Jacob Thyrsted1, Stine Yde Nielsen1, Christian Kanstrup Holm1*,Søren Helbo Skaarup2,Andreas Fløe Hvass2, Elisabeth Bendstrup2, Pernille Hauschildt2*and Sara Moeslund Joensen3
1 Department of Biomedicine, Aarhus University, Aarhus, Denmark
2 Deparment of Respiratory Diseases, Allergy, Aarhus University Hospital, Skejby, Denmark
3 Department of Clinical Microbiology, Lillebaelt Hospital, Vejle, Denmark
- *Corresponding Author:
- Christian Kanstrup Holm
Department of Biomedicine,
University of Aarhus,
Aarhus,
Denmark,
E-mail: holm@biomed.au.dk
Pernille Hauschildt
Department of Respiratory Diseases,
University of Aarhus,
Skejby,
Denmark,
E-mail: pernhaus@rm.dk
Received Date: December 01, 2021;Accepted Date: December 15, 2021; Published Date: December 22, 2021
Citation: Thyrsted J, NielsenSY, Holm CK, Skaarup SH, Hvass AF, et al. (2021) Anti-microbial Effect of Filtered 222 nm Excimer Lamps in a Hospital Waiting Area. J BioMed Sci Vol.10 No.S6:004.
Keywords
Hospital acquired infections; 222 nm excimer; Ultraviolet light; Respiratory infections; Immunocompromised state
Introduction
Hospital-Acquired Infections (HAI) is a major health problem on a global scale; it is estimated that 23.6% of hospital-treated sepsis cases are hospital acquired. In the USA alone, the applied cost for health care providers from HAI has been estimated to consist up to 14.9 billion USD and furthermore, HAI account for up to 37,000 annual deaths in Europe and 99,000 annual deaths in the USA (WHO).
The recent Sars-CoV-2 pandemic has highlighted our vulnerability toward spread of highly contagious infectious agents, and the importance of implementing and further developing techniques to prevent spread of contagions, especially in places where large numbers of persons pass by, or where particularly vulnerable persons gather. The clinic of pulmonology is an example of such a high-risk area. Here, numerous patients with respiratory diseases are crowed in a small area. Some patients visit the clinic to commence or followup treatment for infectious respiratory diseases such as complicated pneumonia, lung absces, fungal pneumonia, tuberculosis or bronchiectasis and wait near others patients who are on immunosuppressive therapy, have had lung transplantation or have severely reduced lung function. Thus, spreading infection from one patient to another may have dramatic consequences in this population. Use of anti- microbial measures such as frequent cleaning of rooms and furniture along with separation of patients and focus to reduce waiting time may lower risk for infections, but more efforts to modify the risk are needed and advanced techniques have evolved in recent years to supplement the effect of such measures.
Ultraviolet (UV) light is well-known to possess excellent disinfecting properties, by inducing the formation of pyrimidine dimers in RNA and DNA, thereby interfering with transcription and replication [1,2]. “Classical” 254 nm UV light has long been used in biological safety cabinets in laboratories. However, the fact that conventional 254 nm UV light is highly carcinogenic in humans limits its potential for anti-septic utilization in locations with high risk of person-to-person transmission of contagions [3]. Recently, a new generation of filtered excimer lamps based on excitation of Krypton Chloride (KrCl), generating 222 nm UVCLight, has been introduced. In contrast to UVC-Light at 254 nm, filtered 222 nm excimer lamps (UV222 TM lamps) can be safely installed in populated areas [4-11].
In order to test the anti- microbial potential of filtered 222 nm excimer lamps to reduce the risk of nosocomial spread of infections, we tested the effect of installing filtered filtered 222 nm excimer lamps in a out-patient clinic waiting room on bacterial load on exposed surfaces.
Materials and Methods
Aims, setting and study design
The primary aim of this study was to investigate the antimicrobial potential of filtered 222 nm excimer lamps in an outpatient hospital setting. A prospective longitudinal single arm interventional study with serial sampling was designed and set up in the waiting area at the out-patient clinic at the Department of Respiratory Diseases and Allergy, Aarhus University Hospital, Aarhus, Denmark.
Secondary aims were to evaluate how the filtered 222 nm excimer lamps affected bacterial load in the 222 nm exposed area compared to chairs placed in the more distant area of the waiting area and thus outside the range of the filtered 222 nm excimer lamps. Furthermore, we aimed to identify the bacteria load and determine which bacterial species were present on non-UV-exposed chairs compared to 222 nm-exposed chairs.
The waiting area
In the clinics waiting area patients awaits consultation or respiratory examinations. The clinic has services for patients with complicated infectious respiratory diseases, follows up after lung transplantation, severe asthma, interstitial pneumonias, and suspected lung cancer and is equipped with 10 chairs.
Filtered 222nm excimer lamp
The far-UVC source used in this study was a germicidal lamp (UV222TM, UVmedico, Denmark) based on a filtered KrCl* excimer light source emitting at 222 nm (Care222, Ushio, Japan). The optical filter blocked the remnants in the 230-350 nm emission range which are naturally present in KrCl* excimer lamps. At 222 nm the lamp had a total output of 120 mW, with a full-width half-max emission angle of 60 degrees, resulting in an irradiance of 13.7 μW/cm2 at 1 m distance. The output power, optical spectrum and spatial distribution of the lamp has been characterized using a UV calibrated goniometer (“LabSpion” from “Viso Systems”). Input information into the UV222TM software contained data on distance to nearest unprotected eye, maximum occupancy time per patient or staff, and Dose Delivered (DD) per on-off cycle in the farthest distance from the lamp. In this instance, dd for chair seats were 400 μJ, which is the approximate equivalence of the dose needed to reduce infectivity of SARS-CoV2 with approximately 90% [4,12].
Simulation of waiting room
For simulation and visualisation of the light distribution and energy levels on different surfaces in a room, the DiaLux EVO version 9.2 Light simulation software was used. The fixture files used in the program were verified and measured using the reference LabSpion system and goniometer from Viso Systems. To illustrate the setup and to calculate 222 nm doses, a 3Dmodel of the waiting area and the placement of the lamps was generated. Evaluation of the overall exposure intensity and the exact delivered energy in μW/cm2 on each section of the chairs was done using this model. Based on the energy values on the outer part of the two chairs positioned under one of the lamps (1,3-2,0 μW/cm2), we adjusted the filtered 222 nm excimer lamps to deliver a total of 400 μJ for each on-cycle. The rationale for this dosage is that many viruses including SARS-CoV2 are significantly inactivated at this dosage [12]. Infectious viruses are present mainly in aerosols in the air and thus closer to the lamp. As the intensity of the emitted light increases with increased proximity to the filtered 222 nm excimer lamps, viruses suspended in the air would then receive a sufficient 222 nm dose to significantly reduce the risk of transmission in one on-cycle [4,12]. The length of the off-cycle was adjusted so that patients were never exposed to more than 22.3 mJ in one visit, which is maximum daily exposure limit set by the Danish government and the European Union.
Bacterial load sampling
Bacterial loads were determined using Hygicult® TPC sampling kit (Adian) in accordance with the protocol supplied by the manufacturer. The agar-covered sampling sticks were used to collect samples from chair seats and backrests. For each seat or backrest sampling, two measurements were performed using the two sides of the hygicult sampling stick. The sampling sticks were then incubated overnight at 38°C before counting bacterial colonies.
Samples were collected at the same time in the afternoon on three consecutive days with the filtered 222 nm excimer lamps turned off and repeated for three consecutive days with the lamps turned on. As the same spots were sampled on each chair on three consecutive days, CFU counts of each day were assessed to see if variance in bacterial load was introduced.
Maldi-Tof MS identification of bacteria
Matrix-assisted Laser Desorption Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS), was used to determine which bacterial species were present on non-UV-exposed chairs compared to 222 nm-exposed chairs. Hygicult® TPC sampling sticks were randomly selected and analyzed.
Ethical concerns
Following local regulative informed patient consent was not required. No sensitive data was recorded. The filtered 222 nm excimer lamps lamp is commercially available (UV222TM) and approved by Conformité Euroéenne, the CE-mark, meeting European Union standards for health and safety. Conduction of the study was approved by the chief of department.
Statistical analysis
Paired students t-test was performed according to analysis of parametric data distribution. A student’s t-test test was done to evaluate change in bacterial load over the days of sampling. Statistical level of significance was set to 5%. Data were analysed in graph pad prism.
Results
Simulation of 222 nm exposure from filtered 222 nm UVC-lamps installed in the waiting area at Aarhus University Hospital
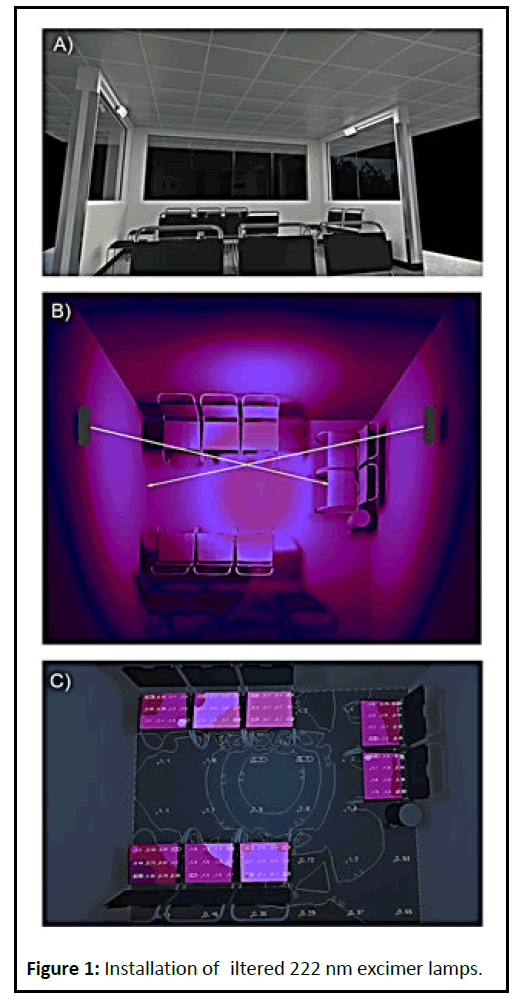
Using the simulation 3D-model of the waiting room the overall exposure intensity and the exact exposure on each chair was calculated and the filtered 222 nm excimer lamps were adjusted to deliver a total of 400 μJ for each on-cycle (Figure 1).
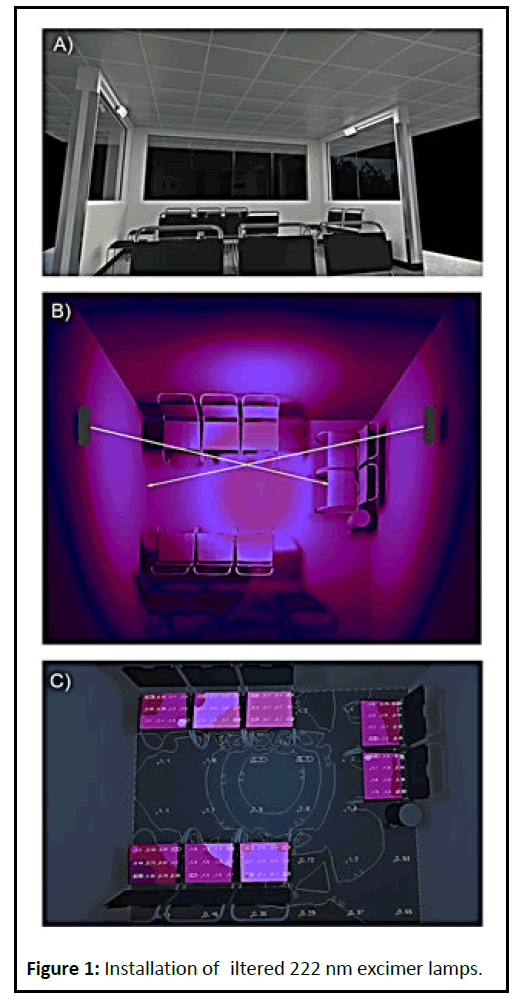
Figure 1: Installation of iltered 222 nm excimer lamps..
Effect of filtered 222 nm UVC-Light
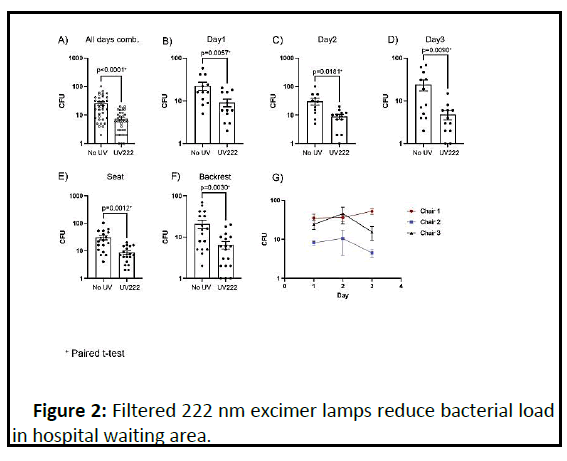
Regarding aim 1, we found that filtered 222 nm excimer lamps reduced the bacterial load of all chairs as the CFU count was significantly lowered from a mean of 26 CFU pr sample without exposure to 8 CFU pr sample with exposure (p<0.0001 by paired t-test). Interestingly, we found that the installation of the filtered 222 nm excimer lamps not only decreased the overall amount of CFU but also efficiently removed all high CFU counts (above 20 CFU per sample ). The decrease in CFU was consistent when comparing the sampling days. Additionally, exposure to 222 nm UVC-light was sufficient to decrease the CFU of both seat and backrest of all chairs indicating good coverage of the chairs with 222 nm UVC-Light exposure. Furthermore, we found no pattern of variance throughout the sampling period thus suggesting that the sampling itself did not affect CFU numbers (Figure 2)
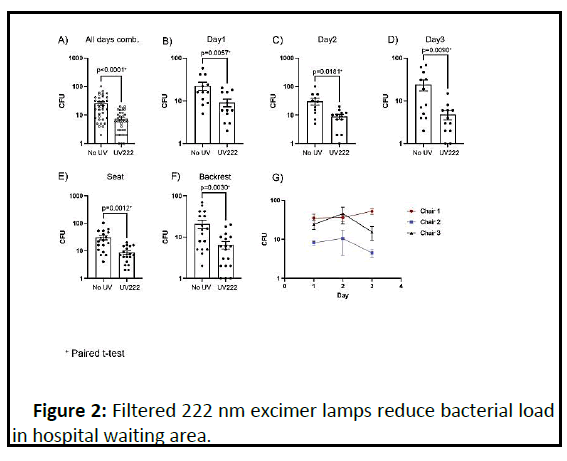
Figure 2: Filtered 222 nm excimer lamps reduce bacterial load in hospital waiting area..
Bacterial load outside the exposed area
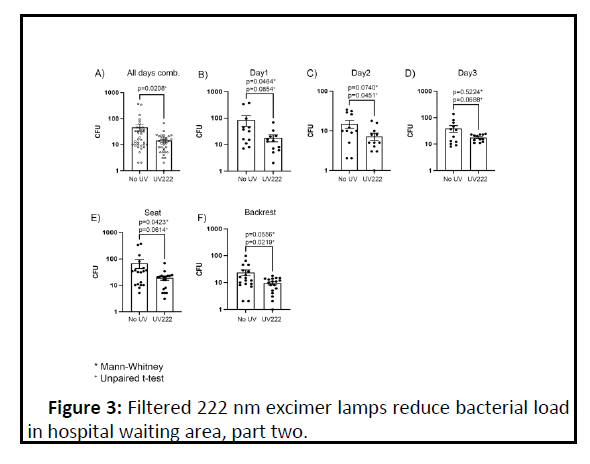
In aim 2, we found a decrease in the bacterial load within the zone exposed to 222 nm UVC-Light as compared to the chairs that were not exposed to the filtered 222 nm excimer lamps. The reduction in CFU was consistent during all three sampling days yet with some variation to the degree of bacterial removal. In accordance with results from the chairs that were exposed to the 222 nm UVC-light, we observed that CFU was reduced on both the seat and the backseat of all chairs during the days with lamps turned on (Figure 3)
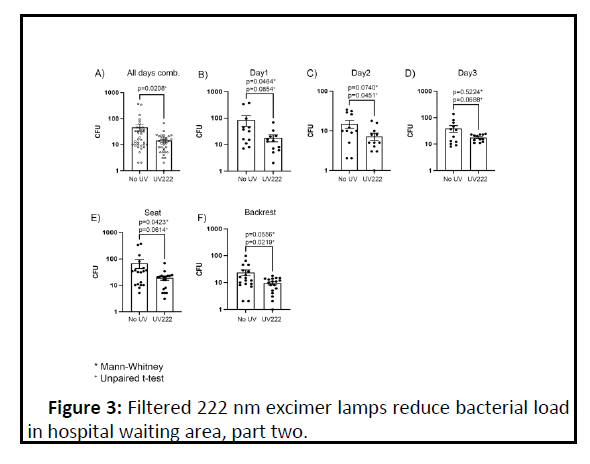
Figure 3: Filtered 222 nm excimer lamps reduce bacterial load in hospital waiting area, part two..
Identification of specific bacetrial species using MALDI-TOF
MALDI-TOF MS identified multiple bacterial species. On non- UV chairs 17 different species were identified of which 10 were unique to these chairs as they were not found on exposed chairs. Interestingly, only 10 different species were found on chairs exposed to filtered 222 nm UVC-Light, of which seven were seen on both non-UV and UV exposed chairs.
Discussion
This study aimed to evaluate the antimicrobial effect of filtered 222nm light and found that such exposure significantly reduces the overall bacterial load and seemed to eliminate a number of pathological bacterial species in a waiting area at a pulmonology out-patient clinic.
Conventional mercury UV light has long been known to have disinfecting capability but its carcinogenic potential limits use in areas populated with humans. Searches for a tolerable technique have led to the development of the excimer lamp that generates UV light at 222 nm, a wavelength safe to humans. Most studies published on the antimicrobial efficiency of UV at 222 nm has been performed in laboratory settings as proof of principle [12]. While results have been very positive with regards to human safety and in-vivo antimicrobial effect, this study is the first to show efficacy in a real-life setting and finds two interesting results.
Firstly, the ability of filtered 222 nm excimer lamps to significantly decrease the CFU of hospital waiting room chairs highlight the usability of these types of devices in the clinical setting. Of specific interest is the ability of filtered 222 nm excimer lamps to eliminate all higher CFU counts possibly stemming from patches of high bacterial density. It is reasonable to assume that these high-density patches potentiate a high-risk bacterial spread. Therefore, removal of all higher bacterial patches could potentially lower spread of bacteria from this surface. This would be of tremendous benefit as a pulmonology out-patient waiting room has a high flow of patients; some patients carry pathogenic and some patients carry antibiotic resistant bacteria and some patients are immunocompromised and may develop fatal illness if exposed to these bacterial patches.
Secondly, we show that filtered 222 nm excimer lamps remove highly pathogenic bacterial species. Of specific interest is the removal of Staphylococcus aureus as this bacterial species is known for its potential to develop antibiotic resistance [13]. As both Methicilin Resistant and Methicilin Sensitive Staphylococcus aureus (MSSA and MRSA respectively) represent an increasing problem in hospital environments and nosocomial infection with these species are common and lead to increases in duration of hospital admission [14]. Thus, removal of this species using filtered 222 nm excimer lamps could be of high value especially in departments treating patients with compromised immune systems who easily suffer from infections and in surgical departments. Also of interest is the apparent removal of Staphylococcus epidermidis, which is known to cause infection following insertion of catheters and in many resistant to therapy due to formation of biofilm. Reduction in biofilmforming bacteria could be of huge benefit, not only in the clinical world but also in multiple industries suffering from the generation of biofilm.
One limitation of this study is that bacterial samples were only taken from surfaces; no air sampling was done. In patients suffering from respiratory diseases, inhaled bacteria are of special interest; however, it is reasonable to assume that free flowing microbes also are eliminated by 222 nm UVC-Light.
Aerosolized particles are exposed from all sides and are more easily eliminated than surface fixed bacteria and are also in closer proximity to the lamps that receiving a larger dose of 222 nm light. A theoretic risk of exposure could be that elimination of some bacteria allows other species to develop, and if these are pathogenic, the filtered 222 nm excimer lamps would potentially create a more dangerous milieu. However, results from the MALDI-ToF reject this concern. Importantly, the primary study objective was to reduce bacterial load in a clinical setting. A significant reduction was achieved but whether this results in to fewer infections in the patients is yet to be studied.
Finally, following the SARS-CoV-2 pandemic, it has become evident there is a need for better and more efficient disinfection techniques in areas with high density of people. Especially, techniques targeting not only viral pathogens such as SARSCoV- 2 but all disease-causing microorganisms are highly sought after. We did not include SARS-CoV-2 in our study as we expected very low, if any, of this virus in the out-clinic setting as all patients were tested negative before visits. However, viruses, including SARS-CoV-2 are more easily eliminated by 222 nm UVC-Light than bacteria and is therefore reasonable to assume that filtered 222 nm excimer lamps would inactivate these viruses in this setting as well [12]. A limitation to 222 nm UVCLight technology is that it only asserts its effect to surfaces that are exposed. Although UVC-Light is reflected and thus will reach most surfaces, those surfaces that are only indirectly exposed are likely to require much longer exposure time to experience significant reductions in bacterial load.
Conclusion
In conclusion, this study shows the usability of filtered 222 nm excimer lamps in a clinical setting. These devices, being safe for use in areas occupied by humans, have a high potential to become the disinfecting technology of the future as they can generate a continuous anti-microbial environment in areas with high density and high flow-through of people.
Acknowledgements
We would like to acknowledge UV medico (Aarhus Denmark, UVmedico.com) for supplying filtered 222 nm excimer lamps (UV222TM) and Christian Byriel for simulation of 222 nm exposures in the hospital waiting area.
Conflicts of Interest
Christian Kanstrup Holm is co-owner and Jacob Thyrsted is part-time employed at UV medico, which is a manufacturer of UV222TM nm lamps.
41916
References
- Goosen N, Moolenaar GF (2008) Repair of UV damage in bacteria. DNA Repair (Amst) 7:353-379.
- Cutler T, Wang C, Qin Q, Zhou F, Warren K, et al. Kinetics of UV(254) inactivation of selected viral pathogens in a static system. J Appl Microbiol 111:389-395.
- Anna B, Blazej Z, Jacqueline G, Andrew CJ (2007) Mechanism of UV-related carcinogenesis and its contribution to nevi/melanoma. Expert Rev Dermatol 2:451-469.
- Buonanno M, Welch D, Shuryak I, Brenner DJ (2020) Far-UVC light (222 nm) efficiently and safely inactivates airborne human coronaviruses. Sci Rep 10:1-9.
- Welch D, Grilj V, Shuryak I, Buonanno M, Crickmore C, et al. (2018) Far-UVC light: A new tool to control the spread of airborne-mediated microbial diseases. Sci Rep 8:1-8.
- Buonanno M, Ponnaiya B, Welch D, Stanislauskas M, Pehrson GR, et al. Germicidal Efficacy and Mammalian Skin Safety of 222-nm UV Light. Radiat Res 187:483-491.
- Cadet J (2020) Harmless Effects of Sterilizing 222-nm far-UV Radiation on Mouse Skin and Eye Tissues. Photochem Photobiol 96:949-950.
- Eadie E, 'Mahoney OP, Finlayson L, Barnard I, Wood K, et al. (2021) Computer Modeling Indicates Dramatically Less DNA Damage from Far-UVC Krypton Chloride Lamps (222 nm) than from Sunlight Exposure. Photochem Photobiol 97:1-5.
- Barnard IRM, Eadie E, Wood K (2020) Further evidence that far-UVC for disinfection is unlikely to cause erythema or pre-mutagenic DNA lesions in skin. Photodermatol Photoimmunol Photomed 36:476-477.
- Yamano N, Kunisada M, Sugihara k, Kaidzu S, Nishiaki-Sawada A, et al. (2020) Long-term Effects of 222-nm ultraviolet radiation C Sterilizing Lamps on Mice Susceptible to Ultraviolet Radiation. Photochem Photobiol 96:853-862.
- Narita K, Asano K, Morimoto Y, Igarashi T, Nakane A (2018) Chronic irradiation with 222-nm UVC light induces neither DNA damage nor epidermal lesions in mouse skin, even at high doses. PLoS One 13:1-8.
- Hessling M, Haag R, Sieber N, Vatter P (2021) The impact of far-UVC radiation (200-230 nm) on pathogens, cells, skin, and eyes - a collection and analysis of a hundred years of data. GMS Hyg Infect Control 16:1-5.
- Lencastre H, Oliveira D, Tomasz A (2007) Antibiotic resistant Staphylococcus aureus: A paradigm of adaptive power. Curr Opin Microbiol 10:428-435.
- Cowie SE, Ma I, Lee SK, Smith RM, Hsiang YN (2005) Nosocomial MRSA infection in vascular surgery patients: IMPAct on patient outcome. Vasc Endovascular Surg 39:327-334.