Sarita Choudary*
S.M.S Medical College Jaipur, Rajasthan, India
Corresponding Author:
Sarita choudary
S.M.S Medical College Jaipur, Rajasthan, India
Tel: 09413384988
E-mail: drsaritachoudhary@yahoo.com
Received date: December 02, 2015; Accepted date: December 18, 2015; Published date: December 24, 2015
Citation: Choudary S, Acute Myocardial Infarction with Simultaneous Involvement of Right Coronary Artery and Left Anterior Descending Artery: A Case Report. Arch Med. 2015, 8:1.
Keywords
Acute myocardial infarction, Coronary artery disease, Coronary artery thrombosis, Double infarction, Combined myocardial infarction, Multivessel occlusion
Introduction
The pathogenesis of acute myocardial infarction (AMI) is rupture of coronary artery plaque resulting in acute thrombotic occlusion of a coronary artery that is the “culprit” lesion, but on rare occasions this culprit lesion can be found in more than 1 artery. This is rare and has poor prognosis. Here, we report a case of acute myocardial infarction (AMI) with simultaneous total occlusion of the left anterior descending artery (LAD) and right coronary artery (RCA).
Case report
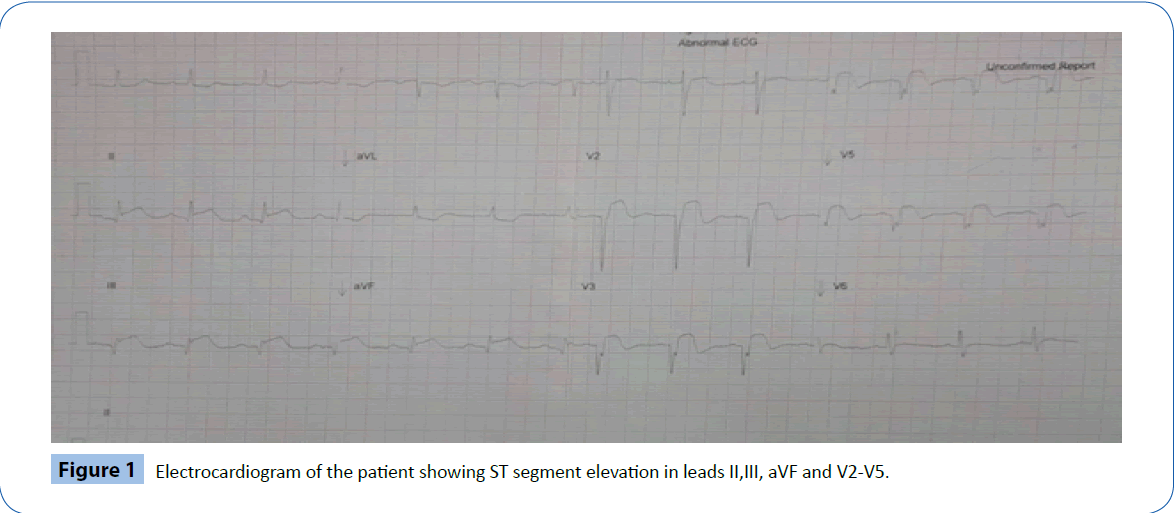
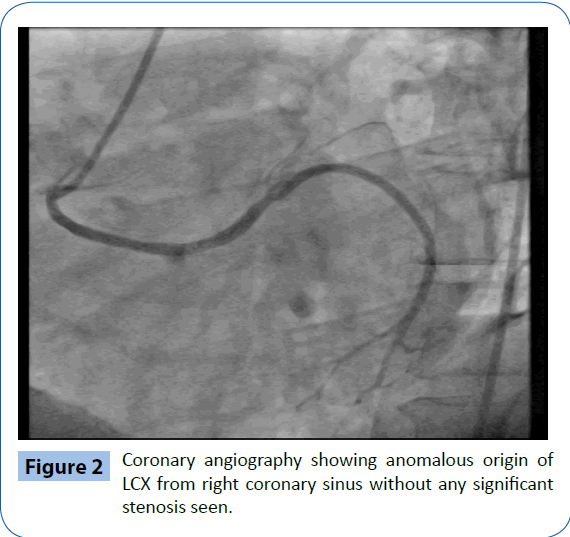
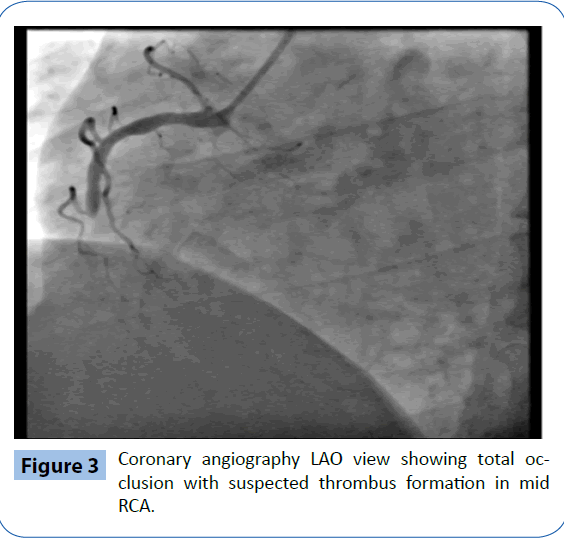
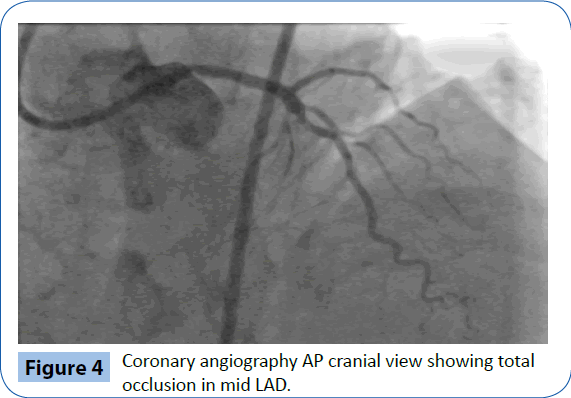
A 56-year-old male presented to the emergency department with sustained chest pain and diaphoresis since past 3 hours. He was chronic smoker since past 15 years. Patient was on antihypertensive drugs since last 2 years .He had no history of diabetes mellitus or family history of coronary artery disease. On presentation his blood pressure was 140/90 mm Hg and physical examination revealed no abnormality. His lung fields were clear. The initial 12 lead electrocardiogram showed a sinus rhythm with ST segment elevation in leads II,III, aVF, and V2-V5 (Figure 1). The echocardiographic examination showed hypokinetic wall motion abnormality of mid distal anteroseptal , apical and basal inferior wall of left ventricle , with left ventricular ejection fraction(LVEF) of 40%. Patient was in killip class 1 and TIMI score was 2/14 (hypertension, anterior lead ST elevation). Patient was started on antiplatelets, statin, heparin and was taken for primary percutaneous coronary intervention (PCI). Coronary angiography showed anomalous origin of LCX from right coronary sinus (Figure 2) and total occlusion with suspected thrombus formation in mid RCA and mid LAD (Figures 3 and 4). Patient underwent successful PCI, with drug eluting stent implantation in both LAD and RCA. Further hospital stay was uneventful and patient was discharged on day four.
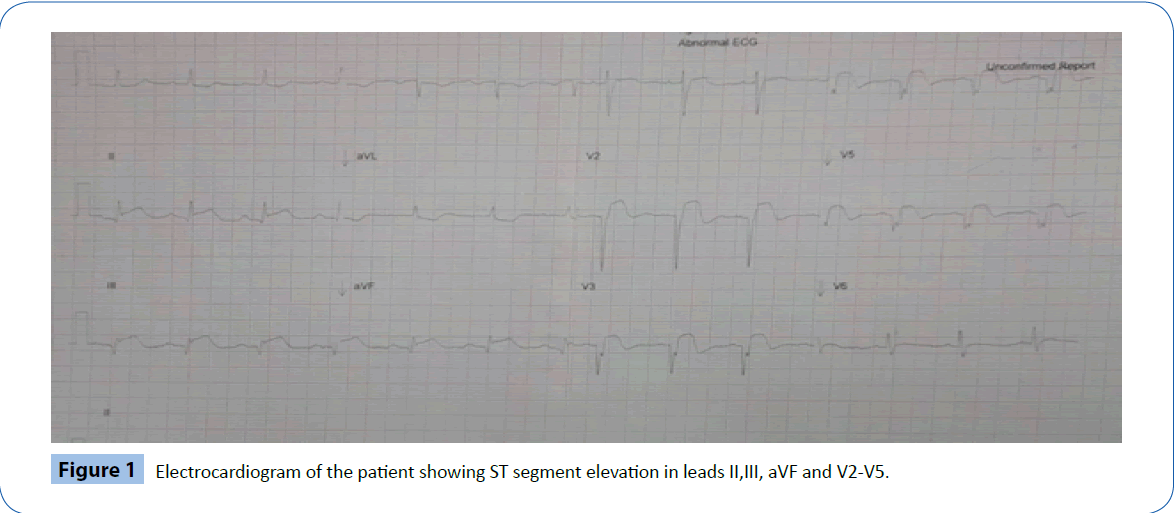
Figure 1: Electrocardiogram of the patient showing ST segment elevation in leads II,III, aVF and V2-V5.
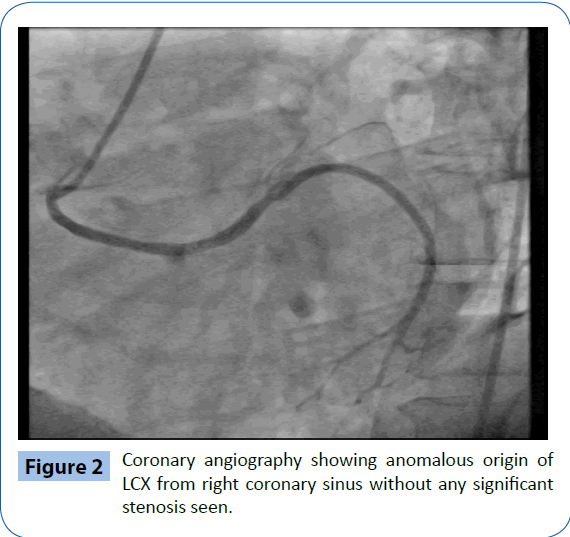
Figure 2: Coronary angiography showing anomalous origin of LCX from right coronary sinus without any significant stenosis seen.
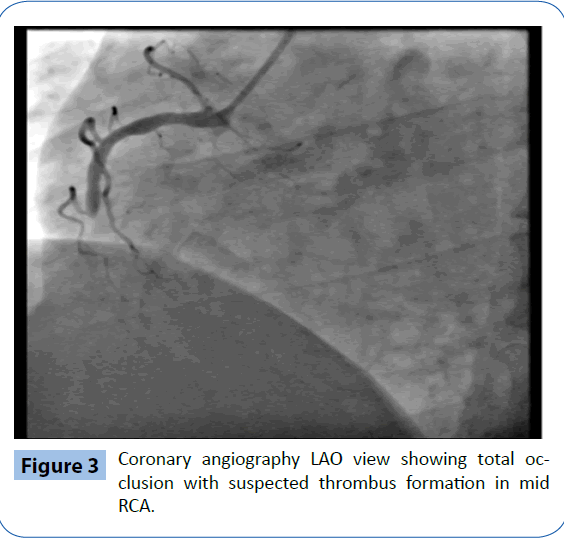
Figure 3: Coronary angiography LAO view showing total occlusion with suspected thrombus formation in mid RCA.
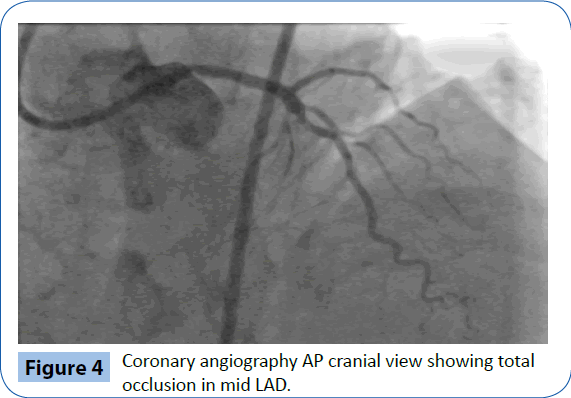
Figure 4: Coronary angiography AP cranial view showing total occlusion in mid LAD.
Discussion
AMI commonly occurs through occlusion of a coronary artery by atheromatous plaque rupture followed by thrombus formation [1]. In the present case, this phenomena occurred simultaneously in two coronary vessels. Incidence of double-vessel coronary thrombosis may account for 1.7% to 4.8% of all primary PCIs [2]. Although rarely reported in most series of patients admitted for AMI, autopsy studies reveal that thrombotic occlusion of more than one major epicardial coronary artery is not uncommon, occurring in up to 50% of patients with infarction [3]. By contrast, Pollak et al. found 18 cases (2.5%) of multiple culprit arteries in a series of 711 patients undergoing primary PCI. This discrepancy is probably due to selection bias in that patients with multiple culprit arteries are more likely to suffer sudden cardiac death, not surviving long enough to undergo angiography [2]. It is often fatal, resulting in sudden cardiac death, and thus accurate diagnosis of multivessel coronary occlusion is rarely achieved in clinical settings. Further, even if these patients are admitted, hospital mortality rate is still high. Most of these patients have evidence of hemodynamic instability, with approximately 1/3 of patients had cardiogenic shock, and nearly 1/4 of patients had life-threatening arrhythmias or required intra-aortic balloon pumps [2].
The mechanism of multiple simultaneous coronary occlusions is not clear. Several factors are thought to be closely correlated with the disease, such as essential thrombocythemia, idiopathic thrombocytopenic purpura, multivessel spasm, hypercoagulability, and cocaine abuse [4]. Moreover, traditional coronary heart disease risk factors such as diabetes mellitus, cigarette use, and hyperlipidemia also contribute to occlusion. A possible mechanism is the pan-coronary process of vulnerable plaque and simultaneous rupture of multiple plaques in different coronary arteries [5]. The concept that plaque instability is not merely a local vascular accident but probably reflects more generalized pathophysiologic processes with the potential to destabilize multiple atherosclerotic plaques throughout the coronary tree. The presence of multiple complex plaques was independently predictive of clinical events [6]. Another possible mechanism is the first ischemic event causing impairment of blood flow to other vessels or increased catecholamine surge and inflammatory response caused by the occlusion of the first artery causing thrombosis of the other [4].
It occurs more commonly in males (85%), smokers and dyslipidemic patients [2]. Angiographically, RCA and LAD acute occlusion (49%) was the commonest presentation (as in our patient), followed by RCA and left circumflex (28%) (1). LAD (78%) and RCA (87%) were the arteries involved in most patient [4].
The 12-lead ECG is an important tool for the diagnosis and localizing the infarct-related coronary artery in AMI. However, its use is limited in patients with simultaneous coronary occlusions. However in our case, the initial ECG revealed ST elevation over leads II, III, aVF, and V2-5 correlated with both anterior and inferior territory involvement. A combination therapy of judicious medical treatment, efficient primary PCI and early mechanical support devices is crucial to improving the survival rate of this high mortality rate disease [7]. Most logical strategy when treating ACS with two culprit arteries is complete revascularization in the acute phase [8,9]. Our patient was treated aggressively with glycoprotein IIb/IIIa inhibitor, dual anti-platelet therapy, thrombus aspiration and stenting in both the RCA and LAD. Because the added complication of cardiogenic shock is common in these high risk patients further mechanical support with IABP or even an extracorporeal membrane oxygenation device may be necessary. Several factors, such as old age, poor left ventricular systolic function may worsen the prognosis.
Conclusion
Acute myocardial infarction caused by simultaneous multi-vessel coronary occlusion is a rarely reported event that needs immediate management owing to the higher mortality rate and complicated hospitalization course with arrhythmia, heart failure, and cardiogenic shock. Therefore early diagnosis, aggressive reperfusion therapy and medical treatment are very important in these cases.
7936
References
- Arbustini E, Dal Bello B, Morbini P, Burke AP, Bocciarelli M, et al. (1999) Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart 82: 269-272.
- Pollak PM, Parikh SV, Kizilgul M, KeeleyEC (2009) Multiple culprit arteries in pa¬tients with ST segment elevation myocardial infarction referred for primary percutaneous coronary intervention. Am J Cardiol 104: 619-623.
- Davies MJ, Thomas A (1984) Thrombosis and acute coronary-artery lesions in sudden cardiac ischemic death. N Engl J Med 310: 1137-1140.
- Kanei Y,Janardhanan R, Fox JT, Gowda RM (2009) Multivessel coronary artery thrombosis. J Invasive Cardiol 21: 66-68.
- Asakura M, Ueda Y, Yamaguchi O, Adachi T, Hirayama A, et al. (2001) Extensive development of vulnerable plaques as a pan-coronary process in patients with myocardial infarction: an angioscopic study. J Am CollCardiol 37: 1284-1288.
- Goldstein JA,Demetriou D, Grines CL, Pica M, Shoukfeh M, et al. (2000) Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med 343: 915-922.
- Sia SK, Huang CN, Ueng KC, Wu YL, Chan KC (2008) Double vessel acute myocardial infarction showing simultaneous total occlusion of left anterior descending artery and right coronary artery. Circ J 72: 1034-1036.
- Derian W, Hertsberg A (2007) Acute myocardial infarction from simultaneous total occlusion of the left circumflex and right coronary artery. A case report. Int J Cardiol 119: e65-67.
- Maagh P, Wickenbrock I, Schrage MO, Trappe H-J, Meissner A (2008) Acute simultaneous proximal occlusion of two major coronary arteries in acute myocardial infarction: successful treatment with percutaneous coronary intervention. J IntervenCardiol 21: 483-492.