Olfa Slimani*, Gargouri Linda, Ben Temim Riadh, Makhlouf Tahar, Mathlouthi Nabil and Attia Leila
Department of Gynecology, Charles Nicolle Hospital, Tunisia
*Corresponding Author:
Olfa Slimani
Department of Gynecology
Charles Nicolle Hospital, Tunisia
Tel: 0021629029929
E-mail: slimani_olfa@yahoo.fr
Received Date: 04 October 2016; Accepted Date: 10 December 2016; Published Date: 14 December 2016
Citation: Slimani O, Gargouri L, Riadh BT, et al. Angiomyofibroblastoma (AMFB) of the Vagina: A Case Report. Arch Can Res. 2016, 4: 4.
Keywords
Angiomyofibroblastoma; Mesenchymal tumors; Vagina
Introduction
Angiomyofibroblastoma is a rare, recently described, soft tissue tumour that occurs mainly, but not exclusively, in the vulval region of premenopausal women [1]. While majority of the tumors are encountered in the vulva, 10% to 15% of them occur in the vagina, occasionally in the perineum and the inguinal region while rare reports of fallopian tube lesions are also found.
These tumors are commonly seen in women of childbearing age as well as in middle aged or peri menopausal women [1].
Differential diagnosis of mesenchymal neoplasms in the vulvovagina includes an array of lesions that are bland and overlapping in both their morphology and immunohistochemistry. In addition to their rarity, this creates a significant dilemma in making the correct diagnosis. Among these, aggressive angiomyxoma and cellular angiofibroma are the important mimickers of AMF.
Case Report
A 41-year-old woman gravida 2, para 1 presented to the gynecology department with complains of dyspareunia since, 6 weeks. She has no medical or surgical history. On clinical examination, a 6 cm lesion was found arising from the middle one-third of the left posterior vaginal wall.
Pelvic and abdominal Ultrasonography were normal. Perineal ultrasonography showed a 6 cm × 5.5 cm heterogeneous mass which prolapsed laterally in Douglas, both ovaries are normal. The patient underwent simple total excision. She has been discharged after 5 days in a good health. The pathological examination confirmed the diagnosis of AMF.
Discussion
AMF is a rare, benign, soft-tissue tumor that shows myofibroblastic differentiation and represents neoplastic proliferation of stromal cells [1]. AMF was first described by Fletcher et al. in 1992. AMF is composed of myofibroblastic cells and prominent thin-walled blood vessels within a fibromxyoid stroma [2]. Following that, several reports had been published where majority was vulvo-vaginal origin [3,4].
Its cause and pathogenesis are unknown at present. Since AMF is rare, no statistical data are available about its incidence in the general population. Most cases of AMF are benign, and only one case with sarcomatous transformation has ever been reported. A rare lipomatous variant of AMF with local invasion has also been reported.
In most reports, AMF has occurred in women aged between 20 and 50 years, i.e., during the reproductive years. In our case, the patient is aged 41 years old.
There are very rare reports of AMF occurring in male patients. In most patients, AMF presents as a painless neoplasm located in the superficial regions of the lower female genital tract, such as the vulva and vagina, and are therefore easily detected. Tumors arising in the cervix, uteri, or urethral region sometimes present with obstructive symptoms. Tumors in the pelvis, iliac fossa or peritoneal cavity are extremely rare, and usually grow insidiously and reach a massive size before they are detected. Their greatest dimensions have ranged from 3.8 cm to 25 cm. To our knowledge, only four cases of pelvic AMF have been reported at least so far [5].
Several reports have analyzed the imaging features of AMFs. On perineal ultrasonography, AMFs appear as a soft-tissue mass with inhomogeneous mixed echogenicity, which corresponds to the cellular inhomogeneity found on histopathological examination. Therefore, the ultrasonographic characteristics of AMFs may help to differentiate them from other mesenchymal neoplasms. On CT imaging, AMFs most likely show moderate-to-strong enhancement, which may reflect the prominent vascularity of these tumors.
Immunohistochemistry showed that the tumor expressed estrogen and progesterone receptors, which suggests that it might have originated as a neoplastic proliferation of hormonally responsive mesenchymal cells. In our case, we report a case of vaginal AMF. It was firm, pearly white in color. Characteristic histological features of angiomyofibroblastoma were appreciated. Immunohistochemical staining showed strong positivity of the stromal cells for desmin and vimentin. There was no staining of stromal cells for actin and S 100 protein. The blood vessels were well-highlighted by staining with SMA. Diffuse strong positivity of stromal cells for ER and PR receptors was noted.
Because of their location, AMFBs could be mistaken for bartholin cysts or lower genital tract lipomas, causing delays in diagnosis and treatment [6].
Differential diagnosis of the vulvar mass includes other benign tumors such as cellular angiofibroma, fibroepithelial stromal polyp, or superficial angiomyxoma. These benign mesenchymal tumors are mostly found at vulvovaginal area and organize a distinctive disease entity [7].
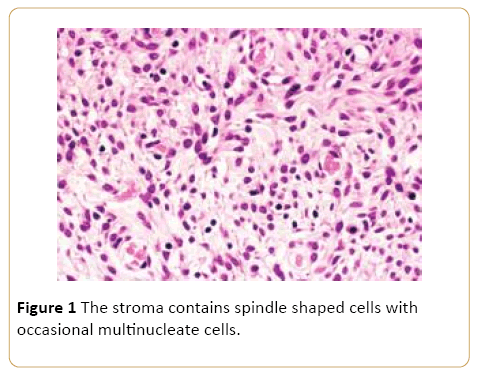
Aggressive angiomyxoma(AAM) is most likely to be confused with AMF because it shares many features with AMF including age at presentation, location, clinical manifestations, and pathological entities. However, AAM presents as a malignant, locally infiltrative, non-metastasizing stromal neoplasm with a strong tendency to recur. On microscopic examination, AMFs generally show much higher cellularity, more numerous blood vessels and more frequent plump or short spindle-shaped cells (Figure 1) in contrast, AAM cells are sparsely and diffusely distributed, without the characteristics of alternating density and aggregation around small blood vessels [4]. AAMs show more distinctive myxoid degeneration than AMFs. AMFs are characterized by the expression of vimentin, desmin and CD34, suggesting an undifferentiated mesenchymal tumor with preferential myofibroblastic differentiation. Desmin expression was previously thought to be specific for AMFs, but positive expression of desmin has been found in some cases of AAMs. Most AAMs are also positive for estrogen and progesterone receptors [8]. Hence, desmin, estrogen receptor and progesterone receptor are no longer considered reliable markers for distinguishing AAMs from AMFs. After surgical treatment, 30% of AAMs have been found to relapse within 2 years [9,10].
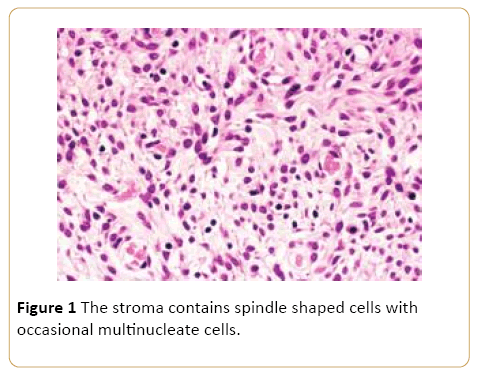
Figure 1: The stroma contains spindle shaped cells with occasional multinucleate cells.
Since the morphology and IHC markers of AMF are similar to those of AAM, differentiation between these two tumors is largely based on the appearance of the tumor margins (AMFs AMFB’s treatment is always simple excision. It is curable with surgical simple excision and no recurrence in the follow-up [11], which confirms the benign nature of AMF. AMF shows no propensity for infiltrative growth [12].
Conclusion
Although the exact nosologic position of AMF is still surrounded by some controversy and requires further elucidation, we conclude that our case represents the eighth report of AMF of the vagina, based on its conventional histopathologic and immunophenotypic features. Simple excision appears sufficient for the surgical management of AMF, whereas wide excision after histological examination is needed for the management of the related AAM, which is associated with a high risk of local recurrence and infiltration.
17678
References
- Canales BK, Weiland D, Hoffman N, Slaton J, Tran M, et al. (2006) Angiomyofibroblastoma-like tumors (cellular angiofibroma). Int J Urol 13: 177-179.
- Banerjee K, Datta Gupta S, Mathur SR (2004) Vaginal angiomyofibroblastoma. Arch GynecolObstet 270: 124-125.
- Magro G, Salvatorelli L, Angelico G, Vecchio GM, Caltabiano R (2014) Lipomatousangiomyofibroblastoma of the vulva: Diagnostic and histogenitic considerations. Pathologica 106: 322-326.
- Magro G, Righi A, Caltabiano R, Casorzo L, Michal M (2014) Vulvovaginalangiomyofibroblastoma: morphologic, immunohistochemical, and fluorescence in situ hybridization analysis for deletion of 13q14 region. Hum Pathol 45: 1647-1655.
- Barat S, Tirgar-Tabari S, Shafaee S (2008) Angiomyofibroblastoma of the vulva. Arch Iran Med 11:224-226.
- Park JH, Shin MK, Lee M, Park ST, Park SH, et al. (2013) Angiomyofibroblastoma of the vulva: A casereport with literature review. Case Reports in Clinical Medicine. 2:221-224.
- Magro G, Caltabiano R, Kacerovská D, Vecchio GM, Kazakov D, et al. (2012) Vulvovaginalmyofibroblastoma: Expanding the morphological and immunohistochemical spectrum. A clinicopathologic study of 10 cases. Human Pathology. 43: 243-253.
- Stewart C (2009) Angiomyofibroblastoma of the vagina. Pathology 41: 199-200.
- Bae JM, Jee BC, Ku SY, Suh CS, Choi YM, et al. (2005) A case of vaginal angiomyofibroblastoma. Korean J ObstetGynecol 48:2745-2750.
- McCluggage WG, White RG (2000) Angiomyofibroblastoma of the vagina. J ClinPathol 53:803.
- Kanda M, SonoyamaA, Hirano H, Kizaki T, Ohara N (2014) Angiomyofibroblastoma of the vulva. Eur J GynaecolOncol35:77-80.
- Sims SM, Stinson K, McLean FW, Davis JD, Wilkinson EJ (2012) Angiomyofibroblastoma of the vulva: A case report of a pedunculated variant and review of the literature. J Low Genit Tract Dis 16:149-154.