Keywords
Anxiety; Depression; Quality of live; Adult; Sickle cell disease
Introduction
Sickle cell disease is a recessive hereditary disease due to a point mutation of a gene that codes for the synthesis of the β chain of hemoglobin. This leads to anemia, multi organ failure, increased susceptibility to infections, acute and chronic pain. It is frequent in Africa. The prevalence of the sickle cell trait in the Central African region is estimated to be between 20-30% and the disease attacks about 2% of the Cameroonian population (about 400 000 patients) [1].
Anxiety and depressive disorders are severe pathologies that can lead to great sufferings, altered professional school and family lives and thus favors a bad quality of life [2]. According to the World Health Organization (WHO), depression is the most disabling pathology in terms of the number of years of global disability [2]. According to a cohort study with 2981 patients carried out by Heer et al. in Holland, patients with anxiety and depressive disorders had severe disabling chronic pains as opposed to patients without these disorders [3]. In the study by Levenson et al, out of the 266 sickle cell patients in the United States of America, 27.6% of the patients had depressive disorders and 6.5% had anxiety disorders.
In the Cameroonian setting, few studies have been carried out to assess depression, anxiety and quality of life and other associated factors in sickle cell patients. This is also true for sub- Saharan Africa. Thus our objectives were to determine the prevalence and factors linked to anxiety, depression and quality of life of sickle cell patients.
Materials and Methods
We carried out a cross-sectional descriptive and analytic study for 4 months (February 2015 to May 2015). The study site was the Yaounde Central Hospital and sampling was non probabilistic.
Patients
Were included in this study:
- Sickle cell patients aged 19 years and above
- Patients who gave their informed consent
Were excluded from this study:
- Sickle cell patients who had a hemoglobin electrophoresis of AS or whose Hemoglobin electrophoresis was uncertain.
- Sickle cell patients currently admitted in hospital.
- Patients on antidepressants, anxiolytics or patients taking any other antipsychotic medication
- Patients who could not communicate in the official Cameroonian languages (English or French)
Data were collected on data entry forms that were tested on 10 patients. The data entry forms were administered to patients in a face to face interview in a room with just one investigator. After making sure that the patients fulfilled all the inclusion criteria and had none of the exclusion criteria, the patients were interrogated. During the interviews we collected socio- demographic information, clinical information and we measured depression, anxiety and quality of life.
The following socio-demographic data were collected: age, sex, residency (rural/urban), level of education, matrimonial status, number of children, professional status, religion, alcohol consumption, satisfaction with social support, past history of psychiatric disorders in family, the presence of past history of sickle cell disease in the family.
The clinical data collected were: the use of nonconventional medication, the presence of another medical pathology, the presence of complications linked to sickle cell, the number of hospitalizations in last 12 months, the number of blood transfusions in last 12 months, the duration of the last painful crises, the number of times admitted in an emergency hospital service in the last 12 months, currently taking medication that contains hydroxyurea.
Screening of anxiety
Anxiety was investigated with the aid of the General Anxiety Disorders (GAD-7). This questionnaire has been validated and was based on the revised version of the 4th edition of the Diagnostic and statistics manual of mental disorders of the American Society of Psychiatric. The score varies from 0 to 21. Scores of 6 to 10, 11 to 14, 15 to 21 highlights the presence of mild anxiety, moderate and severe anxiety respectively. A score greater than 10 strongly favors a moderate to severe anxiety with a sensitivity of 89% and a specificity of 82%.
Screening of depression
We used the Patient Health Questionnaire (PHQ-9) to screen for symptoms linked to depression. This questionnaire has been validated and was based on the revised version of the 4th edition of the Diagnostic and statistics manual of mental disorders of the American Society of Psychiatric. The score varies from 0 to 27. A score greater than 9 has a sensitivity of 83% and a specificity of 92% for the diagnosis of depression.
In this study the diagnosis of depression was made when the score was ≥ 10. Scores between 10 and 14 represented mild depression, scores 15-19 represented moderate depression and scores greater or equal to 20 represented severe depression. For this study we used the version validated in French.
Evaluation of quality of life
In order to measure the quality of life (QOL), we used the Medical Outcomes Study Short-Form (SF12v2). Considering the recommendations, the scores varied from 0 to 100 with high scores representing a dysfunction, a depreciation or pain. The scores were then transformed to standard deviations and patients with a score less than 50 were considered having an altered quality of mental or physical health. This scale was validated in a population of patients living with HIV in Cameroon in a study carried out by ANRS 12-116.
The data collected were typed, codified and analyzed with the Statistical Package for Social Sciences version 21.1.0 for windows (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Continuous variables were expressed as means (standard deviations) or medians (interquartiles). Categorical variables were expressed as frequencies (n) and proportions (%).
The proportions of anxiety and depression were expressed with the 95% confidence interval using the Fisher Exact test and considering the sensitivity and specificity of scales used. This confidence interval was calculated with the software Windows Program for Epidemiologists (WinPepi) version 11.25.
The student T test was used to compare the means of quality of life between anxious and non-anxious patients and between depressive and non-depressive patients.
To analyze the factors associated to depression, anxiety and bad quality of life, we used the multivariable binary logistic regression statistical analysis. The logistic regression was used by integrating in the model all variables with a p value ≤ 0.20 in the univariate analysis. The null hypothesis was rejected for all values of p<0.05 and for all odds ratio (OR) for which the 95% confidence interval did not include 1.0.
The Pearson correlation was used for the correlation between the degree of anxiety, of depression and the score of the quality of life.
Some explorative analyses were done to measure the reliability and the possibility of using factorial analysis of the scales used. A precision of the sampling by Kaiser-Meyer- Olkin>0.50 and the test of sphericity of Barlett<0.05 indicated a possibility for a factorial analysis to be performed. An alpha of Cronbach>0.5 indicating a good reliability of scales in the studied population.
Results
The mean age was 28.2 years (SD 8.5). The proportion of males and females was equal and was 50%. The most represented level of education was the secondary school level and represented 44.9% (n=35), next was the university level representing 42.3% (n=33), then the primary level with 11.5% and 1.3% had no formal level of education. University students and secondary school students were the most represented with 44.9% (n=35). Out of the 78 patients 68 (87.2%) were single and 10 (12.8%) were married. Twenty one (26.9%) of the patients had children. Seventy two (92.3%) were Christians and 6 (7.7%) were Muslims. Fifty nine (75.6%) patients were satisfied with their social support, 7 (9.0%) had a past history of psychiatric disorders and 23 (29.5%) had a past history of parents with clinical signs linked to sickle cell disease. Four (5.1%) patients drank alcoholic drinks and 2 (2.6%) consumed tobacco. The proportion of patients who used traditional medicines was 17.9% (n=14). In this study 15.4% (n=12) of patients had an associated medical disease: HIV (n=1), gastro-duodenal ulcers (n=4), sinusitis (n=2), gout (n=1), heart diseases (n=1), arthrosis (n=3). In this study 23.1% (n=18) of the patients had a complication due to sickle cell disease and the most represented complication was osteonecrosis (n=7.41.2%). The mean hospitalization within the last 12 months was 1.2 (SD 1.8). The median was 1(interquartile: 0 to 1). Twenty eight patients (35.9%) were not admitted within the last 12 months. The mean admission at emergency medical services within the last 12 months was 0.7 (SD 1.1). The median was 0 (interquartile: 0 to 1). Forty three patients (55.1%) did not have any admissions in an emergency medical service within the last 12 months. The number of painful crises within the last 12 months was 3.2 (SD 3.8). The median was 2 (interquartile 1 to 5). Eighteen patients (23.1%) did not have any painful crises within the last 12 months. The mean period between the last painful crises and data collection was 12.9 months (SD 26.9). The median was 30 months (interquartile 7 to 270). The mean number of blood transfusion within the last 12 months was 0.6 (SD 1.3). Fifty nine patients (75.6%) did not have any blood transfusion within the last 12 months. Two patients (2.6%) took medication containing hydroxyurea. No patient took medication containing antidepressants or anxiolytics.
The mean score with the PHQ-9 scale was 7.3 (SD 4.7) with 0 and 24 as minimum and maximum respectively. The median score was 7 (interquartile 3 to 10). Twenty three patients (29.5%, 95%CI 19.7 to 40.8) were depressed. Mild depression was the most represented category of depression (21.8%). More to that 12.8% (10 patients had suicidal ideas). The factors linked to mental depression were: unsatisfactory social support, the presence of current complications linked to sickle cell disease, hospitalization within the last 12 months, the number of painful crises within the last 12 months.
The mean score with the GAD- scale was 5.0 (SD 4.2) with 0 and 21 being the minimum and maximum scores respectively. The median score was 4 (interquartile 2-7). Eleven (14.1%) patients were anxious. The level of anxiety the most represented was moderate anxiety (9.0%). The factors associated to anxiety were: unsatisfactory social support, the presence of a complication linked to sickle cell disease, being hospitalized within the last 12 months, admission into an emergency medical service within the last 12 months, and having a Vaso-Occlusive Crises (VOC) within the last 12 months. The factors not directly linked to anxiety were: being single, unsatisfactory social support, the presence of complications linked to sickle cell disease and having children.
The mean score of quality of physical life was 42.0 (SD 9.0) with 19.9 and 57.9 being the minimum and maximum scores respectively. The median score was 42.8 (interquartile 35.3-49.3). Sixty-one (78.2%) patients had a bad quality of physical life. The mean score of the mental quality of life was 45.7 (SD 11.4) with 15.5 and 69.8 as minimum and maximum respectively. The median score was 46.1 (interquartile 38.8 to 53.8). Fifty (64.1%) patients had a bad quality of mental life. The factors linked to a poor quality of physical life were: the number of admissions in an emergency service within the last 12 months and having at least one child.
The factors not directly linked to a poor quality of physical life were: the number of admissions in an emergency service within the last 12 months and increasing age. The factors associated with a bad quality of mental life were: family history of sickle cell disease, unsatisfactory social support, having a complication linked to sickle cell disease, being hospitalized within the last 12 months. The factors independently associated to a bad quality of mental life were: unsatisfactory social support, having a complication linked to sickle cell disease, being hospitalized and received a blood transfusion within the last 12 months, had VOC within the last month and being single.
We found out that there was a statistically significant linear association between the GAD-7 scale and the PHQ-9 scale and a negative statistically significant association between the scale MOS SF 12v2 and GAD-7, between the MOS SF12v2 and the PHQ-9 scale (Table 1).
| |
GAD-7 |
PHQ-9 |
MOS SF12v2 Physical |
| PHQ-9 |
0.73 (<0.001) |
- |
- |
| MOS SF12v2 Physical |
-0.07 (0.547) |
0.01 (0.920) |
- |
| MOS SF12v2 Mental |
-0.61 (<0.001) |
-0.68 (<0.001) |
-0.20 (0.086) |
Table 1: Pearson correlation coefficient (p-value) between the medical outcome study short form 12 version 2, GAD-7 scale and PHQ-9 scale.
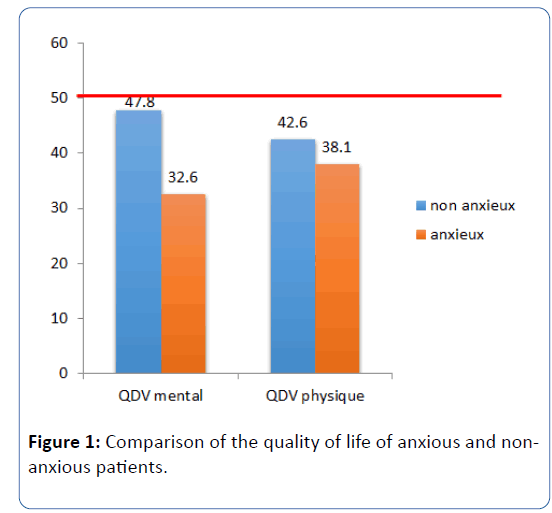
The mean quality of mental life of the anxious and nonanxious patients were different and this difference was statistically significant, P<0.0001; 15, 18 (3,3) 95%CI (8.6 to 21.7).
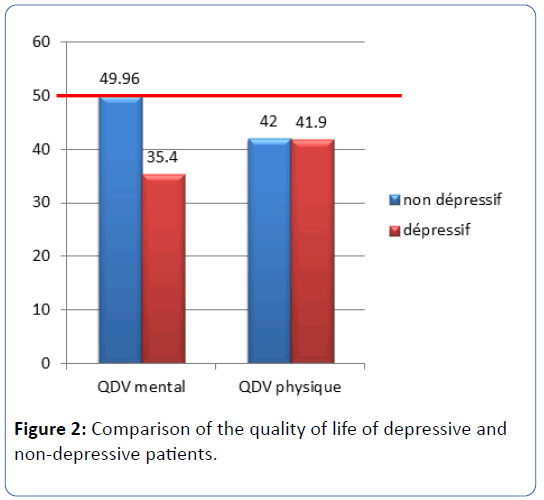
The mean quality of mental life of depressed and nondepressed patients was different and this difference was statistically significant, P<0.0001; 14, 5 (2,3), 95% CI (9,9 to 19,12).
Discussion
The mean age of 28.2 years (SD 8.5) that we obtained is different from that of other studies but very close to the mean of those studies. Dampier et al. in 2011 in a cross sectional study of 1046 patients on complications of sickle cell disease in adults followed up in the United States “Health-Related Quality of Life in Adults with Sickle Cell Disease (SCD): A Report from the Comprehensive Sickle Cell Centers Clinical Trial Consortium” found a mean of 31.4 (SD11.8) years [4].
Levenson et al. in 2008 in a study on anxiety and depression with 266 patients suffering from sickle cell disease in the United States found a mean age of 34 years [5]. Asnani et al. in a study carried out in 2010 on 277 patients in Jamaica looked for depression and loneliness in homozygote sickle cell patients and found a mean age of 31 years [6].
Anie et al. in a study of 510 patients followed up in Algeria on the auto evaluation of pain, mood and quality of life found a mean of 28.9 (SD 10.2) [7]. This can be explained either by the adequate management of patients since enrolment of participants was in a sickle cell health management unit or by a natural selection of patients with less severe disease [7].
The sex ratio was 1, similar to what different studies reported. Dampier et al. had 52% women and 48% men in their study [4]; Levenson et al. got 41.7% men and 58.3% women [5]; Anie et al. in 2012 got 39% men and 69% women and 1% did not register their sex [7]. This could be explained by the fact that sickle cell disease is an autosomal disease and affects as more men as women.
Nevertheless these studies show a net increase of female sex since more females do consult in hospital. Eighty seven (87.2%) of the patients had a level of education beyond secondary school. This finding is similar to what Santos et al. [8], Asnani et al. [6], Levenson et al. [5] who respectively had 71.9% , 82.7% , 86.5%. It was Superior to those of Vilela et al. [9] who found only 36% in a study of 35 patients with 15 adolescents. The high figures we obtained can be explained by the fact that the study site- Yaounde is a University area thus populated with University students. More to that the education of sickle cell patients is more effective and the management of these patients is better since their parents are well informed. The professional status of the patients was difficult to discuss with existing literature for in literature there is no distinction between school patients and patients seeking employment. 30.8% of patients were employed and this represented more than half of the patients thus these were not students. Belgrave et al. in 1991 [10] found a figure close to our value,32% of the patients in their study had employment same like Dos Santos et al. got 31.2% of employed patients. In the study by Vilela et al. [9], 88% of patients were employed; just 25 patients were enrolled probably because just employed patients could be managed at their health facility; for Hasan et al. in 2003 they found that 18% of patients were employed [11]. Just 12.8% of patients were married and 87.2% of them were single. These results were similar to those obtained by Asnani et al. [6] which found 9.7% of married patients. Hasan et al. [11] found that 13% of patients were married. Belgrave et al. [10] found that 17% of the patients were married. Dos Santos [8] found 21.9% of patients were married. Levenson et al. [5] found that 23.2% of patients were married. These results were low despite the fact that 45% of patients were students or university students; but not having results in terms of the general population we cannot attribute this low value to sickle cell disease. 26.0% of patients had at least one child, none of them wanted their child to have sickle cell disease for having a child leads to financial constraints thus could be a factor for anxiety and depression. 92.3% of patients were Christians and 7.7% were Muslims, this predominance could be attributed to the fact that Yaounde was the study site and mostly made of Christians. 75.6% of patients were satisfied with their social support for social support is an important element for wellbeing and patients not being satisfied are an important element for depression, anxiety and a poor quality of life [12].
All patients ought to be satisfied with social support be it financial or emotional. Just 9% of patients had a family history of psychiatric disorders and the prevalence of psychiatric disorders was not known. We found that 29.5% of patient’s hand a past history of sickle cell disease in the family, this finding is close to 25%; the probability of having a brother or a sister with sickle cell disease if we have sickle cell disease. Four (5.1%) of patients regularly consumed alcohol, this can be explained by the fact that patients are aware of the fact that alcohol consumption is a risk factor for dehydration thus favoring VOC. Two (2.6%) patients smoked tobacco and this figure explains the fact that patients also know that tobacco can lead to long term lung diseases that will favor hypoxia and thus falciformed red blood cells. Fourteen (17.9%) patients used traditional medication while others used medications whose innocuousness is unknown. Such medications could worsen sickle cell disease in the long term [13-15].
Patient counseling and clinical studies done under ideal settings should be performed for such medications. Eighteen (23.1%) patients had current complications linked to sickle cell disease, that presence of another disease could be linked to anxiety and depressive symptoms. Amongst these complications no patient complained of a renal, pulmonary or heart disease except those often seen in sicklers [16]. This raises the problem of diagnosis of these complications and of all other complications of sickle cell disease. 64.1% of patients were admitted at least once during last 12 months, this reflects the gravity of the disease. The average VOC of patients was 3.2 (SD 3.8) and the median was 2, so 50% of patients had at least 2 crises within the last 12 months. This result is alarming because the mortality increases with the number of crises [17] and the mean in our study is 3 crises/year. Only 2 (2.6%) patients were taking hydroxyurea, a medication that is given to patients with severe complications. The severity in our study can be categorized as mild to moderate.
The prevalence of mental depression was 29.5% (95%CI=19.7-40.8) and the patients presented depressive symptoms (PHQ 9 ≥ 10), this result is close to that of James et al. who found in 2005 that out of 232 patients in the United States used a data entry form similar to the one we used got 27.6% depressive patients [5]. A study done in Congo-Brazzaville made of children aged 8 to 17 found a high prevalence (86.4%) of depression by using the Multiscore Depression Inventory for Children [14]. In this study we notice that the population included mostly children and adolescents thus less likely to have the pathologies associated to sickle cell disease and more subject to VOC which could lead to anxious symptoms. A stud carried out in Jamaica found a prevalence of 22% in sickle cell patients with mean age 31 years [6].
Factors independently associated to depression were: unsatisfactory social support, the presence of a complication linked to sickle cell disease, the number of transfusions within the last 12 months, a period less than 30 days since the last crises, age. Few studies looked for factors associated to depression in sickle cell patients. Hasan et al. in the United States in 2003 in a cross sectional study of 49 patients (homozygote sicklers) depression in sickle cell disease» found the following factors associated to depression: increase in blood transfusions, low level of control of pain, medication with hydroxyurea, low income, female sex, low level of education, these last 4 factors were not found [11].
Levenson et al. found that increasing age and a low income were associated to symptoms linked to depression [5]. Contrary to the study by Leverson et al. in the United States it is at a very young age that patients are at risk of depression. This difference could be due to the fact that life expectancy could be high in this context.
The presence of current complications linked to sickle cell disease, the admission within the last 12 months and admissions in an emergency service within the last 12 months for a period less than 30 days since the last painful crises and blood transfusion within the last 12 months, these clinical signs show the importance of controlling the sickle cell disease in patients so as to avoid depression. Being admitted in hospital once within the last 12 months was a factor associated to the unset of depression. One chronologic study between the relation of hospitalization and the unset of depressive symptoms should be carried out to have an idea on the relationship between this factor and mental depression. Nonetheless hospitalized patients can have an inflammatory pathology and the inflammation is associated with secretion of interleukins that provoke depressive symptoms. More to that the presence of depression reduces the thresh hold of pain perception and could lead patients to consult for mild pains.
The number of crises within the last 12 months was also a factor associated with depression. The pain in sickle cell patients can have a mechanic component and an inflammatory component that can lead to depression. Again mental depression can lead to vaso occlusive crises and the increase in the sensitivity to mild pain which could be considered by patients as crises. In order to know whether vaso-occlusive crises are the cause or consequence of depression in sickle cell patients, case control or cohort studies should be carried out. Satisfaction with respect to social support was found as an independent factor associated to the unset of depression. Patients who declared to be unsatisfied with their social support could have financial problems that led to stress thus causing depressive symptoms. Again mental depression has as symptoms increased relational issues, the patient accuses his surroundings to be the cause of their state and try to be isolated thus leading to social unsatisfaction.
Having a current complication linked to sickle cell disease was also a factor independent and not associated to the unset of depression. These complications could also be the cause of depression since these complications are chronic pathologies: leg ulcers, osteonecrosis, cerebrovascular accidents and eye pathologies. Mental depression is a pathology that leads to immune-depression and thus can lead to leg ulcers or septic osteonecrosis. Mental depression is also frequent in patients who have had cerebrovascular accidents and is associated with a poor prognosis. Having at least one transfusion within the last 12 months was also seen as a factor independent to unset of mental depression; blood transfusion is not a consequence of mental depression. It could be a cause of mental depression probably through its origin, vaso occlusive crises or infectious pathologies that reduce the hemoglobin level to a level that necessitates a blood transfusion. Patients on transfusion might have more severe manifestation of sickle cell disease and are more likely to have mental depression. Having had a vasoocclusive crisis within the last 30 days was associated in an independent manner to the unset of depression. We do not know if mental depression was present before or after the unset of the VOC, but the VOC is a pain that has inflammatory characteristics and mechanical characteristics thus leading to depressive symptoms; more to that depression can lead to a VOC due to the secretion of substances that can favor the unset of an infection or a CVO. A cohort study should be carried out to assess the sequence of exposition to VOC-disease: unset of mental depression.
In our study the mean score of quality of physical life was 42.0 (SD 9.0) and the mean score of quality of mental life was 45.7 (DS 11.4). These results are similar to those found by Dampier et al. in which 1046 patients in the United States in 2009 [4] had a score QDV Physical of 39.6 (DS 10) and a score of QDV mental of 45.6 (DS 11.9); it was the same for the 8 other scales. These results show that despite the difference of socioeconomic status and quality of medical offers, patients in our study were able to support the disease and had scores of quality of life that were similar.
Factors that were independently associated to a bad quality of physical life were: the number of admissions in an emergency service within the last 12 months, age. The fact of having a child was a factor that is not dependently associated to a bad quality of physical life. Dampier et al. in 2011 in a cross Sectional study of 1046 patients on sickle cell complications in adult sicklers in the United States also found similar results [4].
This could be due to the fact that chronic complications are becoming the more and more frequent with age and worsens the prognosis of patients. The admission into the emergency service could be a sign of gravity and could be frequent in patients with bad physical state.
The factors independently associated to a bad quality of mental life were: unsatisfactory social support, having a complication linked to sickle cell disease (leg ulcer, septic osteonecrosis, VOC), being hospitalized within the last 12 months, had a VOC the month before enrolment, had at least a blood transfusion within the last 12 months, family history of sickle cell disease and being single. The presence of current complications linked to sickle cell disease, had at least one hospitalization within the last 12 months, had a VOC within the last month prior to enrolment, had at least one blood transfusion within the last 12 months were found as factors independently associated to a bad quality of mental health. These findings can be explained by the fact that patients with these factors have a more severe disease and this can contribute to the modification of the psychologic status of the patient thus leading to bad mental health. Lack of satisfaction with respect to social support being a factor independently associated to depression and anxiety might contribute to a bad quality of mental health of patients who want to modify their social and family relations. Single patients could have a social support that could be less than patients with partners and this would affect their mental health, the life of relationships with others and leading to a bad quality of mental health. More to that we found a negative correlation between the degree of anxiety and the score of quality of mental life through the bias of anxiety disorders where single patients could have an alteration in their quality of life. Patients with a family history of sickle cell disease had a higher risk (not dependent on other factors) of presenting a bad quality of mental health, the fact of having a brother or a sister who is sick or dead could be a bias of anxiety affecting the QDV of patients.
These results led us to notice that the degree of anxiety and the degree of depression are inversely proportional to the degree of quality of mental life and the degree of anxiety was proportional to the degree of mental depression. Even though this was not part of the objectives we had these results in addition to the coherence that has been found brings some new elements to validate the data entry forms we used. The quality of mental life of anxious and or depressive patients was inferior to those of patients who are not anxious and non-depressive (Figures 1 and 2). These results were found in other studies [15,16] and shows the sensitivity of MOS SF 12v2 that differentiates anxious and or depressive patients from nonanxious and or non-depressive patients and this scale could be used in clinical studies in our context so as to evaluate QDV.
Figure 1: Comparison of the quality of life of anxious and nonanxious patients.
Figure 2: Comparison of the quality of life of depressive and non-depressive patients.
Conclusion
The prevalence of mental disorders and depressive disorders was high. The quality of physical life and mental life were bad. The factors independently associated to anxiety were: singleness, unsatisfactory social support, the presence of complications linked to sickle cell disease and having children. The factors independently associated to depression were unsatisfactory social support, the presence of complications linked to sickle cell disease, the number of transfusions received within last 12 months, the presence of a VOC within the last 30 days and young age. Factors that were independently associated to a bad quality of physical life were the number of admissions in an emergency service within the last 12 months and increasing age. Factors that were independently associated to a bad quality of mental life were unsatisfactory social support, having a complication linked to sickle cell disease, having been hospitalized and transfused with the last 12 months and having a VOC within the last 30 days, being single. Depression and anxiety correlated and both correlate to the quality of mental life.
21993
References
- Regional Committee for Africa (2006) The drepanocytose in the african region: Current situation and outlook. World Health Organisatiion: 1-9.
- De Heer EW, Gerrits MMJG, Beekman ATF, Dekker J, van Marwijk HWJ, et al. (2014) The association of depression and anxiety with pain: a study from NESDA. PloS One 9: e106907.
- Dampier C, LeBeau P, Rhee S, Lieff S, Kesler K, et al. (2011) Health-related quality of life in adults with sickle cell disease (SCD): A report from the comprehensive sickle cell centers clinical trial consortium. Am J Hematol 86: 203-205.
- Levenson JL, McClish DK, Dahman BA, Bovbjerg VE, de A Citero V, Penberthy LT, et al. (2008) Depression and anxiety in adults with sickle cell disease: The PiSCES project. Psychosom Med 70: 192-196.
- Asnani MR, Fraser R, Lewis NA, Reid ME (2010) depression and loneliness in jamaicans with sickle cell disease. BMC Psychiatry 10: 40.
- Anie KA, Grocott H, White L, Dzingina M, Rogers G (2012) Patient self-assessment of hospital pain, mood and health-related quality of life in adults with sickle cell disease. BMJ Open 2: e001274.
- Dos Santos JP, Gomes Neto M (2013) Sociodemographic aspects and quality of life of patients with sickle cell anemia. Rev Bras Hematol E Hemoter 35: 242-245.
- Vilela RQB, Cavalcante JC, Cavalcante BF, Araújo DL, Lôbo M de M et al.(2012) Quality of life of individuals with sickle cell disease followed at referral centers in Alagoas, Brazil. Rev Bras Hematol E Hemoter 34: 442-446.
- Belgrave FZ, Molock SD (1991) The role of depression in hospital admissions and emergency treatment of patients with sickle cell disease. J Natl Med Assoc 83: 777-781.
- Hasan SP, Hashmi S, Alhassen M, Lawson W, Castro O (2003) Depression in sickle cell disease. J Natl Med Assoc 95: 533-537.
- U.S. Department of Health And Human Services (2000) Measuring healthy days. Center Dis Control Prevent: 44.
- Adegoke SA, Abioye-Kuteyi EA, Orji EO (2014) The rate and cost of hospitalization in children with sickle cell anaemia and its implications in a developing economy. Afr Health Sci
- Lukoo RN, Ngiyulu RM, Mananga GL, Gini-Ehungu J-L, Ekulu PM, et al. (2015) Depression in children suffering from sickle cell anemia. J Pediatr Hematol Oncol 37: 20-24.
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B (2007) Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann Intern Med 146: 317-325.
- Kocalevent RD, Hinz A, Brahler E (2013) Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 35: 551-555.
- Lionnet F, Stankovic K, Girot R (2009) Sickle cell disease of the adult. EMC- Hematology 4: 1-19.