Statistics from the triennial 2010-2013, Mater Dei Hospital Activity Analyses suggest that pressure on bed occupancy is at its greatest during the months from December to March. For the “top five” medical causes for hospitalization, admission numbers increase from an average 305 admissions per month to 399 admissions per month during the peak winter period. This time of the year coincides with the annual influenza season.
Influenza vaccination of high risk population groups has been reported to reduce hospitalization by 32% to 45%. The World Health Organization (WHO) and European Union (E.U.) have recommended that, by 2010 and 2014 respectively, 75% of high risk groups should be immunized against influenza every year.
Vaccination of the elderly population in Malta is currently 40%. Only 70,000 individuals are vaccinated in the Maltese Islands giving a overall population vaccination rate of approximately 16%. In addition, this shortfall in vaccination uptake has in the past resulted in a perennial wastage of more than 8,000 vaccinations per year.
In order to address these lacunae, an influenza vaccination initiative was spearheaded by Mater Dei Hospital’s Patient Safety and Quality Improvement Team (PaSQIT), focusing on high risk patients attending the hospital environs for outpatient or other appointments. The vaccination station was sited in a strategic position close to the Outpatients’ Department so as to increase vaccination uptake. The total number of vaccinations given through this initiative exceeded 7,500.
Keywords
Influenza, Vaccination, Hospitalization rate, High Risk Groups
Introduction
It is evident from the Mater Dei Hospital Activity Analyses (HAA) [1] that the greatest strain on the hospital bed-state occurs during the months of December till March coinciding with the ‘Influenza Season’. The strain on bed occupancy reflects itself in the increased number of admissions and in the length of hospital stay.
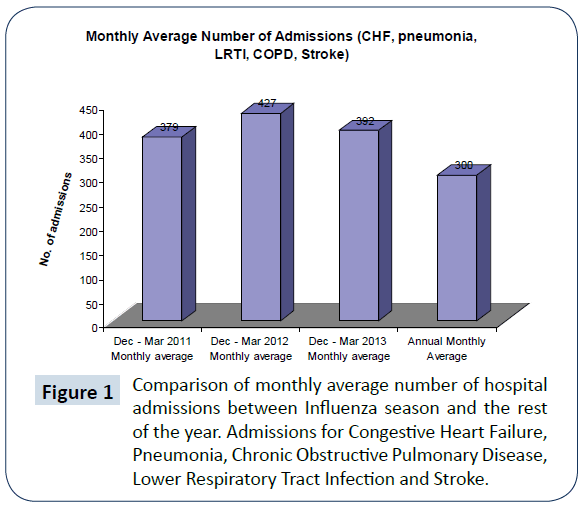
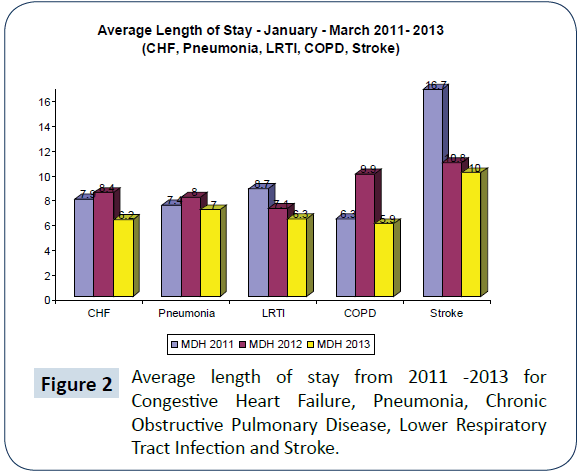
The five most common medical causes for significant hospital stay are Congestive Heart Failure, Pneumonia, Chronic Obstructive Pulmonary Disease, Lower Respiratory tract infection and Stroke (HAA). The average monthly number of admissions for these medical conditions during the years 2011- 2013 was around 305 patients. During the months of December – March, the average number of admissions was 379 (Dec-Mar) 2011, 427 (Dec-Mar 2012), and 392 (Dec-Mar 2013) (HAA) (Figures 1 and 2).
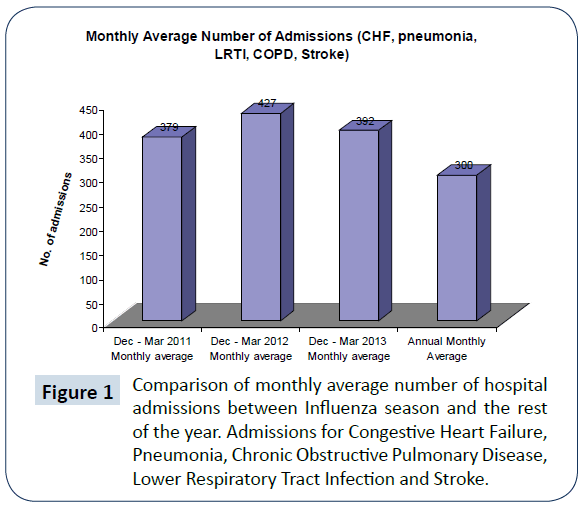
Figure 1: Comparison of monthly average number of hospital admissions between Influenza season and the rest of the year. Admissions for Congestive Heart Failure, Pneumonia, Chronic Obstructive Pulmonary Disease, Lower Respiratory Tract Infection and Stroke.
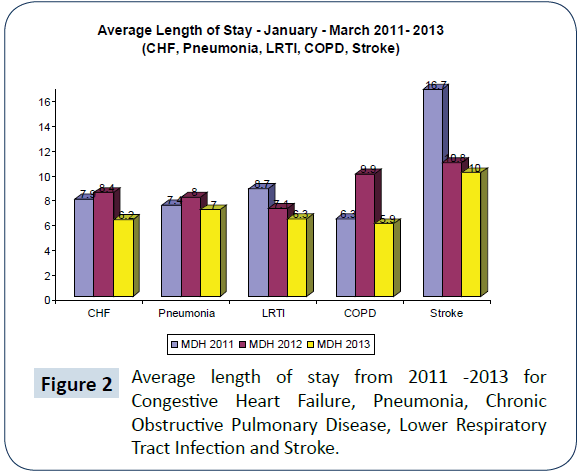
Figure 2: Average length of stay from 2011 -2013 for Congestive Heart Failure, Pneumonia, Chronic Obstructive Pulmonary Disease, Lower Respiratory Tract Infection and Stroke.
Influenza Vaccination and Reduction in Hospitalization
One of the most effective ways to reduce hospitalization during the Influenza season is through immunization with the Influenza vaccine [2-4]. While the influenza vaccinate is considered to be less immunogenic than other traditional vaccinations in part due to immune exhaustion [5], several studies indicate significant reductions in hospitalization are achievable when high risk groups are targeted for vaccination with influenza vaccine [4,6,7] Within high risk groups (Congestive Heart Failure, Pneumonia, Chronic Obstructive Pulmonary Disease, Lower Respiratory Tract Infection and Stroke) reductions in hospitalization ranging from 19% till 57% have been reported (Table 1). Significant reductions in hospitalization in the order of 21% to 63%, have also been noted when vaccination was given to the adults aged 65 years and over. A meta-analysis by Gross et al (1995) suggests that vaccination in the elderly reduces hospitalization in the range of 32% to 45% (Table 2).
| AuthorInfluenza vaccination |
Cohort |
Reduction in Hospitalization |
| Nichol |
Chronic lung disease |
52% |
| Nichol |
Cardiac disease
Stroke
Pneumonia |
19%
23%
32% |
| Wang |
Lung diseases,
Congest heart failure |
43% |
| Nichol |
Pneumonia
Chronic Lung disease
Congestive Heart Failure |
48-57%
27-39%
37% |
| Jefferson |
Respiratory diseases
Pneumonia
Cardiac disease |
22%
27%
24% |
Table 1: Influenza vaccination leading to reductions in hospitalization in patients with chronic disease.
| Author |
Cohort |
Reduction in Hospitalization |
| Mangatani |
65 years or older |
21% |
| Jefferson |
65 years or older |
45% |
| Ahmed |
institutional care and chronic illness |
63% |
| Foster |
noninstitutionalized 65+ years |
45% |
| Gross |
elderlypersons |
32%-45% |
Table 2: Influenza vaccination leading to reductions in hospitalization following vaccination of senior persons.
Bed Occupancy and Influenza vaccination
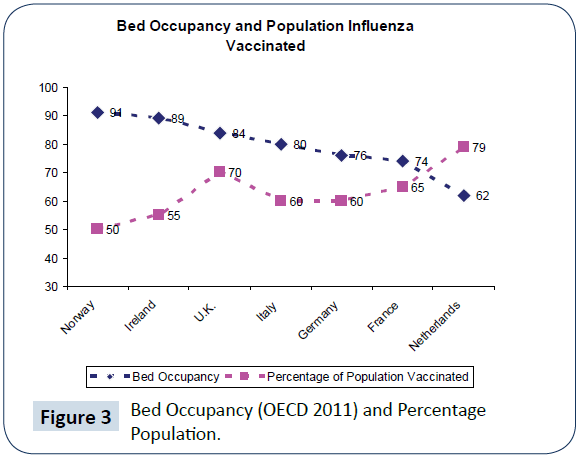
There appears to be a trans-national correlation between bed occupancy (Organisation for Economic Co-operation and Development 2011) [8] and influenza vaccination (Figure 3). In The Netherlands where 79.9% of adults at risk were vaccinated, the bed occupancy was 62% which is the lowest recorded by an OECD report in 2011. Conversely in Norway where the vaccination rate for high risk patients is 50% the bed occupancy is 91% (OECD 2011) [8]. Between these two extremes lies a national trend also supporting a correlation between vaccination rates of high risk group and acute bed occupancy (Table 3). While this correlation appears to be significant, the potential influence of confounders cannot be ignored. Countries with higher community vaccination uptake show concurrently high performance indicators in many other areas relating to quality of care ranging from incidence of healthcare associated infections to patient rights [9].
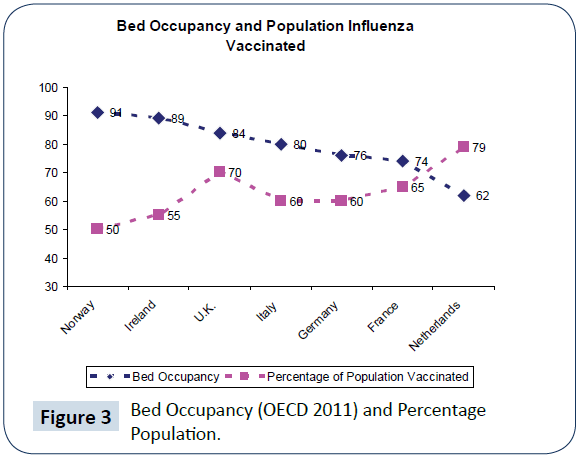
Figure 3: Bed Occupancy (OECD 2011) and Percentage Population.
| “Top 5” reasons for admission to Mater Dei Hospital in 2012 |
No of Episodes |
MDH ALOS |
Total Length of Stay(days) |
| Heart failure |
821 |
7.4 |
6067 |
| Pneumonia |
695 |
8.3 |
5790 |
| Chronic obstructive pulmonary disease |
534 |
7.2 |
3842 |
| Acute lower respiratory infection |
410 |
7.0 |
2868 |
| Stroke |
233 |
11.4 |
2662 |
Table 3: MDH Top 5 reasons for admissions 2012(HAA).
World Health Organization and European Union Influenza Vaccination Recommendations
The World Health Organization (WHO) has recommended that by 2010, 75% of the population at high risk should be vaccinated. The European Union has supported this recommendation and proposed that the 75% threshold should be attained by all member states by the years 2014-2015.
Currently around 70,000 individuals are vaccinated annually in the Maltese Islands giving a population vaccination rate of approximately 16%. From various communications with Maltese Public Health officials it is evident that there is a substantial shortfall in vaccination uptake with a perennial wastage of around 8,000 vaccinations per year. Mereckiene reported that the vaccination rate for elderly population in Malta was 40% [10].
The Introduction of the Hospital Influenza Vaccination Initiative
It is clear that a concerted effort is required to target high risk patients in the Maltese population. To address this, an initiative was undertaken by the Patient Safety and Quality Improvement Team (PaSQIT) of Mater Dei Hospital whereby influenza vaccination was proactively offered to high risk patients attending the hospital. At the same time, more aggressive techniques were adopted by the Infection Control Department of the hospital to increase uptake among healthcare workers [11].
The PaSQIT initiative involved the setting up of a vaccination station at a strategic point in the hospital. The vaccination station was set up one week after the influenza vaccine was available so that patients attending the National Immunization Centre will not be diverted [12]. The duration of the initiative spanned two weeks.
The most strategic place identified was the foyer between the outpatient waiting area and the main hospital corridor. This is a busy thoroughfare where large number of patients passes through. This site has also the added advantage that the Infection Control Department is only one floor under allowing the possibility of secure cold chain storage in this Department [13].
Conclusion
The desired results emanating from this initiative was to optimise the bed occupancy of Mater Dei Hospital by reducing hospitalization during the “Influenza Season”. If the medical literature is congruent with clinical reality and compliance with this initiative is favourable, significant reductions in hospitalization may be registered. In the medical literature the minimum reduction in hospitalization of high risk patients has been quoted as 20%.[11]
Improving bed occupancy may relieve the pressure on the hospital bed-state and consequently may lead to the attainment of the “holy grail” of Medical Ward Specialization in Mater Dei Hospital. The Hospital Influenza Vaccination Initiative may thus significantly improve the hospital bed-state management leading to greater patient safety and quality care.
Sincere gratitude is to go PaSQIT members:
Carmel Abela, Oscar Aquilina, Dustin Balzan, Charles Borg, Michael A. Borg, John Cassar, Miriam Dalmas, Margaret Muscat, Yves Muscat Baron, Corinne Ward
18328
References
- Mangtani P, Cumberland P, Hodgson CR, Roberts JA, Cutts FT, et al. (2004) A cohort study of the effectiveness of influenza vaccine in older people, performed using the United Kingdom general practice research database. J Infect Dis 190: 1-10.
- Gross P, Hermogenes A, Sacks H, Lau J, Levandowski R, et al. (1995) The efficacy of influenza vaccine in elderly persons: a meta-analysis and review of the literature. Ann Intern Med 123: 518-527.
- Jefferson T, Rivetti D, Rivetti A, Rudin M, Di Pietrantonj C, et al. (2005) Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet 366: 1165-1174.
- Foster D, AkkeNeel T, Furumoto-Dawson A, Ohmit S, Margulies J, et al. (1992) Influenza vaccine effectiveness in preventing hospitalization for pneumonia in the elderly. Epidemiol 136: 296–307.
- Lang PO, Mendes A, Socquet J, Assir N, Govind S, et al. (2012) Effectiveness of influenza vaccine in aging and older adults: comprehensive analysis of the evidence. Clin Interv Aging7: 55-64.
- Nichol k, Margolis K, Sterberg T (1994) The efficay and cost effectives of influenza vaccination of the elderly in the community. New England Journal of Medicine 331: 778- 84.
- Health at a Glance (2011) Organisation for economic co-operation and development (OECD).
- Wang CS, Wang ST, Lai CT, Lin LJ, Lee CT, et al. (2004) Reducing major cause-specific hospitalization rates and shortening hospital stays after influenza vaccination. Clin Infect Dis. 39: 1604-1610.
- Mereckiene J Cotter S, D'Ancona F, Giambi C, Nicoll A, Lévy-Bruhl D, et al. (2010) Differences in national influenza vaccination policies across the European Union, Norway and Iceland 2008-2009. Eurosurveillance 15: 44.
- Borg MA (2012) Could the incidence of healthcare infections in Europe simply be a reflection of overall quality standards? J Hosp Infect 82: 141-2.
- Ryan J, Zoellner Y, Gradl B, Palache B, Medema J (2006) Establishing the health and economic impact of influenza vaccination within the European Union 25 countries. Vaccine 24: 6812-6822.
- Nichol K, Baken L, Wuorenma J, Nelson A (2003) The health and economic benefits associated with pneumococcal vaccination of elderly persons with chronic lung disease. Arch Intern Med 159: 2437-2442.