Sachin Suresh Babu*, Amit Aslam Khan, Gaurav K Mittal, Sudhir P, Chindripu S and Laxmi K
Department of Neurology, St. Stephens Hospital, Delhi, India
*Corresponding Author:
Sachin Suresh Babu
Head of the Department of Neurology, St. Stephens Hospital, Neurology, Tis Hazari, Delhi, 110054, India
Tel: 8375938480
E-mail: sachinsuresh1977@gmail.com
Received date: August 31, 2016; Accepted date: September 06, 2016; Published date: September 09, 2016
Citation: Suresh Babu S, Aslam Khan A, Mittal GK, et al. Anterior Spinal Artery Thrombosis Following Trivial Trauma in A Young Girl-Case Report and Review of Literature. J Neurol Neurosci. 2016, 7:5. doi: 10.21767/2171-6625.1000144
Keywords
Anterior spinal artery; Thrombosis; Spinal angiography
Introduction
The typical clinical syndrome of ASA thrombosis was first described by Preobraschenski in 1904 and the anatomical substrate was pathologically defined by Spiller [1,2]. The combination of acute flaccid weakness of all four limbs with dissociated anaesthesia (involvement of the spinothalamic and sparing of the posterior column sensations) along with bladder involvement and severe pain is pathognomonic of this catastrophic illness. Patients may have associated involvement of the medulla and diaphragm [3]. MRI of the spine usually reveals long segment T2 and FLAIR hyper-intensities restricted to the anterior part of the spinal cord. The axial sections classically show an “owl-eye” appearance [4]. Treatment if initiated immediately can produce worthwhile results. Long term prognosis is not encouraging with residual disabilities being the norm.
Case Report
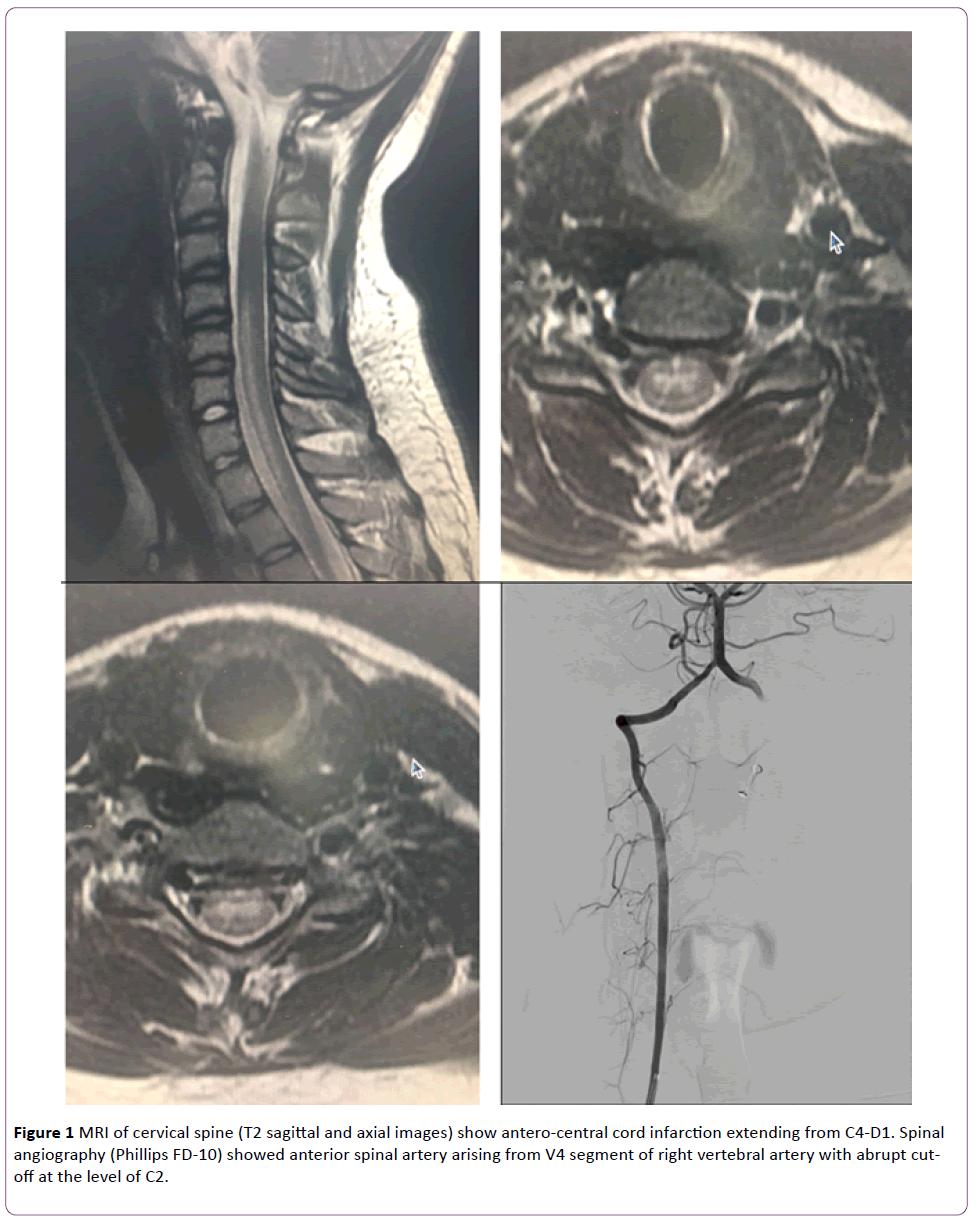
A 14 year old girl was apparently well until one day when her friend gently pulled her left hand and immediately she experienced a dull pain in the neck region. Over the next 1-2 hours, she started feeling weak in her legs but still managed to get back independently from school. She felt like lying down and after a couple of hours woke up to find herself completely paralysed. No movement was possible in the lower limbs, while some degree of movement remained in her upper limbs but not against gravity. She also could not turn around in bed without support. Incontinence of urine was reported an hour later and she denied any sensation of bladder fullness. 6-7 hours into the illness she started having pain in the shoulder region and limbs which were ill defined and poorly localized. She however did not report any loss of sensation. She had few episodes of giddiness and vomiting during the transit to the nearest hospital where she underwent neuroimaging of spine and brain which returned normal findings. Subsequently she was seen by many centers only to be labelled as dissociative disorder. Finally, she was seen at our center where a neurological examination revealed flaccid are flexic weakness of all four limbs (0/5 power in the lower limbs and 2/5 in the upper limbs) with trunk muscle weakness. Plantars were mute and abdominal reflexes were not elicitable. Spinothalamic sensations were impaired up to D6 level. Touch, two-point discrimination and vibration sense was normal. A clinical diagnosis of ASA thrombosis was made and patient was immediately initiated on anti-platelets and LMWH along with methyl prednisolone pulse therapy. 1.5 Tesla MRI spine was repeated which revealed anterior cord infarction extending from C4-D1. A digital subtraction angiography of the spinal vessels was performed using Phillips FD 10 for confirming the diagnosis. The ASA was seen to arise from the medial wall of V4 segment of right vertebral artery proximal to the vertebrabasilar junction. It was seen coursing in the midline in its proximal segment stopping short at the odontoid level (Figure 1). Rest of the vasculature was normal; artery of Adamkweiz was seen arising from D10 and was well visualized in its entire course up to cauda equina.
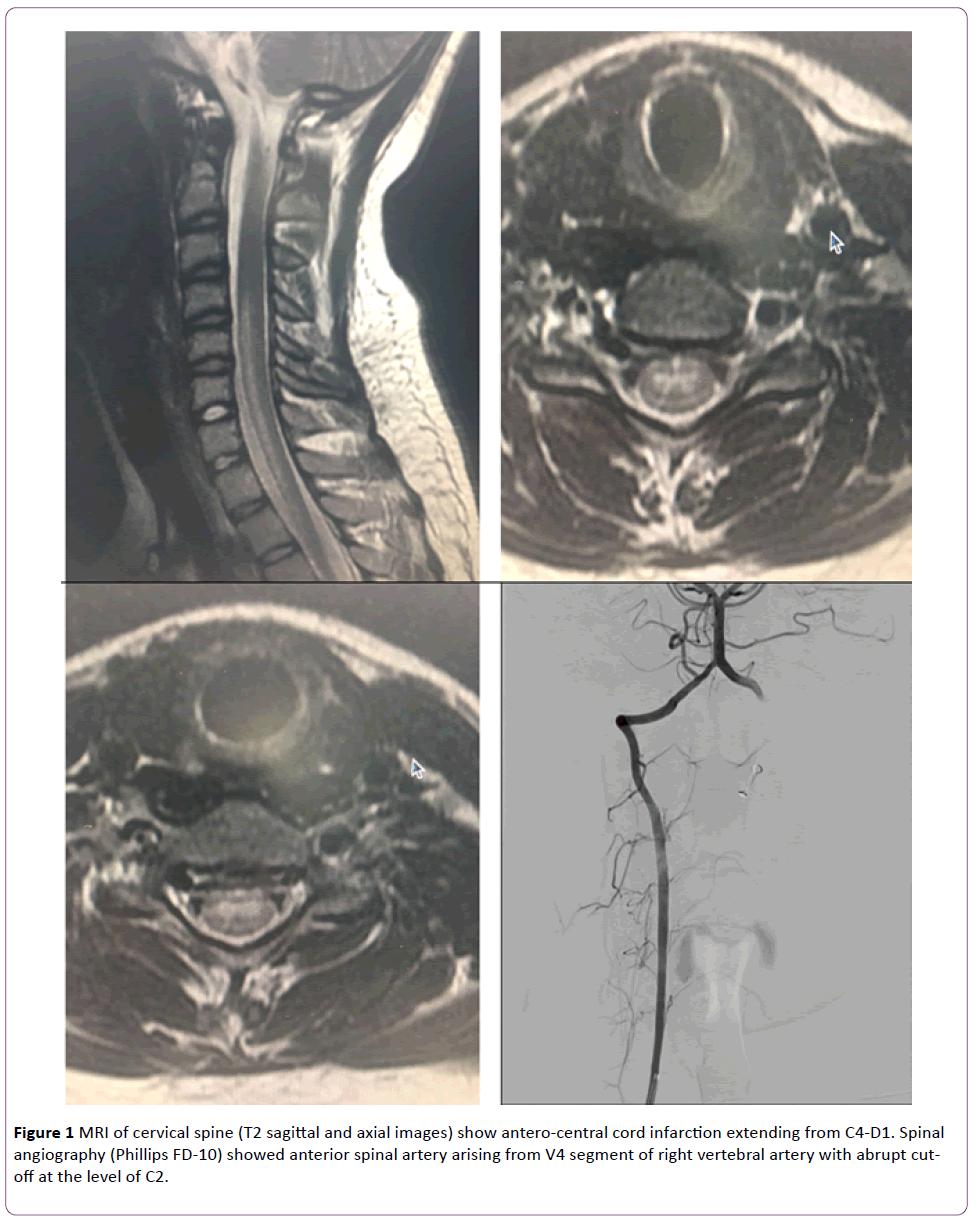
Figure 1 MRI of cervical spine (T2 sagittal and axial images) show antero-central cord infarction extending from C4-D1. Spinal angiography (Phillips FD-10) showed anterior spinal artery arising from V4 segment of right vertebral artery with abrupt cutoff at the level of C2.
As the patient presented beyond the therapeutic window for thrombolysis, conservative measures were continued. Routine blood work up, ANA profile, Anti phospholipid antibody screen, Hb electrophoresis, 2D ECHO, ultrasound abdomen, chest roentgenogram, thrombophilia work up were performed to identify any underlying abnormality but delivered negative results.
After 10 days of treatment, flicker of contractions was noted in the lower limbs, while truncal movement and upper limb power also showed mild degree of improvement.
Discussion
ASA syndrome refers to the typical neurological syndrome of acute painful flaccid paralysis with bladder involvement secondary to occlusion of the anterior spinal artery. As evidenced in the present case, the manifestations are secondary to infarction of the antero-lateral and central cord which comprises the anterior horn cells, cortico-spinal and spinothalamic tract along with fibers sub-serving higher control of bladder function. In addition these patients would have severe pain which can have features of radicular or tract pain. Posterior column sensations are characteristically preserved. A diligent search was made for any medullary involvement in view of giddiness and vomiting but repeated brain imaging did not reveal any diffusion restriction. Fulminant infarction of the higher cervical cord can produce postural hypotension due to autonomic involvement which could be an alternate explanation for these symptoms [3-5].
Apart from this classical presentation, the clinical setting in which the event occurred in the present patient was also quite unique. Thrombogenesis in our patient is most likely the result of shear stress resulting in endothelial injury to the anterior spinal artery. Salkov et al. has described the accounts of two patients with dislocation facture of cervical vertebra who developed thrombosis in the vertebral. Radicular and medullary arteries are as a result of endothelial inury. This is in fact a practical affirmation of the Virchow’s triad [6]. The other causes of this devastating syndrome include hypercoagulable states, anti-phospholipid antibody syndrome, Sickle cell anemia, Down syndrome, atlanto-axial dislocation, embolism and vasculitis which were ruled out by appropriate investigations. Adult patients usually have risk factors like hypertension, diabetes, smoking, hypercholesterolemia or degenerative spine disease. Aortic dissection and aortic surgeries can result in fulminant ASA thrombosis [3-5].
After the initiation of injury, the profound impact of the thrombosis needs to be explained This in turn is determined by the support offered to the ASA in supplying the cervical cord by the radiculo-medullary arteries predominantly arise from the vertebral and costo-cervical trunk. The largest of these branches is the artery of the cervical enlargement described by Lazorthes [7,8]. During angiography, we studied vertebral arteries, costocervical trunk, thyrocervical trunk, subclavian and the intercostals to search for the artery of Lazorthes which was conspicuously absent. The only other supply was from the right ASA arising from the lower segment of vertebral. This anatomical disadvantage could have culminated in this catastrophic infarction of the cervical cord [9].
Radiological identification of ASA thrombosis can be challenging as abnormalities may take time to surface as in this hapless patient who was suspected of having psychogenic weakness based on normal neuroimaging and hence was deprived of the opportunity of time-limited therapeutic interventions. Diffusion weighted MRI should be used to distinguish acute ischemia from other causes of myelitis [10]. Antero-central cord infarction can be seen on axial sections as the typical owl eye appearance [11].
The preferred therapy in acute phase would be the use of thrombolytic therapy (intravenous or intra-arterial) which was not considered in our patient as she had presented outside the window period of 4.5 hours [12]. In a previous report, administration of tissue plasminogen activator 0.9 mg/kg by intravenous route did not produce any immediate sustained change in neurological status but patient achieved a certain degree of functionality over time [13]. In another case report, a 71 year old man achieved dramatic recovery after receiving intravenous thrombolysis within 3 hours [14]. Antiplatelets and low molecular weight heparin can be used along with supportive measures and physiotherapy.
The overall prognosis remains poor with majority of patients ending up with some degree of disability [3-5,15,16]. In a study on the clinical outcome of ASA ischemia, 17.1% patients were ambulatory at the time of discharge which speaks against a universally bad prognosis. Patients who were younger were observed to have a better outcome [15]. Severe initial impairment and female sex were found to be independent predictors for poor outcome in another study both of which are factors which are going to play a significant part in the neurological recovery of our patient [16].
Conclusion
The case described here elaborates the clinical presentation and angiographic findings of ASA thrombosis precipitated by traumatic shear stress to the vessel. The challenges in diagnosis and patho-genetic mechanisms are discussed for a better understanding of this unusual cascade of events.
17297
References
- Preobrashenski PA (1904) Syphilitic paraplegia with dissociated disturbance of sensation. J Nevropat I Psikhiat Korsakova, Mosk 4: 394-433.
- Spiller WG (1909) Thrombosis of the cervical anterior median artery: syphilitic acute anterior poliomyelitis. J Nerv Ment Dis 36: 601-613.
- Kumral E, Polat F, Gulluoglu H (2011) Spinal ischaemic stroke: clinical and radiological findings and short-term outcome. Eur J Neurol 18: 232-239
- Masson C, Pruvo JP, Meder JF (2004) Spinal cord infarction: clinical and magnetic resonance imaging findings and short term outcome. J Neurol Neurosurg Psychiatr 75: 1431-1435.
- Salvador De La BS, Barca BA, Montoto MA, Ferreiro Velasco ME, Cidoncha DM, et al. (2001) Spinal cord infarction: prognosis and recovery in a series of 36 patients. Spinal Cord 39: 520-525.
- Salkov M, Zozylia N, Tsymbaliuk V, Dzyak L, Kozlov S, et al. (2015) New concept of the development of brainstem ischemia in the setting of occlusions of the vertebral arteries and radicular and medullary arteries in the presence of the cervical spinal injury. Brain Disord Ther 4: 193.
- Lazorthes G, Gouaze A, Zadeh JO, Santini JJ, Lazorthes Y, et al. (1971) Arterial vascularization of the spinal cord. J Neurosurg 35: 253-262.
- Salkov M, Tsymbaliuk V, Dzyak L, Rodinsky A, Cherednichenko Y, et al. (2015) New concept of pathogenesis of impaired circulation in traumatic cervical spinal cord injury and its impact on disease severity: Case series of four patients. Eur Spine J.
- Cheshire WP, Santos CC, Massey EW Jr (1996) Spinal cord infarction: etiology and outcome. Neurology 47: 321-330.
- Marcel C, Kremer S, Jeantroux J (2010) Diffusion-weighted imaging in non-compressive myelopathies: a 33-patient prospective study. J Neurol 257: 1438-1445
- Udiya AK, Shetty GS, Singh V, Phadke RV (2015) "Owl eye sign": Anterior spinal artery syndrome. Neurol India 63: 459.
- Mullen MT, Pisapia JM, Tilwa S, Messé SR, Stein SC (2012) Systematic review of outcome after ischemic stroke due to anterior circulation occlusion treated with intravenous, intra-arterial, or combined intravenous+intra-arterial thrombolysis. Stroke 43: 2350-2355.
- Müller KI, Steffensen LH, Johnsen SH (2012) Thrombolysis in anterior spinal artery syndrome. BMJ Case Rep 7: 2012.
- Restrepo L, Guttin JF (2006) Acute spinal cord ischemia during aortography treated with intravenous thrombolytic therapy. Tex Heart Inst J 33: 74-77.
- Salvador DLB, Barca BA, Montoto MA (2001) Spinal cord infarction: prognosis and recovery in a series of 36 patients. Spinal Cord 39: 520-525.
- Nedeltchev K, Loher TJ, Stepper F (2004) Long-term outcome of acute spinal cord ischemia syndrome. Stroke 35: 560-565.