Keywords
Obesity; Airway assessment; Laryngeal Mask Airway (LMA); Complications
Introduction
ESS mandates a secure airway and good control of blood pressure. Tracheal intubation will prevent soiling of the lungs with blood and debris from the surgical sight and prevent aspiration of gastric content from below. A throat pack ensures that no blood passes into the stomach so nausea and vomiting less likely post operatively. The LMA Supreme TM has a unique double seal. A oropharangeal seal which prevent aspiration from above and an oesophageal seal which seperates the digestive tract below. SGAs are an alternative to endotrachael intubation by ensuring adequate ventilation, avoiding hypoxia and preventing aspiration.
Major complications of ESS are intra-cranial orbital injury, blindness, tension pneumo-encephalitis, cerebrospinal fluid leaks, infection and blood loss.
Case Study
A 56-year-old male business executive was scheduled for Septoplasty and ESS. He weighed 113 kilograms with a height of 1.73. He’s body mass index (BMI) was 37.7 kg/m2 and led a sedentary life-style. He used a CPAP mask at night and said his snoring was getting worse. He also complained of daytime somnolence and driving his car was becoming hazardous. There was no history of Diabetes, Hypertension or Ischaemic Heart Disease. He had occasional dyspepsia that settled on antacids.
Physical examination was unremarkable. He had a BP of 143/86. Pulse was 76. Chest examination was clinically normal. He had a short neck a small mouth opening and was classified as a Mallampati 3 (A clinical sign when a small amount of the tonsillar pillar, hard palate, and soft palate are visible with a very slight view of the uvula on inspecting the mouth). A difficult airway was anticipated and prepared for (McCoy laryngoscopes, laryngeal masks) and a surgeon at hand should an urgent surgical airway be required.
Anesthetic technique: The patient was given 100 percent oxygen for three minutes. Metoclopramide 10 mg given at induction. Remifentenil started at 0.05 micrograms/kg/min and midazolam 2.5 mg given as a co-induction agent. Atacurium 2.5 mg administered as a de-facicullating agent and a rapid sequent induction intubation planned. Propofol used as induction agent and with loss of eye-lid reflexes suxamethonium 125 mg given. Cricoid pressure was applied. Laryngoscopy proved difficult and the larynx could not be visualized. Face mask ventilation with a Guedell airway was attempted but ineffective and the patient desaturated preciptously to less than 90 percent. No repeat attempt at laryngoscopy was attempted. A laryngeal mask airway SupremeTM size 5 was then inserted. This was placed with ease and good chest movements observed. Ventilation was shown to be adequate and a good end tidal CO2 graph seen on capnopgraphy. The O2 Saturation which had dropped precipitously was restored to 100 percent.
Surgery was allowed to continue as the airway was protected from above by the First SealTM and below by the Second SealTM which has a gastric drain outlet. Further, muscle relaxation given with 0.5 mg/kg atacurium. Pressure support ventilation (PSV) (Allows control of peak airway pressure during ventilation with less likelihood of barotrauma and respiratory complications. Ventilation strategies in in the obese patient undergoing surgery; Aldenkortt et al.) instituted with PSV of 20 cm H2O and Rate of 13. Good tidal volumes and a minute ventilation of 9.5 with an end-tidal CO2 of 35 achieved. Oxygen saturation remained in the mid-ninety's. The patient was placed in a head- up position (reverse trendelenberg) which further improved ventilation due to less splinting of the diaphram from the abdominal viscera and adipose tissue.
Anaesthesia was maintained on oxygen/nitrous oxide 50% and desflurane at 1 MAC (minimum alveleolar concentration) using low flows of 2 liters/minute. Remifentanil titrated to maintain hemodynamics stability and mean (BP) blood pressure of 80 mm. Hg. Surgery lasted 65 minutes. Perfalgan 1 gm and fentenal 150 micrograms given as analgesia at the end of the procedure as well as decasone 0.1 mg/kg. Muscle relaxation reversed with neostigmine/robinal. Anaesthesia was otherwise uneventful. The patient had bilateral nasal packs inserted, extubated in theatre (OR) and encouraged to breathe through the mouth. He remained co- operative and was placed in a semi-upright position and transferred to the ward on a 40 percent oxygen mask. Seen later that night he remained comfortable except for a small area of surgical emphysema around one orbit. Vision was unimpaired and good ocular movements observed. Ice packs were applied to the affected area and he remained stable overnight and discharged the following morning.
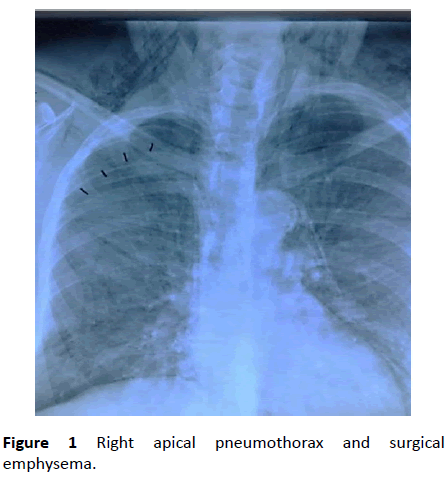
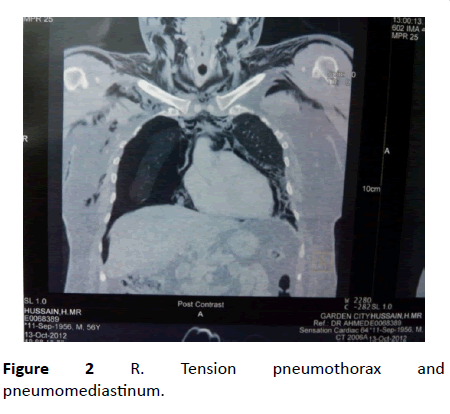
24 hours later the patient was re-admitted in respiratory distress. His breathing was laboured and he had surgical emphysema on the anterior chest wall and neck. A chest radiograph (CXR) also showed a pneumo- mediastinum and a pneumo-thorax on one side (Figures 1 and 2). Repeat laboratory tests included a FBC, Electrolytes and an ECG was normal. Blood gas showed a normal PH and a PO2 of 80 mmHg on a 40 percent face mask. An urgent CT scan of the thorax was requested and swelling of the trachea and narrowing of the tracheal lumen seen. There were also micro tears of the trachea reported which may have caused air tracking into the mediastinum and the surgical emphysema. The uni-lateral R sided pneumo-thorax was now causing compression of the lung and a tension pneumo-thorax had developed. A gastrogaffin swallow excluded any leak or tears of the oesophagus. The patient was scheduled for an elective tracheotomy and insertion of an inter-costal drain (ICD).
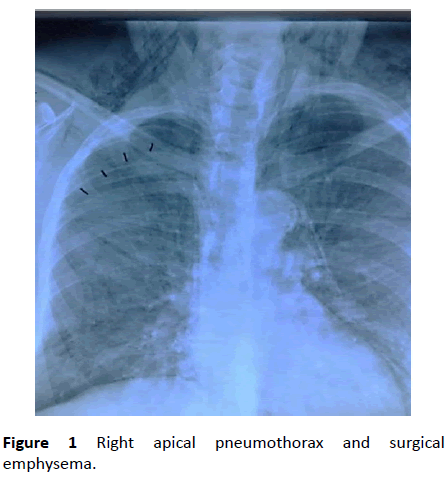
Figure 1: Right apical pneumothorax and surgical emphysema.
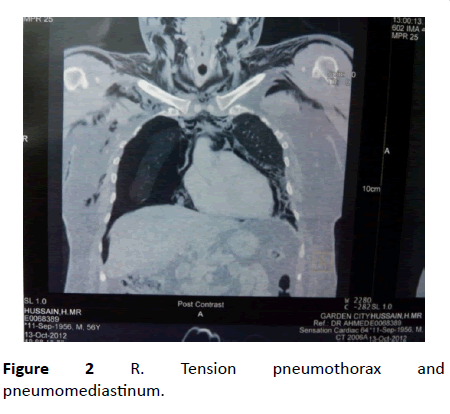
Figure 2: R. Tension pneumothorax and pneumomediastinum.
24 hours later the patient was re-admitted in respiratory distress. His breathing was laboured and he had surgical emphysema on the anterior chest wall and neck. A chest radiograph (CXR) also showed a pneumo- mediastinum and a pneumo-thorax on one side (Figures 1 and 2). Repeat laboratory tests included a FBC, Electrolytes and an ECG was normal. Blood gas showed a normal PH and a PO2 of 80 mmHg on a 40 percent face mask. An urgent CT scan of the thorax was requested and swelling of the trachea and narrowing of the tracheal lumen seen. There were also micro tears of the trachea reported which may have caused air tracking into the mediastinum and the surgical emphysema. The uni-lateral R sided pneumo-thorax was now causing compression of the lung and a tension pneumo-thorax had developed. A gastrogaffin swallow excluded any leak or tears of the oesophagus. The patient was scheduled for an elective tracheotomy and insertion of an inter-costal drain (ICD).
Induction began with a face mask in place and the patient allowed breathing spontaneously on three percent (3%) sevoflurane and 100 percent O2. Midazolam and alfentenyl were titrated to effect and a percutaneous tracheostomy done under local anaesthesia. A right sided ICD was inserted. In the intensive care unit (ICU) a continuous infusion of precedex for sedation and perfalgan and tramadol prescribed for analgesia. Syncronous intermittend mandatory ventillation (SIMV) was used in ICU in view of his high BMI to reduce the work of breathing. Enteral feeding commenced after 12 hours and the patient made good progress with the ICD removed when the lungs had fully expanded. He was left with a fenestrated tracheostomy tube in-situ which allows for speech. Physiotherapy was prescribed to expand areas of lung atelectasis and he was discharged a week later with the tracheostomy tube in-situ and encouraged to start an active weight loss program. A few weeks later the tracheostomy tube removed with no further problems.
Discussion
Major complications following ESS do occur. This unusual complication was the result of micro-tears of the larynx causing tracking of gas and the subsequent surgical emphysema. The lung complications are ventilator-associated lung injuries (VALI) that occurred during the perioperative period caused by Volutrauma (alveolar overdistension), Barotrauma (air leaks) and Biotrauma (inflammatory mediators) during positive pressure ventilation
The difficult airway in the obese patient
An endotrachael tube (ETT) with the use of muscle relaxation is a good first choice in anaesthesia.
It remains the gold standard allowing good ventilation and protection against aspiration. SGAs are useful rescue devices in the event of a difficult or failed intubation and are also being used electively in laparoscopic gynaecological surgery and cholecystectomy [1,2].
The 6 - Ds helpful useful in evaluating difficult airways are [3]
• Disproportion (Mallampati classification.)
• Distortion (e.g. Thyroid masses)
• Decreased thyromental distance (receding chin)
• Dysmobility (decreased range of movement at the cervical spine.)
• Decreased interincisor gap (small mouth opening)
• Dental overbite
Pre-positioning of the obese patient in the Head Elevated Laryngoscopy Position (HELP) improves the view at laryngoscopy and there is an increase in the desaturation safety period [3].
Problems at tracheal intubation can cause serious soft tissue injury, hypoxia and death. In an anticipated or unexpected difficult airway management protocols are lifesaving. In the worst case scenario like cannot incubate cannot ventilate situation a surgical airway is needed. Hodgson R et al. [4] discuss the resources needed to establish a definite airway.
The glidescope videolaryngoscope is a major advance in airway management.
Obese patient and the morbidly obese may be more difficult to intubate. Kim W, Ahn C, Lee C et al. [5] in their study of obese Asian patients (BMI ≥ 27.5 kg /m2 ) note that difficult intubations were more common in obese patients and that a neck circumference to thyromental distance(NC/TM) ratio greater than [5] performed better in predicting difficult intubations then other established indices. Brodsky [6] studied morbidly obese patients with BMI >40 kg/m2 and state that obesity alone is not predictive of tracheal intubation difficulties but a high Mallampati score (≥ 3) and a large neck circumference may increase the potential for difficult laryngoscopy and intubation. A high BMI is a weak but statistically significant predictor for difficult and failed intubation [7].
Sleep apnea (SA) may be associated with upper airway obstruction and obesity. Surgical relief of the obstruction and weight reduction are effective in reversing this condition. Drugs in the perioperative period with respiratory depressant effect must be used with caution or avoided.
There are other major respiratory and cardiovascular complications of obesity. The work of breathing is increased; ventilation/perfusion (V/Q) abnormalities may result in progressive hypoxeamia and pulmonary hypertension. Insulin resistance, hypertension, dyslipidemia and joint diseases are all associated comorbidities.
Airway management with the LMA.
Belena, Nunez, Gracia et al. [1,2] evaluated the safety and efficacy of the LMA Supreme TM during laparoscopic surgery. Oropharangeal leak pressure (OLP) which indicates the degree of airway protection and the feasibility for positive pressure ventilation (PPV) was a mean of 28.2 cm H2O. A mean peak pressure below this during PPV would support its use.
Belena et al. also included obese patients with a BMI greater than 35 kg/m2 in whom the LMA SupremeTM was safe and effective ventilation achieved. He concludes that it provides a functional airway seal with minimum adverse events. They are easy to insert with a high success rate. Coughing and movement may occur. Severe airway complications such as bronchospasm, hypoxia or aspiration were not seen [1].
Post intubation outcome included sore throat, dysphonia and blood on the mask [1]. In a comprehensive study Verghese has reviewed critical incidence and outcome of LMA usage [8]. In 11 900 patients a total of 44 critical incidents were noted. 18 were related to the airway and none required intensive care management. LMAs were considered safe and effective for both spontaneous and controlled ventilation.
LMAs may be recommended as essential devices in cannot intubate cannot ventilate situation.
Conclusion
All obese patients for anaesthesia will require proper preparation and assessment as airway management remains challenging. Obesity remains a global epidemic and its prevalence high in both sexes. It is a chronic lifestyle disease that impact on health [9]. The perioperative period requires skills and vigilance, and should complications occur timely interventions are lives saving.
21612
References
- Belena JM, Nunez M, Gracia JL, Perez JL (2012) the laryngeal mask airway supreme(TM): safety and efficacy during gynaecological laparoscopic surgery. South Afr J Anaesth Analg 18: 143-146.
- Belena JM, Gracia JL, Ayala TL, Nunez J (2011) The laryngeal mask airway supreme for positive pressure ventilation during laparoscopic cholecystectomy. J Clin Anesth 23: 456-460.
- Troop C (2017) Difficult Intubation in the obese patient. J Anesthesia Surgery. 2: 1-4.
- Hodgson RE, Milner A, Barrett D, Alberts A, Joubert I, et al. (2008) Airway management resources in operating theaters. South Afr J Anaesth Analg 14: 1-15.
- Kim WH, Ahn H J, Lee CJ, Shin BS, Ko JS, et al. (2011) Neck circumference to thyromental distance ratio: A new predictor of difficult intubation in obese patients. Br J Anaesth 106: 743-748.
- Brodsky JB, Harry JM, Lemmens M, Brock-Utne JG, Vierra M, et al. (2002) Morbid obesity and trachael intubation. Anesth Analg 94: 3732.
- Lundstrom LH, Moller AM, Rosenstock C, Astrup G, Wetterslev J (2009) High body index is a weak predictor for difficult and failed tracheal intubation Anaesthesiolo 110: 266.
- Verghese C, Brimacombe JR (1966) Safety and efficacy. Survey of laryngeal mask usage in 11,910 patients: Safety and efficacy for conventional and nonconventional usage. Anesth Analg 82: 129-133.
- Goedecke JH, Jenning LL, Lambert EV (2006) Obesity in South Africa. In: Steyn K, Fourie J, Templen N (eds) Chronic diseases of lifestyle in South Africa: 1995–2005. (Chapter 7). Technical Report. Cape Town: South African Medical Research Council: 65–79.