Hanbyul Choi1, Hyo Ju Lee2, Eun-Kyung Jeong3, Christopher C Lee4, Ho Jung Kim5*, Adam J Singer4 and Han Ho Do6
1School of Medicine, St.George’s University, Grenada, West Indies
2Department of Emergency Medical Technology, Gyeongbuk Provincial College, South Korea
3Department of Emergency Medical Technology, Ho Nam University, South Korea
4Department of Emergency Medicine, Stony Brook University Medical Center, NY, USA
5Department of Emergency Medicine, Bucheon Hospital of Soonchunhyang University, South Korea
6Department of Emergency Medicine, Ilsan Hospital of Dongkuk University, South Korea
*Corresponding Author:
Ho Jung Kim
Department of Emergency Medicine, Bucheon Hospital of Soonchunhyang University
Jomaru-ro Wonmi-gu, Bucheon City, Gyenggi-do, South Korea
E-mail: lovelydr@schmc.ac.kr
Tel: 82236761333
Received date: February 01, 2016; Accepted date: February 10, 2016; Published date: February 15, 2016
Citation: Choi H, Lee HJ, Jeong EK, et al. An Observational Study on Importance of CPR Provider Medical Safety: Hemodynamic Changes and Fatigue in Young Healthy Adults after Multiple Cycles of CPR . Arch Med. 2016, 8:3
Title: An Observational Study on Importance of CPR Provider Medical Safety: Hemodynamic Changes and Fatigue in Young Healthy Adults after Multiple Cycles of CPR.
Background: Cardiopulmonary Resuscitation (CPR) guidelines emphasize delivery of effective chest compressions but do not strongly address the medical safety of CPR providers. We determined the effects of chest compressions on healthy adult firefighters’ symptoms, hemodynamics, and electrocardiography after performing multiple cycles of CPR.
Methods and Findings: Healthy adult firefighters were trained in CPR (compression: ventilation= 30:2, compression rate: at least 100/min, compression depth: at least 2 inches) and performed CPR on mannequins. Provider vital signs (blood pressure, heart rate, respiratory rate, O2 saturation, end-tidal CO2 tension, and pulse pressure), electrocardiography, and fatigue scores (on a scale of 0 to 10 from none to worst) were determined immediately before CPR (T1), after 5 cycles of CPR (T2), and after 10 cycles of CPR (T3). In addition, the presence of clinical symptoms (e.g., shortness of breath, dizziness) among the providers was determined after CPR. 39 firefighters participated in the study. Their mean age was 35.54 ± 10.26 years. Many providers developed fatigue, shortness of breath, and dizziness. Significant changes in heart rate (ðÂÂ’‘=0.000), respiratory rate (ðÂÂ’‘=0.010), end-tidal CO2 ( ðÂÂ’‘=0.000), O2 saturation (ðÂÂ’‘=0.000), and pulse pressure (ðÂÂ’‘=0.000) were observed after both 5 and 10 cycles of CPR. One participant developed sinus dysrhythmia and premature ventricular contractions (PVC) after 10 cycles of CPR.
Conclusions: Delivery of chest compression results in fatigue and hemodynamic alterations in many young healthy adults after performing 5 or 10 cycles of CPR. To optimize medical safety of CPR providers, guidelines and education should take into account the age and presence of cardiac disease of CPR providers.
Keywords
Cardiopulmonary Resuscitation; Chest compression; Vital Signs;Medical Safety; Pulse pressure
Introduction
Immediate delivery of cardiopulmonary resuscitation (CPR) by bystanders significantly reduces mortality in patients with sudden cardiac arrest since severe brain damage occurs as early as 4-6 min after cardiac arrest [1,2]. As a result, CPR training has targeted the general population without any medical background with several studies evaluating the optimal methods for achieving this goal [3-5].
Several studies have demonstrated an association between provider exhaustion and poor quality of CPR and there is evidence that switching roles during the delivery of CPR can reduce fatigue [6-10]. CPR providers can easily become exhausted, especially when only one rescuer is available or when rescuers are female or relatively thin [11,12]. Moreover, in 2011, The Korean Association of CPR published a study demonstrating fatigue in middle-aged women providers resulting in a low quality of chest compressions despite following appropriate CPR recommendations [13]. However, few if any studies have paid particular attention to the medical safety of CPR providers while delivering CPR.
In addition, recent studies on the new CPR guidelines have found that emphasis on chest compressions has resulted in low quality performance due to fatigability among CPR providers [8,14]. Therefore, the current study was designed to evaluate the impact of performing multiple cycles of CPR on provider medical safety by assessing symptoms, fatigue, and hemodynamics.
Methods
Study design
We performed a prospective, observational study to determine the effects of performing chest compressions on CPR providers.
Study subjects
The study enrolled healthy adult firefighters with or without prior CPR training and experience. Informed consent was provided to participants, and this study was approved by institutional review board of Soonchunhyang University.
Study interventions
Participants were asked to fill out a pre-test survey and then they viewed a 2 min CPR education video clip produced by The Korean Association of CPR. Participants were connected to a device that monitored vital signs and 3-lead electrocardiogram (Lifepack® 15 Monitor/Defibrillator, Physio-Control, USA). Specific instructions on the rate (at least 100/min) and the depth (at least 2 inches) of chest compression component of CPR were emphasized and strictly supervised. After performing 5 cycles of CPR (1 cycle: compression: ventilation = 30:2) on a mannequin (SimMan® Essential Laerdal Company, Norway), the subjects were instructed to take a break, long enough for them to return to their resting state, prior to beginning another 10 cycles of CPR. A boardcertified emergency medicine physician was present throughout the experiment in case of any medical emergency among the participants.
Measurement
The subjective level of fatigue was measured on a verbal numeric scale from 0 (no fatigue) to 10 (most fatigue imaginable). Vital signs (blood pressure, heart rate, respiratory rate, O2 saturation, endtidal CO2 tension, and pulse pressure) and electrocardiography of providers were taken at rest immediately prior to CPR (T1), after 5 cycles of CPR (T2), and after 10 cycles of CPR (T3). Clinical symptoms after CPR were assessed by an open-ended question that asked symptoms that participants experienced during or after 10 cycles of CPR.
Data analysis
Binary data were summarized as numbers and percentage frequency of occurrence. Continuous data were summarized as means and standard deviations (SD) or medians and interquartile ranges (IQR). Participants were grouped into 3 categories based on BMI (Normal, overweight, and obese). The paired T-test and ANOVA were used to compare hemodynamic changes by number of CPR cycles and BMI. The X2 test was used to compare the occurrence of any ECG changes by number of CPR cycles and BMI. Pearson’s correlation was used to analyze the correlation between pulse pressure and ETCO2. A p-value less than 0.05 was considered statistically significant. SPSS (IBM, Armonk, NY, USA) for Windows version 21.0 was used for all statistical analyses.
Results
General subject characteristics
The total number of subjects participating in the study was 39. All of the subjects were currently employed firefighters. Of all participants, 38 subjects had taken a CPR course at least once in the past. The mean age of the participants was 35.54 ± 10.26 years and 84.6% of the subjects were male. The mean height and weight of the study subjects were 171.21 ± 6.74 cm and 69.18 ± 8.34 kg respectively. Based on BMI calculations, 18 of the subjects were overweight (25.0 – 29.9 kg/m2) and 7 were obese (30.0 - 39.9 kg/m2). One subject had a previous medical history of hypertension (Table 1).
| |
First responder, N=39 |
| Age (years) |
35.54 ± 10.26 |
| Sex |
|
|
| |
Males, No. (%) |
33 (84.6%) |
| |
Females, No. (%) |
6 (15.4%) |
| Height (cm) |
171.21 ± 6.74 |
| Weight (kg) |
69.18 ± 8.34 |
| BMI (kg/m2) |
23.57 ± 2.23 |
| |
Normal, No. (%) |
14 (35.9%) |
| |
Overweight, No. (%) |
18 (46.25) |
| |
Obese, No. (%) |
7 (18.0%) |
| CPR Training |
|
| |
Prior CPR training experience, No. (%) |
38 (97.4%) |
|   |
Less than 6 months since last training, No. (%) |
17 (43.6%) |
Table 1: Characteristics of the study subjects.
Hemodynamic and electrocardiographic changes
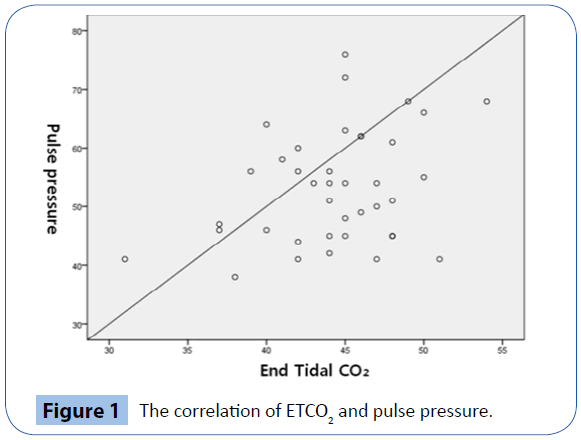
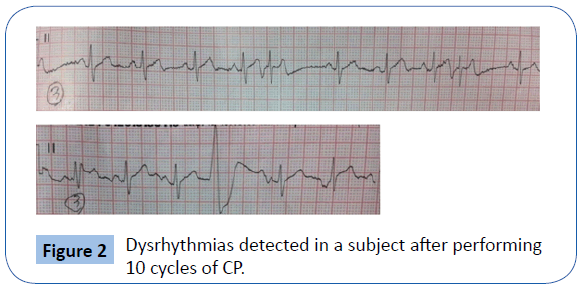
There were no statistically significant changes in blood pressure after both 5 cycles (T2) and 10 cycles of CPR (T3). However, there were significant changes in heart rate (p<0.001), respiratory rate (p=0.010), end-tidal CO2 (ETCO2) (p<0.001), O2 saturation (SPO2) (p<0.001), and pulse pressure (p<0.001). There were also significant changes in pulse pressure between T1 and T2. Between T1 and T3, significant changes were observed in both respiratory rate and pulse pressure (Table 2). Between T1, T2, and T3, there were significant changes in heart rate, SPO2, and ETCO2. The largest change was observed in heart rate between T1 and T3 (increased by 32.4/min). Median (IQR) pulse pressure was 46.0 (29-66) mmHg at T1, 53.0 (21-73) mmHg at T2, and 54.0 (38-76) mmHg at T3. Pulse pressure increased by 7.9 mmHg on average, and SPO2 decreased by 1.4% on average. There was a positive correlation between pulse pressure and ETCO2 after 10 cycles of CPR (r=0.327, p=0.042) (Figure 1). One participant developed sinus dysrhythmia and premature ventricular contractions (PVCS) after 10 cycles of CPR (Figure 2).
| |
Resting state
(T1) |
After 5 cycles
(T2) |
After 10 cycles (T3) |
p (N=39) |
| Systolic BP |
135.51 ± 11.29 |
140.87 ± 13.05 |
136.87 ± 14.73 |
0.163 |
| Diastolic BP |
90.23 ± 10.40 |
88.92 ± 10.91 |
88.67 ± 11.02 |
0.340 |
| Peak Heart Rate |
74.08 ± 11.40 |
103.79 ± 12.88 |
106.46 ± 16.04 |
<0.001 |
| peak Respiration Rate |
18.64 ± 4.73 |
21.03 ± 4.08 |
21.92 ± 5.55 |
0.010 |
| ETCO2 |
41.05 ± 4.41 |
45.92 ± 3.86 |
44.33 ± 4.40 |
<0.001 |
| SPO2 |
98.28 ± 1.39 |
97.23 ± 1.22 |
96.87 ± 1.64 |
<0.001 |
| Pulse pressure (mean) |
45.28 ± 6.93 |
51.95 ± 10.26 |
53.21 ± 9.61 |
<0.001 |
| Pulse pressure (median) |
46 (29-66) |
53 ( 21-73) |
54 (38-76) |
|
ECG
Dysrhythmia, No. (%)
Normal, No. (%) |
0 (0%)
39 (100%) |
0 (0%)
39 (100%) |
1 (2.6%)
38 (97.4%) |
1.000 |
ECG: electrocardiography
post-hoc test
Table 2: Hemodynamic changes by compression-ventilation cycle.
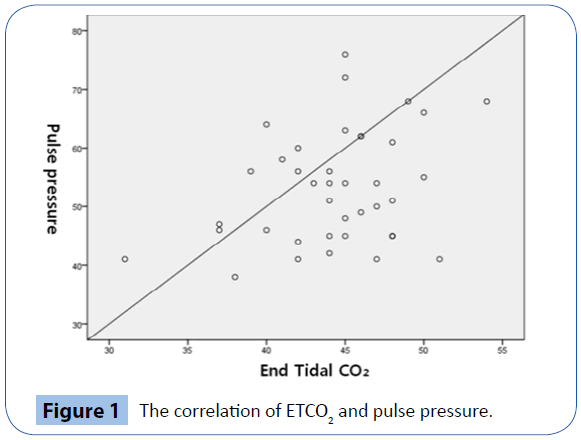
Figure 1: The correlation of ETCO2 and pulse pressure.
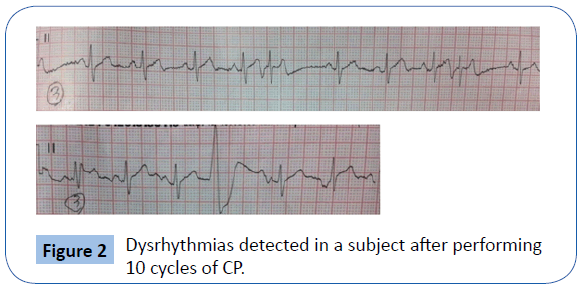
Figure 2: Dysrhythmias detected in a subject after performing 10 cycles of CP.
Significant differences were observed in SPO2 ( p=0.009) and respiratory rate (p=0.044) among the three BMI classes (Table 3). In particular, SPO2 dropped more between T1 and T3 in the normal BMI group (-2.36 ± 1.94) compared to the overweight group (0.57 ± 2.76) or the obese group (-1.44 ± 1.54).
| |
Normal
(N=14) |
Overweight
(N=18) |
Obese
(N=7) |
p(N=39) |
| Systolic BP |
2.29 ± 10.86 |
4.89 ± 10.52 |
7.14 ± 8.21 |
0.575 |
| Diastolic BP |
-4.00 ± 7.83 |
-3.11 ± 6.74 |
-3.86 ± 3.80 |
0.927 |
| Peak Heart Rate |
35.93 ± 11.89 |
32.33 ± 16.42 |
25.43 ± 9.58 |
0.278 |
| Peak Respiration Rate |
6.21 ± 6.67 |
1.89 ± 4.43 |
1.00 ± 4.08 |
0.044 |
| ETCO2 |
2.21 ± 4.64 |
4.44 ± 3.68 |
2.43 ± 3.91 |
0.271 |
| SPO2 |
-2.36 ± 1.94 |
-1.44 ± 1.54 |
0.57 ± 2.76 |
0.009 |
| Pulse pressure |
6.29 ± 10.76 |
8.00 ± 8.54 |
11.00 ± 9.00 |
0.539 |
ECG
Dysrhythmia, No. (%)
Normal, No. (%) |
0 (0%)
14 (100%) |
1 (5.6%)
17 (94.4%) |
0 (0%)
7 (100%) |
0.550 |
Normal: 18.5 Overweight: 25.0 Obese: BMI≥30
Table 3: Hemodynamic changes by BMI.
Clinical symptoms and fatigue after 10 cycles of CPR
Of all subjects, 13 participants (33.3%) experienced shortness of breath, 12 participants (30.8%) complained of hand pain, and 4 participants (10.3%) reported dizziness. The mean fatigue score was 6.84 ± 1.81 (Table 4).
| |
N (%) |
Mean±SD |
| Clinical manifestation, No. (%) |
|
|
| Shortness of breath? |
13 (33.3) |
|
| Dizziness |
4 (10.3) |
|
| Back hand problems |
12 (30.8) |
|
| Other |
2 (5.1) |
|
| None |
8 (20.5) |
|
| Mean fatigue score |
|
6.84±1.81 |
Table 4: Clinical manifestations and fatigue scores.
Discussions
Recent CPR guidelines issued by the American Heart Association (AHA) emphasize immediate delivery of chest compressions by bystanders so called “Hands-only CPR” (CPR without ventilation) [6]. In addition, in 2010, the AHA changed its recommendations on the depth and rate of compression from 38-51 mm to 50-60 mm and from 100/min to100-120/min respectively [6]. However, emphasis on chest compressions demands physical strength and may cause provider fatigue [15]. Therefore, the current study was specifically designed to assess the medical safety of the CPR provider, by studying the effects of chest compression on fatigue, symptoms, hemodynamics and ECG after performing multiple rounds of CPR.
As recent studies have demonstrated significant changes in vital signs after performing CPR, such as heart rate, ETCO2, and SPO2 or blood pressure and heart rate, [9,11] we found statistically significant changes in heart rate, respiratory rate, ETCO2, SPO2, and pulse pressure after 5 or 10 cycles of CPR. Especially, the current study found significant increases in pulse pressure after multiple cycles of CPR. Although it is normal physiologic phenomenon to have an increased pulse pressure after vigorous exercise, such as chest compression, this potentially is a clinically important finding since multiple studies have found that an elevated pulse pressure is associated with cardiovascular disease and increased mortality [16-19].
Increases in respiratory rate and ETCO2 combined with decreases in SPO2 are also of clinical relevance based on the fact that 33.3% of the participants reported difficulty in breathing after 10 cycles of CPR. Thierbach and colleagues asked subjects to perform CPR only by ventilation and claimed that artificial ventilation can adversely affect the CPR providers’ health due to hyperventilation [20]. However, Kim et al. demonstrated an increase in ETCO2 after CPR including both chest compressions and ventilation, [8] which is similar to our observations. This physiological phenomenon is normal response to excessive muscle use during chest compression, which causes a reduction in oxygen diffusion capacity and inadequate perfusion. However it can be potentially dangerous for CPR providers with background medical illness, such as cardiovascular disease.
In the current study, one male participant (height: 163 cm, weight: 69 kg, age: 50) with a prior history of hypertension, developed sinus dysrhythmia and premature ventricular contractions (PVCs) after 10 cycles of CPR (Figure 2). This participant also complained of difficulty breathing. In addition, his pulse pressure was slightly above normal prior to CPR and rose to 61 mmHg after 5 cycles of CPR. As noted earlier, increased pulse pressure has been shown to be associated with cardiovascular disease and increased mortality, [16-19] and in 1982 Memon and colleagues reported a case of fatal myocardial infarction following CPR training raising medical safety concerns in CPR providers [21]. The case reported here once again raises the potential danger of performing CPR.
Recent studies recommended switching roles in CPR every two minutes in order to prevent one rescuer from performing chest compressions for more than 5 cycles [7,10]. The current study supports this recommendation by finding that there were significant changes in vital signs after 5 cycles of CPR.
As recent studies found no association between physical characteristics of CPR providers and fatigability during CPR, [8,14] current study did not find any clinically significant association between BMI and health of CPR providers. Interestingly, current study found that individuals with normal BMI were associated with greater drop in SPO2 after CPR. This phenomenon may be explained as healthier people performed CPR more vigorously utilizing more oxygen.
Limitations
The following limitations should be considered when interpreting the results of the current study. First, the study was conducted using a mannequin and was not a live clinical scenario. Consequently, participants did not experience as much urgency, stress, or fatigue as they would in an actual emergency condition. Second, subjects were healthy firefighters who may not be representative of the general bystander population. Third, the device used to monitor vital signs was not able to detect continuous hemodynamic changes throughout CPR performance. Future studies should include a wider variety of study subjects and record vital signs and ECG continuously while performing CPR. Fourth, although the rate and the depth of chest compression was strictly supervised, an objective method was not utilized in current study on measuring the depth of compression. Future study would be significantly benefitted if the intervention included an objective method of controlling depth of chest compression by minimizing person to person variation in intensity of CPR
Conclusions
Significant fatigue, symptoms, and changes in hemodynamic parameters were noted among healthy adult firefighters after delivery of 5 and 10 cycles of CPR on a mannequin. In order to optimize medical safety of CPR providers, CPR guidelines and education should emphasize medical safety of CPR providers by taking into account the age and the presence of cardiac disease of CPR providers.
9573
References
- Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, et al. (2004) Advandced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med 351: 647-656.
- Platz E, Scheatzle, Pepe PE, Dearwater SR (2000) Attitudes towards CPR training and-performance in family members of patient with heart disease. Resuscitation 47: 273-280.
- Anderson ML, Cox M, AI-Khatib SM, Nichol G, Thomas KL, et al. (2014) Rate of cardiopulmonary resuscitation training in the United States. JAMA Intern Med 174: 194-201.
- Kim HJ, Lim DS, Lee JO, Lee MK, Kim KY, et al. (2007) Selection of target age for School education of cardiopulmonary resuscitation using Video self-instruction program. J Korean Soc Emerg Med 18:196-201.
- Lee CW, Ahn JY, Cho GC, Lee WW, Son YD, et al. (2010) E-learning can be Helpful for Mastering basic life support skills on public. J Korean Soc Emerg Med 21:423-428.
- Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, et al. (2010) 2010 American Heart Association Guidelines for cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122: S685-705.
- Yi KH, Park SO, Lee KR, Kim SC, Jeong HS, et al. (2012) Comparison of the Alternating Rescuer method between Every Minute and Two Minutes During Continuous Chest Compression in Cardiopulmonary Resuscitation According to the 2010 Guidelines. J Korea Soc Emerg Med 23: 455-459.
- Kim YB, Choi SM, Kim YM, Lee WJ, Park KN, et al. (2006) Effect or Single-Rescuer Fatigue on the Quality if Cardiopulmonary Resuscitation with 30:2 and 15:2 Compression-to-ventilation Ratios. J Korea Soc Emerg Med 17:519-527.
- Pozner C, Almozlino A, Poole S, McNamara D, Barash D (2009 ) Abstract P168: Early Markers of Rescuer’s Fatigue. Circulation 120: S1478.
- Choi UJ (2008) Physiology changes on the rescuer and efficiency of CPR in the increased chest compression. Korean J Emerg Med Ser 12:43-53.
- Jang MS, Tak YJ (2013) The variation of elapsed time on fatigue and quality of single rescuer cardiopulmonary resuscitation. Korean J Emerg Med Ser 17: 9-19.
- Hong DY, park SO, Lee KR, Baek KJ, Shin DH (2012) A different rescuer changing strategy between 30:2 cardiopulmonary resuscitation and hands-only cardiopulmonary resuscitation that considers rescuer factor: A randomized cross-over simulation study with a time-dependent analysis. Resuscitation 83: 353-359.
- Kim GN, Choi SS, Choi SW (2013) Comparison on the Quality and fatigue of hands only CPR according to the presence or absence of verbal counting by some middle-aged women. Journal of the Korea Academia-Industrial cooperation Society 14: 1320-1329.
- Yannopoulos D, Aufderheide TP, Gabrielli A, Beiser DG, McKnite SH, et al. (2006) Clinical and hemodynamic comparison of 15:2 and 30:2 compression-to-ventilation ratios for cardiopulmonary resuscitation. Crit Care Med 34: 1444-1449.
- Lucia A, de las Heras JF, Perez M, Elvira JC, Carvajal A, et al. (1999) The importance of physical fitness in the performance of adequate cardiopulmonary resuscitation. Chest 115: 158-164.
- Franklin SS, Khan SA, Wong ND, Larson MG, Levy D (1999) Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham study. Circulation 100: 354-360.
- Mitchell GF, Moye LA, Braunwald E, Rouleau JL, Bernstein V, et al. (1997) Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. Circulation 96:4254-4260.
- Cho SW (2005) Correlation between the pulse pressure and IMT (intra-media wall thickness) of the carotid artery in hypertension patients. Unpublished master's thesis. The graduate school of Chung-Ang University, Seoul, Korea.
- Domanski M, Norman J, Wolz M, Mitchell G, Pfeffer M (2001) Cardiovascular Risk Assessment Usion Pulse Pressure in the First national Health and Nutrition Examination Survey (NHANES ?). Hypertension 38:793-797.
- Thierbach AR, Wolcke BB, Krummenauer F, Kunde M, Janig C, et al. (2003) Artificial ventilation for basic life support leads to hyperventilation in first aid providers. Resuscitation 57:269-277.
- Memon Am, Salzer JE, Hillman EC Jr, Marshall CL (1982) Fatal myocardial infarct following CPR training: the question of risk. Ann Emerg Med 11: 322-323.