Muhammad Wasif Haq1, Farzeen Tanwir2*, Madiha Nawaz3, SabaTabassum4, Muhammad Jabar5
1Student of Masters of Speech Pathology, Flinders University, Adelaide, Australia
2Post doctorate, PhD, MPhil (KI,Sweden),C.Orth(USA), BDS, Director of Post graduate Studies and Research, Associate Professor and HOD, Department of Periodontology, Ziauddin University, Pakistan
3Private Medical Practice, Islamabad, Pakistan
4House Officer, Hamdard College of Medicine & Dentistry, Karachi, Pakistan
5Data Analyst at University of Lahore, Lahore, Pakistan
- Corresponding Author:
- Farzeen Tanwir
Post doctorate, PhD, MPhil (KI,Sweden),C. Orth(USA)
Director of Post graduate Studies and Research
Associate Professor and HOD, Department of Periodontology
Ziauddin University, Pakistan
E-mail: Farzeen_tanwir@yahoo.com
Citation: Wasif Haq M, Tanwir F, Nawaz M, et al. Association of Systemic Diseases on Tooth Loss and Oral Health. J Biomedical Sci. 2015, 4:1. doi:10.4172/2254-609X.10001
Copyright: © 2015 Wasif Haq M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Key words
DMFT, DMFS, Tooth loss, systemic diseases
Introduction
Pakistan ranks as sixth most populous country of the world yet only 2.6% of total gross domestic product is allocated for public health. Approximately 70% of the population is resident in rural areas making the access to healthcare facilities difficult as most of tertiary care hospitals are located in the urban cities. The doctor to patient ratio is 1: 1254 while dentist to patient ratio is 1: 6557 reflecting a dearth of health care facilities in the country.
There is high prevalence of systemic diseases in the population. One in every four middle aged adult carries risk of coronary artery disease [1]. Pakistan is ranked as fifth and sixth country world over to be affected by pulmonary infections such as tuberculosis and diabetes mellitus (10% diabetes prevalence) [2,3]. Hepatitis B and C infections affect 9-10 Million people [4,5]. At 45 years, every third person is reported to be hypertensive (33% prevalence) while more than 50% of hypertensive often remains undiagnosed [6]. Likewise the rate of cerebral stroke is 4.8 % which is said to be one of the highest in the world [7]. Similarly 37% of the newborn are low weight [8].
Many of the above mentioned systemic disorders are either caused or aggravated by poor oral hygiene and vice versa. It is now believed that compromised oral health can increase the complications of diabetes mellitus, cardiovascular diseases, respiratory infections, gastrointestinal pathologies, renal ailments, liver problems, bone and joint disease as well as complicate the outcome of pregnancy by increasing the risk of pre-term delivery of low weight babies [9]. These systemic disorders may deteriorate oral health leading to the development of infections such as gingivitis, periodontitis and if left untreated, may cause tooth loss.
Therefore the aim of this study, which is a part of a larger research project evaluating the impact of systemic illnesses on oral hygiene, was to observe and compare the level of oral hygiene in patients with systemic disorders. To the authors’ knowledge, there has been less data available comparing oral health in patients of various systemic diseases.
Materials and Methods
This observational study was approved by the Ethics committee at Ziauddin University, Karachi, Pakistan. The sample size was calculated using online sample size calculator by Raosoft. The recommended minimum sample size was 377, which was increased to 520 for accuracy (non-probability sampling). Data were collected from November, 2012 to February 2013 from two public sectors; tertiary care hospitals in Islamabad namely Pakistan Institute of Medical Sciences (P.I.M.S.), Capital Development Authority (C.D.A.) hospital, outpatient department at Islamic International Dental College and Hospital, Islamabad and Jinnah Postgraduate Medical Center (J.P.M.C.) Karachi which is also a public tertiary care hospital. Patients from nine systemic illnesses were chosen for this study, which are listed in Table 1.
| Systemic Diseases |
Conditions Present |
| Diabetes Mellitus (D.M.) |
Type 1 and Type 2 |
| Cardiovascular disorders (C.V.S.) |
Myocardial infarction, Angina Pectoris |
| Respiratory disorders |
Tuberculosis, Asthma, Chronic obstructive pulmonary disease, Pneumonia |
| Gastrointestinal disorders (G.I.) |
Gastric ulcer, Gastritis, Inflammatory bowel disease, Typhoid. |
| Hepatic disorders |
Hepatitis B & C, Hepatocellular carcinoma. |
| Renal disorders |
Chronic kidney failure, proteinuria. |
| Bone/joint disorders |
Rheumatoid arthritis, osteoarthritis, osteoporosis. |
| Hypertension (H.T.N.) |
Primary hypertension |
| Diabetes Mellitus + Cardiovascular patients (D.M.+ C.V.S.) |
Diabetic patients with co-morbid heart disease. |
Table 1 Systemic disorders along with the most frequent forms of the disorders present in the study population.
Conscious patients with permanent dentition suffering from one of the diseases listed in Table 1 were selected after obtaining informed consent. Patients with acute infections, pain, pregnancy, loss of teeth due to trauma and total absence of teeth were excluded which reduced sample size to 450 patients. For every disease; 50 patients were chosen in the consecutive order with the recruitment stopping when 50 patients were assigned to every disease group. The patients were inquired about their disease and the reason for visiting hospital. Their medical reports were assessed to rule out co-morbidities.
Dental examination was performed using a sterilized dental mirror, periodontal probe, wooden tongue depressor and a torch light. Data for age, gender, number of remaining teeth, decayed, missing and filled teeth (D.M.F.T.) and decayed, missing and filled surfaces (D.M.F.S.) was recorded for every patient (WHO). The normal number of teeth was taken to be 28 excluding 3rd molars for this study.
For statistical analysis, Statistical Package for Social Sciences SPSS 16.0 was used to calculate the mean for each variable along with the standard error. One way ANOVA test was used to find significant differences between study variables. Moreover, Post-hoc Duncan test was applied to categorize diseases that are similar to each other with respect to number of teeth, age, D.M.F.T. and D.M.F.S. The level of significance (α) was 0.005.
Results
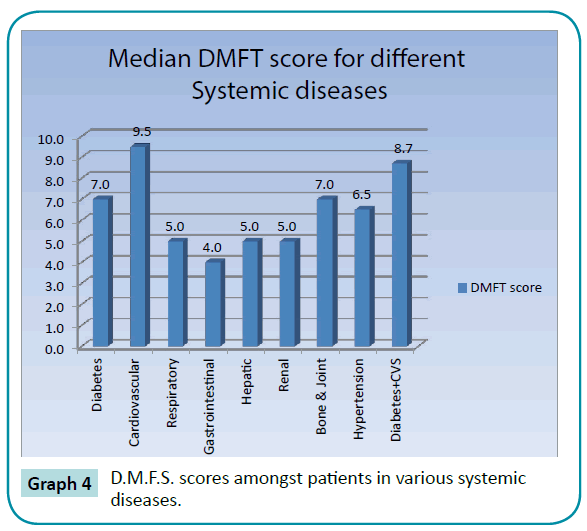
There were equal number of males and females in the selected sample of 450 patients. The mean age of study population was 43.28 years (± 14.45) with an age range of 13-84 years. The mean number of teeth, D.M.F.T. and D.M.F.S. scores were 23.13 (+5.76), 7.93 (± 5.78) and 22.94 (± 19.27), respectively.
Table 2 Results from one way ANOVA analysis for systemic diseases and dependent variables such as age, gender, number of remaining teeth, D.M.F.T. and D.M.F.S scores. The mean value along with standard error in parenthesis is represented.
| Disease |
D.M |
C.V.S |
Respiratory |
G.I |
Hepatic |
Renal |
Bone/ Joint |
H.T.N |
D.M+CVS |
P-value |
| Age |
49 (16.1) |
49.1 (12.1) |
47.6 (10.1) |
39.2 (16) |
37 (13.3) |
35 (12) |
38.3 (12) |
43.6 (16) |
50.8 (11.7) |
0.00 |
| No. of teeth |
21.8 (5.6) |
20.4 (7) |
25.7 (3.9) |
25.6 (3.8) |
25 (3.8) |
23.6 (5) |
21.9 (6.7) |
23.5 (5.3) |
20.7 (7.3) |
0.00 |
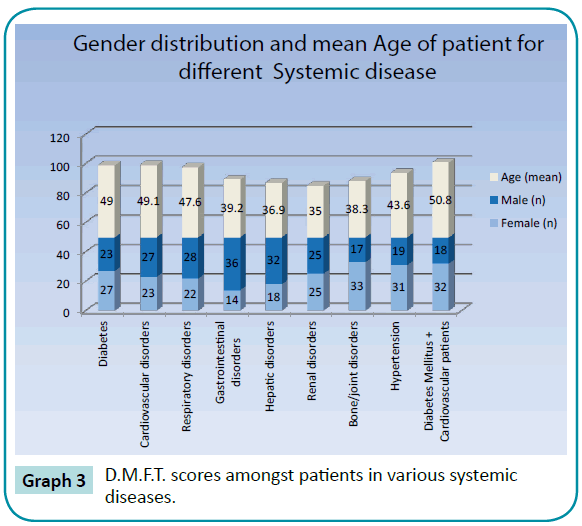
| DMFT |
8.7 (5.4) |
10.5 (6) |
6.1 (4.5) |
5.4 (4.8) |
5.7 (3.9) |
7.2 (5.2) |
9.5 (6.5) |
7.9 (6.1) |
10.4 (6.9) |
0.00 |
| DMFS |
26.9 (18.6) |
32.2 (21.5) |
13.9 (12.5) |
14 (14.4) |
16.6 (16) |
20.7 (19) |
26.4 (20.2) |
23 (19.2) |
32.6 (23.8) |
0.00 |
Table 2 Mean (S.D) with ANOVA test for systemic diseases with respect to age, number of teeth, D.M.F.T. and D.M.F.S. is observed.
By using post-hoc Duncan test, the values for number of remaining teeth, age, D.M.F.T. and D.M.F.S. are represented in Tables 3 and 4. Diseases showing similar patterns were categorized vertically in subset of groups for number of teeth, age, D.M.F.T. and D.M.F.S
| Systemic Disease |
Subset of number of teeth |
Systemic Disease |
Subset of age |
| 1 |
2 |
3 |
1 |
2 |
3 |
4 |
| C.V.S |
20.4 |
|
|
Renal |
35 |
|
|
|
| D.M + CVS |
20.7 |
|
|
Hepatic |
37 |
|
|
|
| D.M |
21.8 |
21.8 |
|
Bone/ Joint |
38.3 |
38.3 |
|
|
| Bone/Joint |
21.9 |
21.9 |
|
G.I |
39.2 |
39.2 |
|
|
| H.T.N |
|
23.5 |
23.5 |
H.T.N |
|
43.6 |
43.6 |
|
| Renal |
|
23.6 |
23.6 |
Respiratory |
|
|
47.6 |
47.6 |
| Hepatic |
|
|
24.9 |
D.M |
|
|
49.0 |
49.0 |
| G.I |
|
|
25.5 |
C.V.S |
|
|
49.1 |
49.1 |
| Respiratory |
|
|
25.7 |
D.M+CVS |
|
|
|
50.8 |
| P-value |
0.20 |
0.14 |
0.07 |
P-value |
0.15 |
0.06 |
0.06 |
0.28 |
Table 3 Homogeneous groups for number of teeth and age of patients with systemic illnesses.
| Systemic Disease |
Subset D.M.F.T. score |
Systemic Disease |
Subset D.M.F.S. score |
| 1 |
2 |
3 |
4 |
1 |
2 |
3 |
4 |
| G.I |
5.4 |
|
|
|
Respiratory |
13.9 |
|
|
|
| Hepatic |
5.7 |
5.7 |
|
|
G.I |
14.0 |
|
|
|
| Respiratory |
6.1 |
6.1 |
|
|
Hepatic |
16.6 |
16.6 |
|
|
| Renal |
7.2 |
7.2 |
7.20 |
|
Renal |
20.8 |
20.8 |
20.8 |
|
| H.T.N |
|
7.9 |
7.86 |
|
H.T.N |
|
23.0 |
23.0 |
|
| D.M |
|
|
8.72 |
8.7 |
Bone/ Joint |
|
|
26.4 |
26.4 |
| Bone/ Joint |
|
|
9.46 |
9.4 |
D.M |
|
|
26.8 |
26.8 |
| D.M+CVS |
|
|
|
10.3 |
C.V.S |
|
|
|
32.2 |
| C.V.S |
|
|
|
10.5 |
D.M+CVS |
|
|
|
32.6 |
| P-value |
0.14 |
0.08 |
0.06 |
0.14 |
P-value |
0.10 |
0.11 |
0.14 |
0.13 |
Table 4 Homogeneous groups for D.M.F.T. and D.M.F.S of patients with systemic diseases.
Table 3 The vertical groups represent diseases showing similar pattern. Some of the diseases in a group share common features with diseases in other group which is shown by repetition of the value of these diseases in the next group. Each subset is significantly different to other subset but non-significant within a subset. Similarly for age groups, but here the order is different than number of teeth.
Table 4 Diseases with similar patterns are represented in vertical groups with diseases sharing common features with other diseases are shown by repetition of the value of these diseases in the next group. Each subset is significantly different to other subset but non-significant within a subset. Similarly for age groups, but here the order is different than number of teeth.
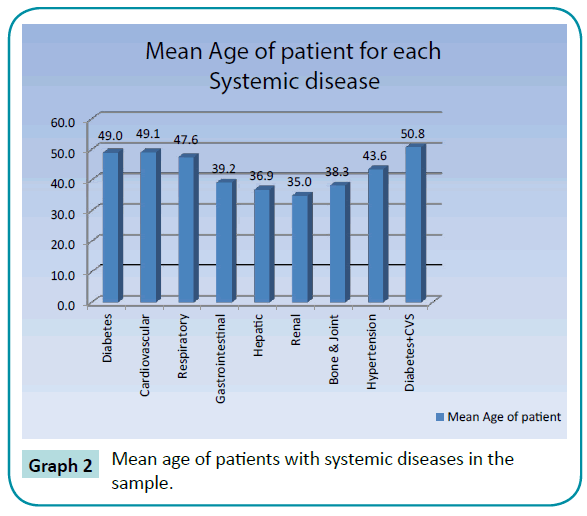
Group 1 diseases
Relatively more males (54%) compared to females (46%) had cardiovascular problems with the mean age of forty nine years which did not differ from mean ages of D.M. sample with or without C.V.S. problems. C.V.S. patients on average had eight missing teeth and the highest D.M.F.T. score. There was greater percentage of females (54%) affected with D.M. compared to males (46%) with the diabetics having an average of seven missing teeth. When D.M. was present as co-morbidity in C.V.S. patients, the tooth loss and D.M.F.T. score increased with the D.M.F.S. score reaching maximum amongst all systemic diseases (Graphs 3 and 4). The last disease in the Group 1 type diseases (Table 3) was bone/joint disorder. 66% females with a mean age of 38.3 years suffered from these disorders making it the most common disease in females with the age group as young as 16-29 years. The patients in our study had on average seven missing teeth and third highest D.M.F.T. scores (Graph 3 and Table 4).
Group 2 diseases
Hypertension was the second most prevalent disease amongst females (62%) after Rheumatoid arthritis. The hypertensive patients in the study had on average five missing teeth. The D.M.F.T. and D.M.F.S. score ranked hypertension as fifth systemic disease to affect the oral health (Graphs 3, 4 and Table 4). The mean age of renal patients was lowest amongst all groups suggesting an earlier onset (35 years). Equal number of males and females were affected by renal disorders (Graphs 1 and 2). Dentally, the disease showed similar pattern to hypertension with five missing teeth.
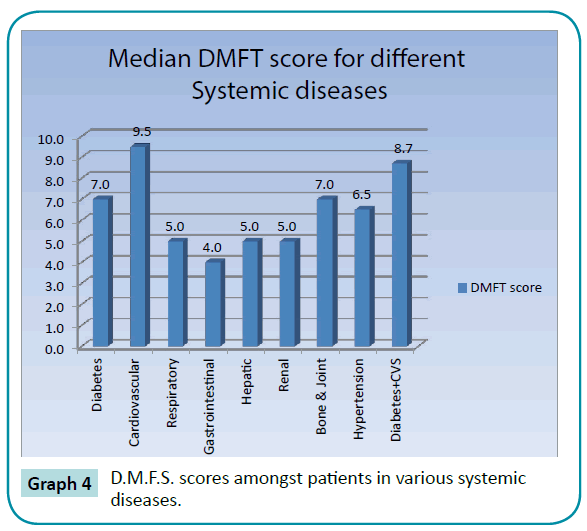
Figure 1: Representation of systemic diseases with respect to gender of patients.
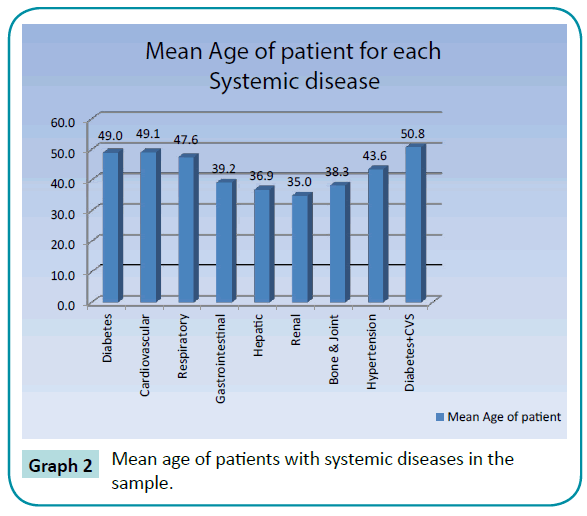
Figure 2: Mean age of patients with systemic diseases in the sample.
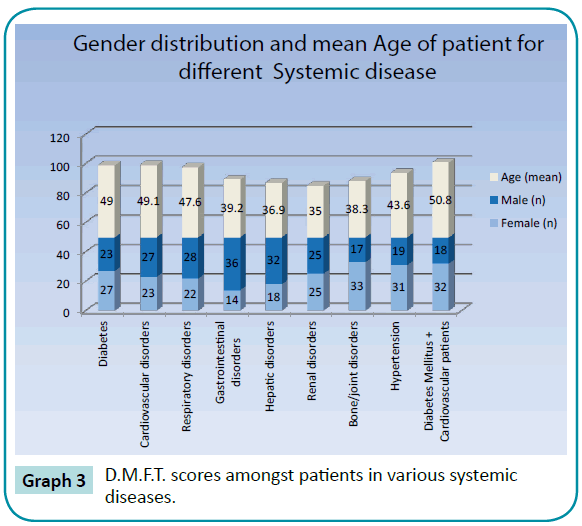
Figure 3: D.M.F.T. scores amongst patients in various systemic diseases.
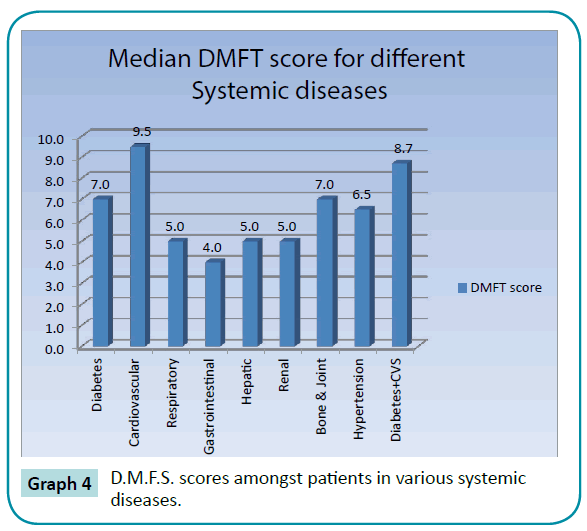
Figure 4: D.M.F.S. scores amongst patients in various systemic diseases.
Group 3 diseases
All the patients with systemic diseases in Group 3 had on average three missing teeth (Table 3). In terms of hepatic pathologies, more males (64%) compared to females (36%) suffered with a mean age of thirty seven years with D.M.F.S. score higher than the D.M.F.T. In the current study, 72% of men suffered from G.I. disorders compared to 28% females with the mean age being thirty nine years (Graphs 1 and 2). Finally respiratory ailments caused least number of tooth loss. As was true for all the Group 3, men had more pulmonary problems (56%) compared to females (44%) with a mean age of forty seven years. These patients had the lowest D.M.F.T. score.
Discussion
Age, gender, number of remaining teeth, D.M.F.T. and D.M.F.S. scores were found to be highly significant with the systemic diseases (p <0.05). This is in accordance to previous findings which list age and gender as risk factors for certain diseases e.g. D.M., Rheumatoid arthritis and C.V.S. disorders [10-12]. Higher prevalence of C.V.S. disorders in men might be attributed to higher cholesterol levels and increased habit of smoking in men [13]. Maximum numbers of missing teeth in C.V.S. patients reflect the poorest oral hygiene amongst all other disease groups which is in accordance with a previous report [14]. Myocardial infarction deteriorates oral health and reports have linked level of periodontal detachment and loss of teeth in cardiac patients to earlier mortality [15]. People with less than ten teeth remaining had seven times higher mortality risk than those having greater than twenty five remaining teeth [16]. Total loss of teeth (edentulism) also increases risk of cerebrovascular disorders such as stroke [17]. Not only C.V.S. problems can cause dental problems, a compromised oral hygiene can also aggravate C.V.S. problems and it has been noted that improving oral hygiene in cardiac patients decrease the chances of thrombus formation and associated complications such as stroke [18]. This might be due to high levels of bacterial endotoxin, proinflammatory cytokines, lipids, fibrinogen and C-reactive protein and platelets, which can cause thromboembolic events such as ischemic stroke [19].
D.M. and compromised oral health affect each other. People with neglected oral hygiene have poor glycemic control and higher Insulin resistance [20]. Periodontitis is listed as sixth complication of D.M. and both types of D.M. promote loss of teeth [21,22]. In terms of global prevalence; South Asians have a higher prevalence of C.V.S., D.M. (Type 2) and Insulin resistance which necessitates the maintenance of good oral hygiene particularly in this population [23].
The current study supports the higher ratio of females compared to males being affected with bone/joint problems with mean age of 38.5 years in Pakistan [11]. It has been reported previously that 43.4% females above twenty years suffer from Osteopenia and about 25% have established Osteoporosis in Pakistan [24]. Periodontitis is also linked to the presence of bone/joint disorders, possibly due to Estrogen deficiency developing earlier in females compared to males [9]. A recent survey showed no strong association between oral health and bone/joint disease, however, the current study places bone/joint disorders in Group 1 diseases that cause greatest number of tooth loss similar to D.M. and C.V.S. disorders [25]. This finding is supported by other studies which relate higher frequency and severity of Periodontitis in Rheumatoid arthritis and Osteoporosis patients, however few have noted a smaller number of decayed teeth in Rheumatoid arthritis patients compared to controls [26-29]. Poor oral hygiene and presence of Porphyromonas gingivalis, a periodontal pathogen, promotes the development of autoimmune antibodies which are responsible for Rheumatoid arthritis [30].
H.T.N. has a high prevalence in Pakistan affecting an estimated 19% of population over the age of 15 years with female population being at a higher risk compared to men [31]. Elevated blood pressure causes alveolar bone loss and is associated with tooth loss in a bidirectional relationship as well [32,33]. People with lesser number of teeth and edentulous patients tend to have higher blood pressure, however one study found no relation between hypertension and oral health [34-36].
Earlier studies on Pakistani population found thirty years as the mean age whereby 25% have been diagnosed with reduction in kidney function [37]. A slightly greater predilection was observed in males in reference to the risk of renal disease by an earlier study which is not in line with our findings [38]. There is reportedly high D.M.F.T. score, poor oral hygiene and alveolar bone loss in patients with kidney disease particularly in patients undergoing hemodialysis [39,40]. Renal patients have more tooth loss and edentulous patients carry higher chances of developing chronic renal failure suggesting bidirectional relation between the two [41,42]. Two studies, however, found no association between kidney problems and oral health [43,44].
A previous study showed 68% of Pakistani men to be affected with hepatic problems compared to 31% females with the most cases occurring in the age range of 20-39 years which is similar to our findings [45,46]. Decreased oral hygiene has been linked to the presence of hepatic disease and in turn poor oral health can cause liver abscess formation [47,48]. It has also been observed that patients presenting with Hepatitis C have higher chances of developing Periodontitis [47].
Gastrointestinal disorders are also frequent with 60% reported prevalence of gastritis [49]. Furthermore H.pylori; bacteria linked to gastritis, gastric ulcers and increased insulin resistance has been found in the drinking water in many cities of the country [50,51]. G.I. disorders are highly prevalent in men (Graph 1) and a previous study also yielded same results [52]. People having neglected oral hygiene have greater number of Helicobacter pylori in the mouth which can cause gastric disorders as well as recurrence of these disorders [53]. This bacterium produces volatile Sulfur compounds responsible for halitosis and glossitis [54]. A study has linked the production of these compounds to the concomitant levels of gastric mucosal injury, thereby halitosis may be reflective of gastric injury [55]. Moreover it is also linked to increased caries risk and higher D.M.F.T. score compared to controls [56]. Conditions such as inflammatory bowel disease, Crohn’s disease and ulcerative colitis also affect oral hygiene negatively [57,58].
A higher incidence of respiratory problems in men compared to females with the mean age of 46.3 years has been already reported [56]. Tuberculosis, Chronic obstructive pulmonary disease, asthma and other respiratory diseases impact oral health negatively and less than optimum oral hygiene can cause decrease in lung function as well as increase the chance of pneumonia [59-63]. The less number of missing teeth along with lowest D.M.F.T. score reflects the fewest dental problems amongst in the sample.
The strength and weakness of the study deserve mentioning. This study is to compare oral health in patients with multiple systemic illnesses. Sample size was increased to have better evaluation of risk factors responsible for tooth loss. The weaknesses of the study include no adjustment for known cofounders like socioeconomic factors, failure to record the severity of the underlying systemic diseases owing to the lack of funds and lab facilities available and also not having control group of health subjects to compare the findings.
Conclusion
This study highlights association between age, gender, tooth loss, D.M.F.T., D.M.F.S. score and systemic diseases. Diseases such as cardiovascular disorders, diabetes mellitus with and without cardiovascular pathologies and bone/joint disorders negatively impact oral hygiene. Greatest loss of teeth and higher indices were observed in these patients. Hypertensive and renal patients had comparable oral hygiene to diabetes mellitus and bone/ joint patients. The earlier onset of renal diseases is alarming as observed in this study. Patients suffering from pathologies of liver, gastrointestinal tract and respiratory system had compromised oral hygiene though relatively less compared to other diseases studied in this group. Therefore it is the need of the hour to educate the dentists, general physicians and specialists about the association of systemic diseases with oral health and vice versa as many of the systemic diseases may be prevented and improved by improving oral hygiene.
Acknowledgments
We would like to pay special thanks to Col (R) Dr. Haq Nawaz, Dr. Sebastian Doeltgen, Dr. Usman Nawaz, Dr. Asad Noor at C.D.A. hospital, Dr. Rizwan at P.I.M.S. hospital and to Arsalan Yahya for the valuable help offered during this study.
6517
References
- Jafar, T.H., Jafary, F.H., Jessani, S.,Chaturvedi, N. Heart disease epidemic in Pakistan: women and men at equal risk. Am Heart J 2005; 150: 221-226.
- Jamal-u-Din Qureshi., M.B., Khan, A.J. Prevalence of diabetic retinopathy among individuals screened positive for diabetes in five community-based eye camps in northern Karachi, Pakistan. J Ayub Med Coll Abbottabad. 2006;18(3):40-43.
- Hasnain, J., Memon, G.N., Memon, A., Channa, A.A., Creswell, J., et al. Screening for HIV among tuberculosis patients: a cross-sectional study in Sindh, Pakistan. BMJ Open 2012; 2.
- Ali, M., Idrees, M., Ali, L., Hussain, A., Ur,Rehman, I., et al. Hepatitis B virus in Pakistan: a systematic review of prevalence, risk factors, awareness status and genotypes. Virol J 2011; 8: 102.
- Ali, S., Iram, S. Comparative effectiveness and adverse effects of interferon alpha-2b plus ribavirin therapy in hepatitis 'C' for 26 weeks. J Ayub Med Coll Abbottabad 2009; 21: 15-18.
- Khealani, B.A., Hameed, B., Mapari, U.U. Stroke in Pakistan. J Pak Med Assoc 2008; 58: 400-403.
- Jafar, T.H. Blood pressure, diabetes, and increased dietary salt associated with stroke--results from a community-based study in Pakistan. J Hum Hypertens 2006; 20: 83-85.
- Qureshi, A., Ijaz, S., Syed, A., Qureshi, A., Khan, AA. Periodontal infection: a potential risk factor for pre-term delivery of low birth weight (PLBW) babies. J Pak Med Assoc 2005; 55: 448-452.
- Kim, J., Amar, S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology 2006; 94: 10-21.
- Zafar, J., Bhatti, F., Akhtar, N., Rasheed, U., Bashir, R., et al. Prevalence and risk factors for diabetes mellitus in a selected urban population of a city in Punjab. J Pak Med Assoc 2011; 61: 40-47.
- Alam, S.M., Kidwai, A.A., Jafri, S.R., Qureshi, B.M., Sami, A., et al. Epidemiology of rheumatoid arthritis in a tertiary care unit, Karachi, Pakistan. J Pak Med Assoc 2011; 61: 123-126.
- Kamal, A.K., Itrat, A., Murtaza, M., Khan, M., Rasheed, A., et al. The burden of stroke and transient ischemic attack in Pakistan: a community-based prevalence study. BMC Neurol 2009; 9: 58.
- Saleheen, D., Frossard, P. CAD risk factors and acute myocardial infarction in Pakistan. ActaCardiol 2004; 59: 417-424.
- Chin, U.J., Ji, S., Lee, S.Y., Ryu, J.J., Lee, J.B., et al. Relationship between tooth loss and carotid intima-media thickness in Korean adults. J AdvProsthodont 2010; 2: 122-127.
- Linden, G.J., Linden, K., Yarnell, J., Evans, A., Kee, F., et al. All-cause mortality and periodontitis in 60-70-year-old men: a prospective cohort study. J ClinPeriodontol 2012; 39: 940-946.
- Holmlund, A., Holm, G., Lind, L. Number of teeth as a predictor of cardiovascular mortality in a cohort of 7,674 subjects followed for 12 years. J Periodontol 2010; 81: 870-876.
- Watt, R.G., Tsakos, G., de, Oliveira, C., Hamer, M. Tooth loss and cardiovascular disease mortality risk--results from the Scottish Health Survey. PLoS One 2012; 7: e30797.
- Mattila, K.J., Pussinen, P.J., Paju, S. Dental infections and cardiovascular diseases: a review. J Periodontol 2005; 76: 2085-2088.
- Grau, A.J., Becher, H., Ziegler, C.M., Lichy, C., Buggle, F., et al. Periodontal disease as a risk factor for ischemic stroke. Stroke 2004; 35: 496-501.
- Jin, L.J., Chiu, G.K., Corbet, E.F. Are periodontal diseases risk factors for certain systemic disorders--what matters to medical practitioners? Hong Kong Med J 2003; 9: 31-37.
- Moore, P.A., Zgibor, J.C., Dasanayake AP Diabetes: a growing epidemic of all ages. J Am Dent Assoc 2003; 134 Spec No: 11S-15S.
- Tanwir, F., Altamash, M., Gustafsson, A. Effect of diabetes on periodontal status of a population with poor oral health. ActaOdontolScand 2009; 67: 129-133.
- Jafar, T.H., Chaturvedi, N., Pappas, G. Prevalence of overweight and obesity and their association with hypertension and diabetes mellitus in an Indo-Asian population. CMAJ 2006; 175: 1071-1077.
- Jaleel, R., Nasrullah, F.D., Khan, A. Osteopenia in younger females. J Surg Pakistan. 2010;15:29–33.
- Demmer, R.T., Molitor, J.A., Jacobs,D.R.Jr., Michalowicz, B.S. Periodontal disease, tooth loss and incident rheumatoid arthritis: results from the First National Health and Nutrition Examination Survey and its epidemiological follow-up study. J ClinPeriodontol 2011; 38: 998-1006.
- Pepelassi, E., Nicopoulou-Karayianni, K., Archontopoulou, A.D., Mitsea, A., Kavadella, A., et al. The relationship between osteoporosis and periodontitis in women aged 45-70 years. Oral Dis 2012; 18: 353-359.
- de Pablo, P., Chapple, I.L., Buckley, C.D., Dietrich, T. Periodontitis in systemic rheumatic diseases. Nat Rev Rheumatol 2009; 5: 218-224.
- Garib, B.T., Qaradaxi, S.S.Temporomandibular joint problems and periodontal condition in rheumatoid arthritis patients in relation to their rheumatologic status. J Oral MaxillofacSurg 2011; 69: 2971-2978.
- de Pablo, P., Dietrich, T., McAlindon, T.E. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J Rheumatol 2008; 35: 70-76.
- Rutger, P.G. Rheumatoid arthritis and periodontitis - inflammatory and infectious connections. Review of the literature. J Oral Microbiol 2012; 4.
- Humayun, A., Shah, A.S., Sultana R Relation of hypertension with body mass index and age in male and female population of Peshawar, Pakistan. J Ayub Med Coll Abbottabad 2009; 21: 63-65.
- de Medeiros,Vanderlei, J.M., Messora, M.R., Fernandes, P.G., Novaes,A.B.Jr., Palioto, D.B., et al. Arterial hypertension perpetuates alveolar bone loss. ClinExpHypertens 2013; 35: 1-5.
- Alman, A.C., Johnson, L.R., Calverley, D.C., Grunwald, G.K., Lezotte, D.C., et al. Loss of alveolar bone due to periodontal disease exhibits a threshold on the association with coronary heart disease. J Periodontol 2011; 82: 1304-1313.
- Lee, H.K., Lee, K.D., Merchant, A.T., Lee, S.K., Song, K.B., et al. More missing teeth are associated with poorer general health in the rural Korean elderly. Arch GerontolGeriatr 2010; 50: 30-33.
- Ayo-Yusuf, O.A., Ayo-Yusuf, I.J. Association of tooth loss with hypertension. S Afr Med J 2008; 98: 381-385.
- Rivas-Tumanyan, S., Spiegelman, D., Curhan, G.C., Forman, J.P., Joshipura, K.J Periodontal disease and incidence of hypertension in the health professionals follow-up study. Am J Hypertens 2012; 25: 770-776.
- Saeed, Z.I., Hussain, S.A. Chronic kidney disease in Pakistan: an under-recognized public health problem. Kidney Int 2012; 81: 1151.
- Jamro, S., Channa, N.A., Shaikh, A.H., Ramzan, A. Chronic renal failure in children. J Pak Med Assoc 2003; 53: 140-142.
- Brito, F., Almeida, S., Figueredo, C.M., Bregman, R., Suassuna, J.H., et al. Extent and severity of chronic periodontitis in chronic kidney disease patients. J Periodontal Res 2012; 47: 426-430.
- Guerra, E.N., Vianna, L., Sobreira, M.N., de Araújo, F.N., de Melo, N.S. Oral manifestations of hyperoxaluria. J CraniofacSurg 2011; 22: 2191-2192.
- Tramini, P., Montal, S., Valcarcel, J. Tooth loss and associated factors in long-term institutionalised elderly patients. Gerodontology 2007; 24: 196-203.
- Klassen, J.T., Krasko, B.M. The dental health status of dialysis patients. J Can Dent Assoc 2002; 68: 34-38.
- Ardalan, M.R., Ghabili, K., Pourabbas, R., Shoja, M.M.A causative link between periodontal disease and glomerulonephritis: a preliminary study. TherClin Risk Manag 2011; 7: 93-98.
- Garcez, J., Limeres, P.J., Carmona, I.T., Feijoo, J.F., Diz Dios, P. Oral health status of patients with a mild decrease in glomerular filtration rate. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 2009; 107: 224-228.
- Khan, F., Shams, S., Qureshi, I.D., Israr, M., Khan, H., et al. Hepatitis B virus infection among different sex and age groups in Pakistani Punjab. Virol J 2011; 8: 225.
- Centers for Disease Control and Prevention (CDC) Establishment of a viral hepatitis surveillance system--Pakistan, 2009-2011. MMWR Morb Mortal Wkly Rep 2011; 60: 1385-1390.
- Coates, E.A., Brennan, D., Logan, R.M., Goss, A.N., Scopacasa, B., et al. Hepatitis C infection and associated oral health problems. Aust Dent J 2000; 45: 108-114.
- Ohyama, H., Nakasho, K., Yamanegi, K., Noiri, Y., Kuhara, A., et al. An unusual autopsy case of pyogenic liver abscess caused by periodontal bacteria. Jpn J Infect Dis 2009; 62: 381-383.
- Ahmed, J., Haider, S.I., Choudhri, A.N. Dyspepsia in a rural cohort. J Coll Physicians Surg Pak 2004; 14: 91-93.
- Khan, A., Farooqui, A., Kazmi, S.U. Presence of Helicobacter pylori in drinking water of Karachi, Pakistan. J Infect DevCtries 2012; 6: 251-255.
- Gen, R., Demir, M., Ataseven, H. Effect of Helicobacter pylori eradication on insulin resistance, serum lipids and low-grade inflammation. South Med J 2010; 103: 190-196.
- Bhurgri, Y., Pervez, S., Kayani, N., Haider, S., Ahmed, R., et al. Rising incidence of gastric malignancies in Karachi, 1995- 2002. Asian Pac J Cancer Prev 2009; 10: 41-44.
- Al Asqah, M., Al Hamoudi, N., Anil, S., Al Jebreen, A., Al-Hamoudi WK Is the presence of Helicobacter pylori in dental plaque of patients with chronic periodontitis a risk factor for gastric infection? Can J Gastroenterol 2009; 23: 177-179.
- Adler, I., Denninghoff, V.C., Alvarez, M.I., Avagnina, A., Yoshida, R., et al. Helicobacter pylori associated with glossitis and halitosis. Helicobacter 2005; 10: 312-317.
- Yoo, S.H., Jung, H.S., Sohn, W.S., Kim, B.H., Ku, B.H., et al. Volatile sulfur compounds as a predictor for esophagogastroduodenal mucosal injury. Gut Liver 2008; 2: 113-118.
- Kolho, K.L., Hölttä, P., Alaluusua, S., Lindahl, H., Savilahti, E., et al. Dental caries is common in Finnish children infected with Helicobacter pylori. Scand J Infect Dis 2001; 33: 815-817.
- Habashneh, R.A., Khader, Y.S., Alhumouz, M.K., Jadallah, K., Ajlouni, Y., The association between inflammatory bowel disease and periodontitis among Jordanians: a case-control study. J Periodontal Res 2012; 47: 293-298.
- Brito, F., de Barros, F.C., Zaltman, C., Carvalho, A.T., Carneiro, A.J., et al. Prevalence of periodontitis and DMFT index in patients with Crohn's disease and ulcerative colitis. J ClinPeriodontol 2008; 35: 555-560.
- Hussain, S.F., Aziz, A., Fatima,H. Pneumothorax: a review of 146 adult cases admitted at a university teaching hospital in Pakistan. J Pak Med Assoc 1999; 49: 243-246.
- Kakisi, O.K., Kechagia, A.S., Kakisis, I.K., Rafailidis, P.I., Falagas, M.E. Tuberculosis of the oral cavity: a systematic review. Eur J Oral Sci 2010; 118: 103-109.
- Widmer RP., Oral health of children with respiratory diseases. PaediatrRespir Rev 2010; 11: 226-232.
- Holtfreter, B., Richter, S., Kocher, T., Dörr, M., Völzke, H., et al. Periodontitis is related to lung volumes and airflow limitation: a cross-sectional study. EurRespir J 2013; 42: 1524-1535.
- Soh, K.L., Shariff, G.S., Soh, K.G., Abdul, R.R., Sharif, A.S.S., et al. Oral care practice for the ventilated patients in intensive care units: a pilot survey. J Infect DevCtries 2012; 6: 333-339.