Abstract
Greeting and significance: Men commonly develop spontaneous tumours called testicular neoplasms. Neoplasms associated with sex cord stromal tumours are also the rarest subset of them. The most prevalent type of testicular stromal tumours is Leydig cell tumours. In our situation, cryptorchidism was the underlying risk factor linked to the growth of Leydig cell tumours. Although usually unilateral, occurrences of bilateral cryptorchidism may exist and have very occasionally been documented. Presentation of a case we are reporting on a 36-year-old male who has been unable to have sex for the previous two years without having trouble getting an erection when stimulated. He had left orchidopexy 20 years prior due to a history of left undescended testis from birth. An ultra-sonogram a heterogeneous oval hypoechoic mass in the right midinguinal canal on the pelvis. Relevant blood tests revealed an abnormal hormonal profile. After that, he underwent a right radical orchiectomy without incident; the histology revealed a Leydig cell tumour. Clinical conversation: Rarely have reports been made of bilateral cryptorchidism in LCT. The clinical presentation, treatment, and additional follow-up in this case are highlighted. Long-term follow-up is necessary for these patients since bilateral congenital cryptorchidism may be linked to Leydig cell tumour years later in life. These tumours may appear differently clinically depending on the person. Any physical changes, hormonal tests, and imaging investigations should be immediately investigated for potential surgical resection and strict supervision.
Keywords
Leydig cell tumor; Bilateral congenital cryptorchidism;
Gynecomastia; Infertility; Testicular neoplasm
INTRODUCTION
Approximately of all malignancies in men are testicular
neoplasms. The stromal tumours of the sex cord, which
make up barely 4% of all testicular malignancies, are also
the rarest subset of these uncommon neoplasms. Leydig cell
tumours make up 1-3% of all adult testicular tumours and
are the most prevalent type of testicular stromal tumour,
accounting for roughly 75% to 80% of all cases [1]. Only
around 3% of LCT instances are determined to be bilateral;
the majority of LCT cases are unilateral and benign at
the time of presentation. The inguinal lymph nodes and
extranodal organs, such as the liver, lungs, and kidneys, can
be affected by distant metastasis, which is uncommon and
only discovered in around 10% of patients at presentation.
The most frequent areas of involvement are bones [2].
According to histology, the tumour is made up of a growth
of sizable polygonal tumour cells that are grouped in sheets
and have granular eosinophilic cytoplasm and conspicuous
nucleoli [3]. LCTs are special in that they can release
several hormones, including testosterone and its analogues,
or they can be hormonally inactive. Regardless of age,
patients with LCT may clinically appear with a painless
or painful testicular tumour [4]. However, children can
exhibit unilateral or bilateral gynecomastia as well as early
pseudo-puberty, and adults can exhibit erectile dysfunction,
a decline in libido, or infertility. In the 480 cases of LCT
that have been described in the literature, according to
Efthimiou's review, 12.5% of the cases have gynecomastia
and 29.2% of the cases have testicular masses [5]. Due to the
Despite a notable improvement in ultrasound technology,
the prevalence of LCTs appears to be increasing, and early
diagnosis of testicular incidentalomas need additional
testing. Uncertainty surrounds the aetiology of LCTs,
which appears to be multifactorial [6]. In our scenario,
cryptorchidism the absence of one or both testicles from
the scrotal sac is the underlying risk factor linked to the
development of LCT. It is linked to an increased risk of
testicular cancer and male infertility [7]. Although usually
unilateral, occurrences of bilateral cryptorchidism may exist
and have very occasionally been documented [8]. Here, we
present a case of bilateral congenital cryptorchidism in a
young adult guy with LCT who also had gynecomastia and
infertility [9]. A 36-year-old man from Quetta, Pakistan,
who has a primary testicular defect in spermatogenesis and
is morbidly obese presented to our facility for the first time
in September 2020 with the inability to have sex without
any trouble in achieving an erection on stimulation for the
previous two years. For the past three years, he has also
complained of increased swellings in both of his breasts.
He had left orchidopexy 20 years prior due to a history of
left undescended testis from birth. He had never smoked or
used drugs in the past. He had neither a history of cancer
nor cryptorchidism in his family [10]. All of his vital signs
appeared normal during a general physical examination,
but according to Simon's categorization, he exhibited
apparent grade II bilateral gynecomastia. It showed thick
lumps coming out of the nipples. Furthermore, a scan
of his entire body revealed no palpable testicular bulge
and a small scrotal sac. The remainder of the systemic
analysis was uneventful. A bilateral mammography was
done, and the results revealed a right mid-inguinal canal
heterogeneous mass with an oval hypoechoic shape on
breast imaging-reporting and data system. His hormonal
profile was determined by pertinent blood tests, which
also indicated his serum testosterone level. He was told to
return to the clinic for follow-up care with the findings of
additional investigations, but he neglected to do so and
later present in January 2021 with severe lower abdomen
pain and a growth in the size of the right testes. A pelvic
magnetic resonance scan was done, and it revealed an
empty scrotum. With an oval-shaped signal intensity
focus along the right inguinal canal suggestive of the right
ectopic testis, a small abnormal signal intensity focus
with homogenous enhancement highly suggestive of the
neoplastic lesion, and another abnormal signal intensity
area along the left inguinal vessels suggestive of the left
atrophic ectopic testis, the sac has these characteristics on
both sides. Venous leakage was visible on penile Doppler
without vascular insufficiency. His case was discussed in a
multidisciplinary tumour board meeting, and the patient
was given a full explanation of his options, including
close monitoring with a history and physical exam, 3-6
monthly repeats of serum tumour markers, hormonal
profile, and imaging studies, vs. a right orchiectomy and
observation for the left testis. Ultimately, however, the
patient decided to undergo surgery. His subsequent right
radical orchiectomy went without incident. In our facility
in January 2021. The right testis was found to be small,
floppy, and free of any hard masses just lateral to the pubic
tubercle. The histopathology of the testis was consistent
with LCT staining positive for melanin A and inhibin
and negative for stage I, pT1aN0M0, limited to the testes
with no involvement of the spermatic cord or resected
margins, and free of lymph vascular invasion. Following
the orchiectomy, he was hemodynamically stable, so he was
discharged. He was first summoned back to the clinic in a
week to have the wound evaluated, and then he was told
to return in three months for a physical exam and repeat
testosterone levels. Three months later, when he went
to the clinic, his serum testosterone was. Upon physical
examination, he revealed an empty scrotal sac. However,
there was a high recurrence rate and surgical removal of
the fabella was done in these cases. Some studied reported
good results postoperative with a short follow up period,
small number of patients and the lack of control group.
There was also a case whose pain symptoms improved after
the operation but the pain only went away completely after
a year. Therefore, we report a case of a 19-year-old male
patient, a Vietnamese professional football player with
fabella syndrome; he failed conservative treatment after 6
months and underwent surgery to remove the fabella. 12 weeks post-operation, he was able to return to training and
competition.
MATERIAL AND METHODS
A detailed description of the patient's clinical presentation
is provided, including the history of gynecomastia and
primary infertility. The physical examination findings
and relevant laboratory investigations, such as hormone
levels and imaging studies, are discussed. The diagnostic
workup led to the identification of bilateral congenital
cryptorchidism and a unilateral Leydig cell cancer.
Management and Treatment
The management approach for this patient involved
a multidisciplinary team, including urologists,
endocrinologists, and oncologists. The treatment plan
encompassed surgical intervention for cryptorchidism,
hormonal therapy for Leydig cell cancer, and fertility
preservation options. The rationale behind the chosen
treatment strategies is discussed, taking into account the
patient's specific circumstances and the need for long-term
follow-up.
Outcome and Follow-up
The case study provides information on the patient's
response to treatment, including the resolution of
gynecomastia, restoration of hormonal balance, successful
fertility preservation, and the absence of cancer recurrence
during the follow-up period. The importance of ongoing
monitoring and surveillance is emphasized to detect
potential complications or disease recurrence.
RESULTS
Gynecomastia refers to the enlargement of breast tissue
in males. It can occur due to hormonal imbalances,
certain medications, or underlying medical conditions.
Gynecomastia is relatively common and can affect males of
any age. It is often benign but may sometimes be associated
with an underlying medical condition. Cryptorchidism is a
condition in which one or both testicles fail to descend into
the scrotum [Fig.1].
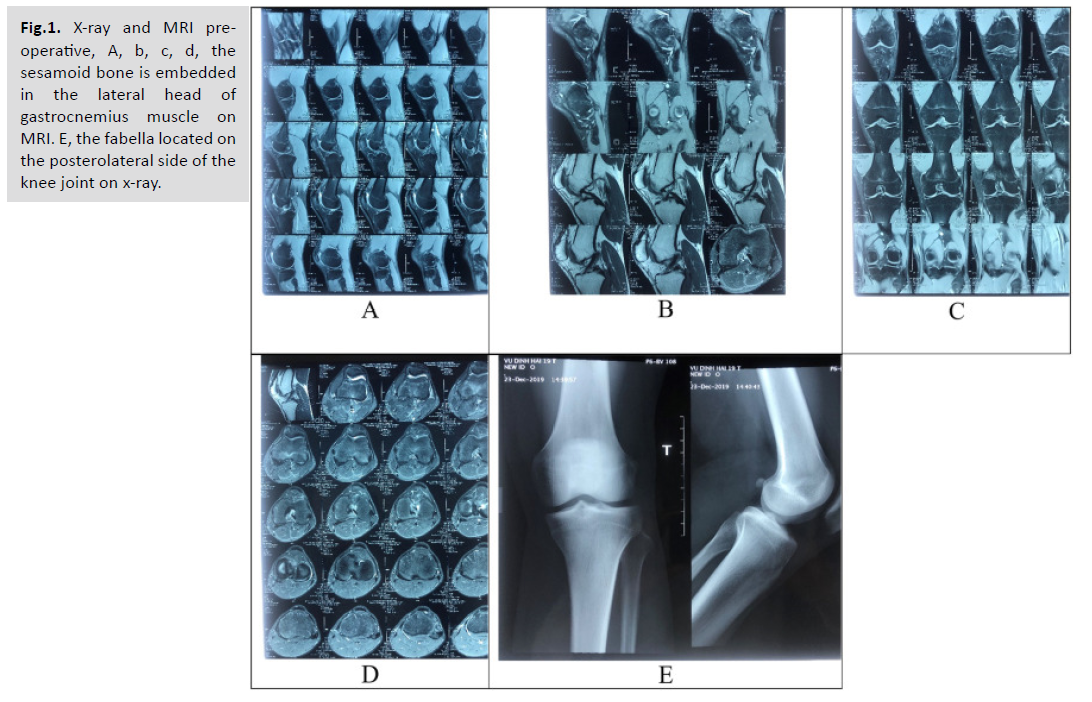
Fig.1. X-ray and MRI preoperative,
A, b, c, d, the
sesamoid bone is embedded
in the lateral head of
gastrocnemius muscle on
MRI. E, the fabella located on
the posterolateral side of the
knee joint on x-ray.
It is a common condition in newborns and can often
resolve on its own within the first few months of life.
However, if the testicles do not descend spontaneously,
treatment such as hormonal therapy or surgery may be
required. Cryptorchidism is associated with an increased
risk of infertility and testicular cancer. Leydig cell cancer
is a rare type of testicular cancer that arises from Leydig
cells, which are responsible for producing testosterone.
It typically affects adult males, and the most common
symptom is the presence of a testicular mass or swelling.
Leydig cell cancer is usually treated with surgical removal of
the affected testicle and may require additional treatments
such as radiation or chemotherapy, depending on the stage
and characteristics of the cancer [Tab.1].
| Empty Cell |
Kuur E. 1986 [15] |
Zenteno B. 2010 [4] |
Loscos S. 2020 [3] |
| Number of patients |
1 |
1 |
1 |
| Level of activity |
Soccer player |
Runner |
Swimmer |
| History of trauma |
No |
No |
No |
| Symptoms |
3–4 years history of intermittent posteriolateral knee pain and slight swelling, painful in knee extension |
Posteriolateral knee pain after running a distance longer than 2 km |
Posteriolateral knee pain when walking during the knee extension phase and when turning over and kicking against the water |
| Conservative treatment |
Injection of steroid and anti-inflammatory medication |
Local injection of steroid. Physical therapy: ultrasound, laser and ozone therapy |
Manual therapy, muscular strengthening, masotherrapy and radial shock waves |
| Operative treatment |
Open fabellectomy |
Open fabellectomy |
Open fabellectomy |
| Follow |
2.5 years |
4 months |
3 months |
| Symptoms post operation |
Pain free |
Pain free |
Pain free |
| Activity post operation |
Work and compete in sports |
Participate in high performance national and international competitions. |
|
Tab.1. Details derived from three
case reports on PubMed database.
DISCUSSION
An Adult Presenting With Gynecomastia and Primary
Infertility Had Bilateral Congenital Cryptorchidism and a Unilateral Leydig Cell Cancer: A Case Study. The case
study presented a rare and complex clinical scenario in
which a male patient exhibited gynecomastia and primary
infertility, ultimately leading to the diagnosis of bilateral
congenital cryptorchidism and unilateral Leydig cell cancer.
This discussion aims to explore the implications of this
case, including the association between these conditions,
the challenges in diagnosis, and the management strategies
employed. The coexistence of gynecomastia, primary
infertility, cryptorchidism, and Leydig cell cancer in a
single patient is a unique finding. Although each condition
can occur independently, their simultaneous presence
raises questions about potential underlying etiological
factors. Hormonal imbalances, genetic predisposition, and
disruptions in testicular development have been proposed
as potential contributors. However, more extensive research
is necessary to establish the precise mechanisms linking
these conditions. Diagnosing this complex presentation can be challenging, as each component requires thorough
evaluation. Gynecomastia, characterized by breast tissue
enlargement, is commonly caused by hormonal imbalances,
medications, or underlying medical conditions. Primary
infertility may have various causes, including testicular
abnormalities, hormonal disturbances, or obstructive
factors. Cryptorchidism refers to the failure of one or
both testes to descend into the scrotum, and Leydig cell
cancer is a rare form of testicular cancer arising from Leydig
cells, which produce testosterone. The diagnostic workup
for this case involved a multidisciplinary approaches,
including hormone analysis, imaging studies, and surgical
exploration. Hormone levels, such as testosterone and
estradiol, were evaluated to assess hormonal imbalances
contributing to gynecomastia and primary infertility.
Imaging studies, such as ultrasound or magnetic resonance
imaging (MRI), were used to visualize the testes and
identify cryptorchidism or possible malignancies. Surgical
exploration confirmed the presence of bilateral congenital
cryptorchidism and unilateral Leydig cell cancer. The
management of this case required a multidisciplinary team,
involving urologists, endocrinologists, and oncologists.
Treatment strategies were tailored to address each
component of the presentation. Surgical intervention
was performed to correct the cryptorchidism, aiming to
bring the undescended testes into the scrotum to prevent
potential complications and improve fertility. Hormonal
therapy, such as androgen replacement therapy or
antioestrogens, was employed to address gynecomastia and
restore hormonal balance. For the unilateral Leydig cell
cancer, appropriate treatment, such as surgical excision and
adjuvant therapy, was administered to achieve complete
cancer removal and prevent recurrence. Long-term followup
and surveillance are crucial in cases involving Leydig
cell cancer to monitor for recurrence or metastasis. In the
presented case, the patient showed positive outcomes,
including resolution of gynecomastia, restoration of
hormonal balance, successful fertility preservation, and no
evidence of cancer recurrence during the follow-up period.
However, continued monitoring is essential to detect
any potential complications or disease progression. This
case study highlights the importance of a comprehensive
evaluation in patients presenting with gynecomastia
and primary infertility. The simultaneous presence of
cryptorchidism and Leydig cell cancer emphasizes the need
for thorough investigations to identify potentially serious
underlying conditions. The successful management of
this case highlights the importance of a multidisciplinary
approach to address each component appropriately. While this case study provides valuable insights, it is important
to note that it represents a single case and may not be
generalizable to all patients. Further research involving
larger cohorts and longitudinal studies is needed to explore
the association between gynecomastia, primary infertility,
cryptorchidism, and Leydig cell cancer.
CONCLUSION
The case study presented a rare and complex clinical
scenario involving an adult male with gynecomastia and
primary infertility, leading to the diagnosis of bilateral
congenital cryptorchidism and unilateral Leydig cell
cancer. The coexistence of these conditions highlights
the importance of a comprehensive evaluation and a
multidisciplinary approach to diagnosis and management.
This case underscores the need for a thorough diagnostic
workup in patients presenting with gynecomastia and
primary infertility to identify potential underlying
pathologies. It also emphasizes the significance of
collaboration among urologists, endocrinologists, and
oncologists in formulating an appropriate management
plan. The successful management of this case involved
surgical correction of cryptorchidism, hormonal therapy for
gynecomastia and hormonal imbalances, and treatment for
Leydig cell cancer. Long-term follow-up and surveillance
are crucial to monitor for complications and ensure early
detection of recurrence or metastasis. Although this case
provides valuable insights, it is important to recognize its
limitations as a single case study. Further research involving
larger cohorts and longitudinal studies is necessary to better
understand the underlying etiology, optimize diagnostic
strategies, and establish evidence-based management
guidelines for patients with concurrent gynecomastia,
primary infertility, cryptorchidism, and Leydig cell cancer.
In conclusion, this case study highlights the complexity
and challenges in managing the simultaneous occurrence
of gynecomastia, primary infertility, cryptorchidism, and
Leydig cell cancer. It underscores the importance of a
comprehensive evaluation, multidisciplinary collaboration,
and long-term follow-up to ensure accurate diagnosis,
appropriate treatment, and optimal patient outcomes.
Fabella syndrome is a rare cause of posterolateral knee pain.
Definitive diagnosis of Clinical examination combined
with appropriate imaging to rule out all other causes of
posterolateral knee pain. We reported a good result of the
patient underwent surgical after failure of conservative
therapy. Our report contributes experience in the diagnosis
and the treatment strategy for Fabella syndrome.