N. Boussetta, R. Dhahri*, F. Agili, L. Metoui, Y. Ben Ariba, I. Gharsallah, B. Louzir, N. Ben Abdelhafidh, S. Othmani
Internal Medicine Department, Principle Military Hospital, Tunis, Tunisia
Corresponding Author:
Rim Dhahri
Internal medicine department, Principle Military Hospital
Tunis, Tunisia
Tel: 21671562305
Email: rimdhahri@ymail.com
Keywords
Acute generalized exanthematous pustulosis, Hydroxychloroquine
Background
Acute Generalized Examthematous Pustulosis (AGEP) is an usual cutaneous side effect. It has been reported to occur in antibiotics [1], mainly β-lactams and macrolides.
Clinically AGEP is characterized by a large areas of eythema with sterile pustules, body temperature over 38ºC and neutrophilia (>5,000/mL).
The cessation of the causative drug is usually associated with a spontaneous resotution within 15 days in most of cases [2].
Case report
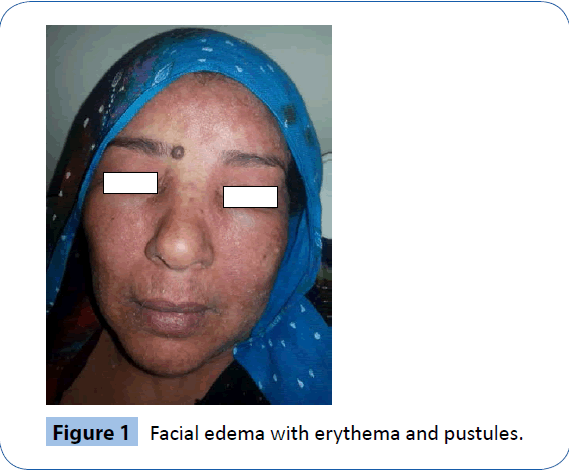
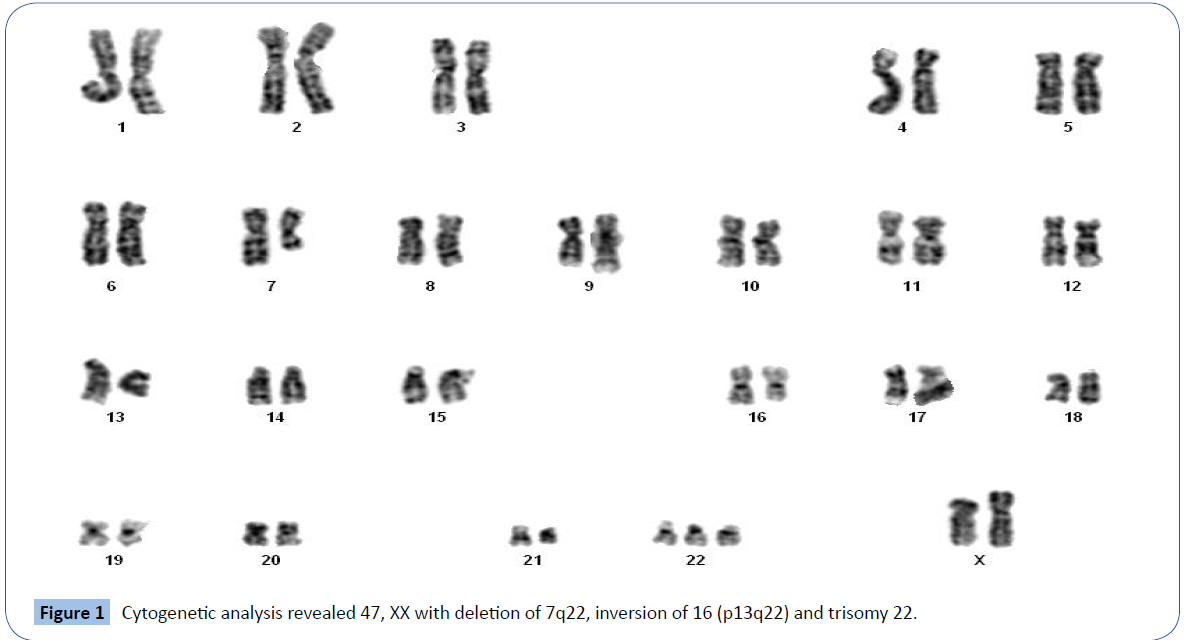
A 54-year-old woman was admitted to our department with an acute widespread pruritic pustular rash and high fever for the last 7 days. She reported that this started 1 month after the beginning of HCQ 200 mg twice daily prescribed for a diagnosis of Sjogren's syndrome associated with pulmonary fibrosis. She reported no psoriasis or eczema in her personal andfamily history. On examination, Her temperature was 40°C. She had facial edema with erythema; multiple pustules on large areas of edematous and erythematous plaques on her lower limbs (Figures 1 and 2). Oral and genital mucosae were normal. Laboratory examination showed white blood cell count at 15,000 elements per mm3 predominantly neutrophils (90%) and CRP at 20 mg / land an erythrocyte sedimentation rate of 120 mm/h. Other biological parameters were normal. Skin biopsy showed necrotic keratinocytes and subcorneal and intradermal pustules associated with edema, and perivascular neutrophil and few eosinophils infiltrate. The histopathological examination did not show no signs of psoriasis or eczeima. The patch test with Hydroxychloroquine practiced in pharmacovigilance department was positive. The EuroSCAR group score was at 4: Severe Adverse Drug Reaction. The diagnosis of HCQ induced AGEP was then retained. HCQ was immediately withdrawn on admission, and supportive treatment including oral antihistamine, local care and paracetamol were administered. On the 7th day of hospitalization, body temperature returned to normal, pustules began to desquamate, erythema and edema subsided, and targetoid lesions partially improved.
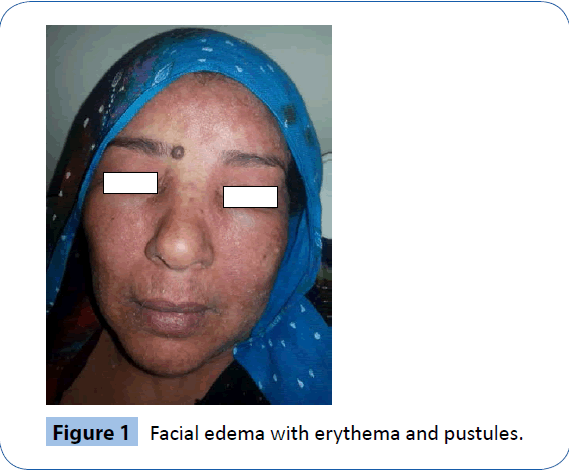
Figure 1: Facial edema with erythema and pustules.
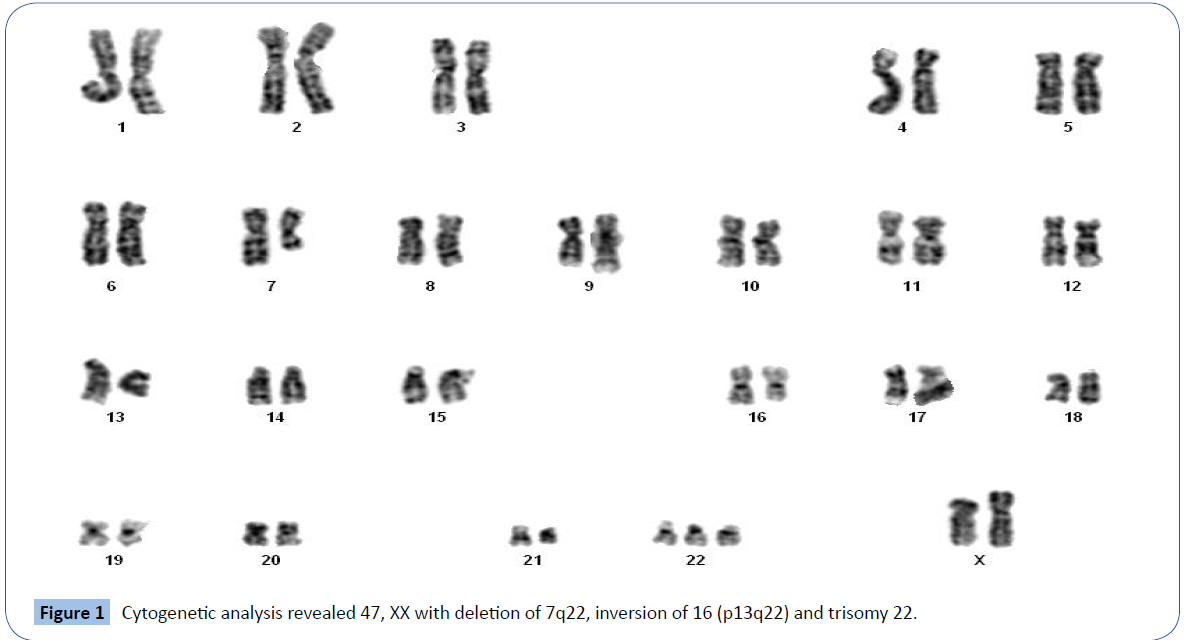
Figure 2: Large areas of edematous and erythematous plaques on the patient's lower limbs with some targetoid lesions.
Discussion
The drug is a drug eruption PAEG in over 90% of cases, with a predominant involvement of antibiotics, including β lactams and macrolides. Hydroxychloroquine is rarely involved [3].
In this case, accountability of HCQ is retained because of the positivity of HCQ test patch and the favorable evolution after treatment cessation. HCQ causes both Pustular Psoriasis (PP) and AGEP. The absence of history of psoriasis and the suggestive histopathologic aspect helped us exclude PP as a differential diagnosis.
The latent period of HCQ-induced AGEP is longer than that of antibiotics-induced AGEP, which are 12∼30 days and 1 day, respectively [4]. The drug' characteristics or the immunologic dysregulation associated with the causative disease may explain this difference.
Conclusion
Our case illustrates a rare side effect of hydroxychloroquine inciting regular monitoring of patients.
7045
References
- Fernando SL (2012) Acute generalised exanthematous pustulosis. Australas J Dermatol 53: 87-92.
- Sidoroff A, Halevy S, BavinckJN, Vaillant L, RoujeauJC (2001) Acute generalized exanthematouspustulosis (AGEP)--a clinical reaction pattern. J CutanPathol 28: 113-119.
- Paradisi A, Bugatti L, Sisto T, Filosa G, Amerio PL, et al. (2008) Acute generalized exanthematouspustulosis induced by hydroxychloroquine: three cases and a review of the literature. ClinTher 30: 930-940.
- Sidoroff A, Dunant A, Viboud C, Halevy S, BavinckJN, et al. (2007) Risk factors for acute generalized exanthematouspustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br J Dermatol 157: 989-996.