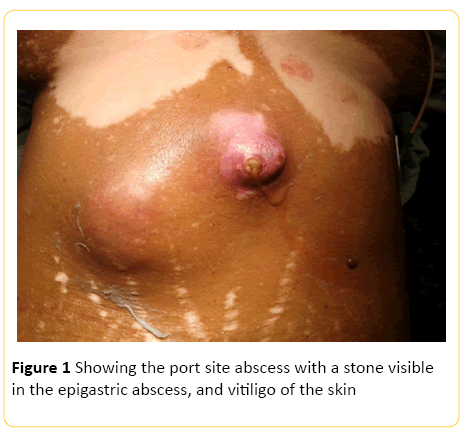
We report a 65 year old female who presented to the emergency room with two parietal wall abscesses. The patient suffered from vitiligo. The patient had undergone laparoscopic cholecystectomy two years back. At the time of admission no medical records were available with the patient. The patient was worked up for surgery and incision and drainage of the abscesses was done under general anaesthesia. The epigastric port site abscess contained about 180 ml of pus and necrotic material (Figure 1). Within that necrotic material there were two multifaceted stones. Another abscess about 10 cm apart and lateral to the epigastric port site in mid clavicular line was drained and necrotic material obtained was sent for histopathological examination. The histopathology report showed adenocarcinoma. Subsequently CT-Scan of the abdomen was done which showed no evidence of intraabdominal malignancy. The patient was planned for wide local excision of the port sites but the patient refused for further treatment.
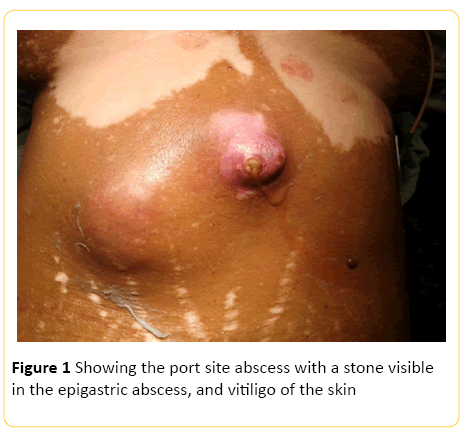
Figure 1: Showing the port site abscess with a stone visible in the epigastric abscess, and vitiligo of the skin
Discussion
Over the past three decades the laparoscopic surgery has become the treatment of choice for the symptomatic gall stone disease. The incidence of complications has been on a decline as the surgeons have become more experienced but still it is more as compared to the open cholecystectomy [3]. The well-known complications are common bile duct injuries, perforation of the gall bladder and spillage of stones. The incidence of gall bladder perforation has been reported to be 15-40% in laparoscopic cholecystectomy [4]. The reported abdominal complication rate after spillage of stones is 1.4%. The gall bladder perforation can occur due to traction applied to visualize the cystic duct and artery, while dissection from the liver bed or while retrieval through the umbilical or the epigastric port. This can result in gall stone spillage which can be avoided by enlarging the extraction incision. If the spillage occurs the perforation should be closed with clips, endoloops or sutures [5]. The chemical composition of the bile and bacteria in the stones can lead to complications. The spilled gall stones can lead to intra abdominal abscess, abscess in the abdominal wall, subphrenic and subhepatic abscesses, dehiscence, hernia, rarely port site tuberculosis and tumors containing stones. Bilirubinate containing stones are known to harbor bacteria and hence are more likely to cause infective complications. They can present within days to years later. The gall stones can lead to fistula formation within the abdomen or externally to the skin. Sometimes they may form subphrenic abscesses and erode into the pleural space [6]. The complications are more commonly seen in old age, male sex, acute cholecystitis, spillage of pigmentary stones. Also the stones larger than 1.5 cm, more than 15 in number and lost in perihepatic location are more known to cause complications [7]. If the spillage of bile and stones occur while doing a laparoscopic surgery, thorough peritoneal toileting should be done with copious amount of saline and every effort should be made to retrieve as many gall stones as possible by using 10 mm suction device. This is more easily done in open cholecystectomy as the packs are applied which prevent their spillage far off but it is not so in case of laparoscopic cholecystectomy. Most of the stones can be retrieved easily and for that matter it is not an indication to convert to an open cholecystectomy, But the gall bladder perforation should be documented properly and note made of any bile leakage or gall stone spillage. Usually a long delay in the operation and the appearance of complications can lead to a wrong diagnosis [8]. A gall bladder harbouring a T1 carcinoma is very difficult to appreciate during laparoscopic cholecystectomy and often a laparoscopic cholecystectomy is curative but a gall bladder perforation can lead to seeding of the peritoneal cavity or the port sites [9]. This is the most devastating drawback of laparoscopic cholecystectomy and is more common in stage 2 carcinoma of gall bladder. The port site positivity means the disease has metastasized and carries a poor prognosis. Thus a laparoscopic cholecystectomy is a contraindication for laparoscopic surgery in suspected carcinoma gall bladder patients [10].
Conclusion
Gall bladder perforartion is one of the most common complications of laparoscopic cholecystectomy. It leads to bile and gall stone spillage. The gall stones can drop into the peritoneal cavity or may be lodged into the parietal wall. This can lead to abscess formation, formation of external or internal fistulas and port site malignancy some times. An abscess harbouring gallstones and malignancy is a rare but serious complication. Hence every attempt should be made to avoid gall bladder perforation and spillage of bile. Emphasis should be on retrieving the stones; and proper documentation of any ball bladder perforation or bile spillage should be done.
Conflict of Interest
The authors declare no conflict of interests.
Consent
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author’s Contributions
Rajesh Chaudhary: Contributed substantially to the Conception and design, Acquisition of data, Analysis and interpretation of data, drafting the article, Critical revision of the article and final approval of the version to be published.
Ramesh Bharti: Contributed substantially to the Conception and design, Acquisition of data, Analysis and interpretation of data, drafting the article, Critical revision of the article and final approval of the version to be published.
Ankit Shukla: Contributed substantially to the Conception and design, Acquisition of data, Analysis and interpretation of data, drafting the article, Critical revision of the article and final approval of the version to be published.
Acknowledgements
Nil
8831
References
- Beal JM (1984) Historical perspective of gallstone disease. Surg Gynecol Obstet 158: 181-189.
- Soper N, Barteau J, Clayman R (1992) Laparoscopic versus standard open cholecystectomy: comparison of early results. Surg Gynecol Obstet 174: 114-118.
- Hawasli A, Schroder D, Rizzo J, Thusay M, Takach TJ, et al. (2002) Remote complications of spilled gallstones during laparoscopic cholecystectomy: causes, prevention, and management. J Laparoendosc Adv Surg Tech A 12: 123-128.
- Kimura T, Goto H, Takeuchi Y (1996) Intraabdominal contamination after gallbladder perforation during laparoscopic cholecystectomy and its complications. Surg Endosc 10: 888-891.
- Kumar TS, Saklani AP, Vinayagam R, Blackett RL (2004) Spilled gall stones during laparoscopic cholecystectomy: a review of the literature. Postgrad Med J 80: 77-79.
- Brockmann JG, Kocher T, Senninger NJ, Schurman GM (2002) Complications due to gallstones lost during laparoscopic cholecystectomy. Surg Endosc 16: 1226-1232.
- Loffeld RJLF (2006) The consequences of lost gallstones during laparoscopic cholecystectomy. The neth. J med 64: 364-366.
- Tsukada K, Kurosaki I, Uchida K (1997) Lymph node spread from carcinoma of the gallbladder. Cancer 80: 661-667.
- Fong Y, Jarnagin W, Blumgart LH (2000) Gallbladder cancer: Comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg 232: 557-569.