Sukanya S1, Rachana S2,V. Lakshmi3* , Rashesh S4, N. Bheerappa5, Shantveer G. Uppin6
1Senior Resident, Department of Microbiology
2Department of Microbiology & Immunology, Faculty of Pharmacy, Ain Shams University, Cairo, Egypt
3Department of Pharmaceutical Microbiology, College of Pharmacy, Taif University, KSA
4Department of Pharmaceutical Microbiology, College of Pharmacy, Taif University, KSA
5Department of Pharmaceutical Microbiology, College of Pharmacy, Taif University, KSA
6Department of Pharmaceutical Microbiology, College of Pharmacy, Taif University, KSA
- *Corresponding Author:
- V. Lakshmi
E-mail: vemulakshmigorthi@gmail.com
Introduction
Typhoid fever, caused by Salmonella Typhi (S. Typhi), presents with a wide variety of systemic manifestations both intestinal and extra-intestinal. The common serious surgical complication of typhoid fever is intestinal perforation, with high morbidity and mortality.[1] However acute cholecystitis is rare, [2] while typhoid perforation of the gall bladder is extremely uncommon, [3] more so if it is an acalculous cholecystitis [4].
Case report
An 18 year old female presented with complaints of recurrent upper abdominal pain of 3 months duration which intensified in severity 3 days before admission to this institute. The pain was associated with high grade fever and bilious vomiting of 5 days duration. There was no associated history of melena, hematemesis and constipation. Before the present admission, an ultrasound abdomen, done elsewhere, showed sludge in the gallbladder. A fever work up showed a significant Widal titre of 1: 160 against both S. Typhi O and H antigens. She was managed conservatively and referred to our hospital. On thorough examination, she was found to be conscious, febrile with signs of generalized peritonitis. A complete hemogram showed polymorphonuclear leukocytosis. Total proteins were 57 g/L with an albumin of 28 g/L and serum amylase 102 U/L. A plain radiograph of the abdomen did not reveal any pneumo-peritoneum. Contrast enhanced computed tomography (CECT) abdomen revealed multiple interloop and subphrenic fluid collections with free fluid in the pelvis. As she had generalized peritonitis, an exploratory laparotomy was performed.
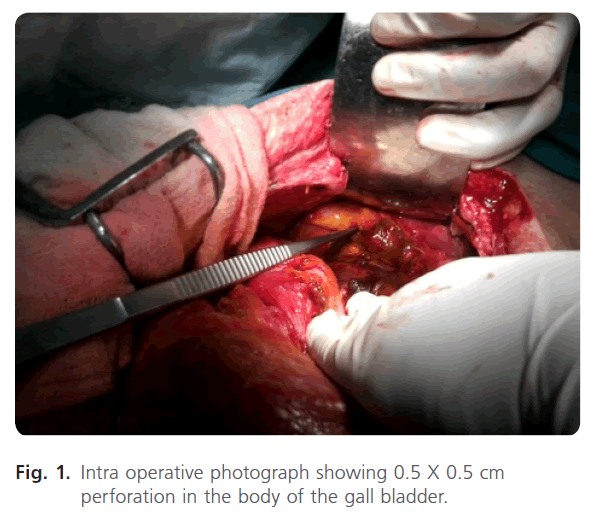
Intra operatively, 1.5 litres of bilious fluid was found in the peritoneal cavity with fibrin flakes on the small intestine. A very small perforation in the gall bladder was identified (Fig. 1) for which cholecystectomy was performed. Common bile duct, duodenum and rest of the viscera were within normal limits.
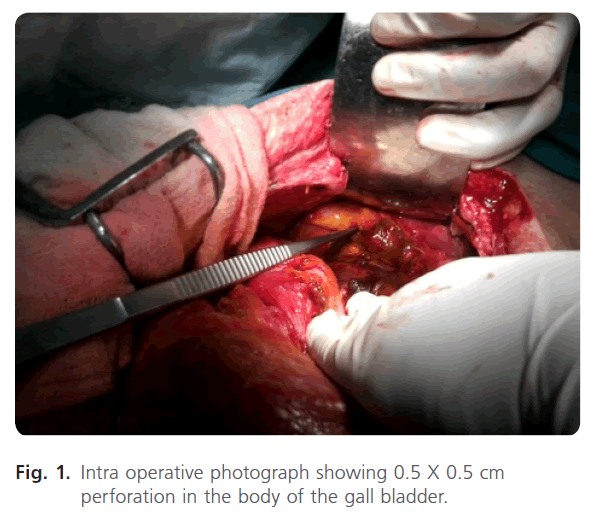
Figure 1: Intra operative photograph showing 0.5 X 0.5 cm perforation in the body of the gall bladder.
The gall bladder sludge and the peritoneal fluid were sent for microbiology processing and the gall bladder was sent for histopathology.
Microbiology: Gram’s stain of the sludge and the fluid showed Gram negative bacilli with plenty of pus cells. The specimen were inoculated on 5% sheep blood agar (COS, bioMerieux, Marcy l’Etoile- France) and chromo agar plates (CPS ID, bioMerieux, Marcy l’Etoile- France) and incubated at 37 C aerobically for 24 hours. Anaerobic culture was done on 5% sheep blood agar for 48 hours at 37 C. Pure growth of pale, moist, round, colonies (non haemolytic on blood agar), was observed both aerobically and anaerobically, from both the sludge and the peritoneal fluid. The isolate was identified as S. Typhi (99.9%) by the Vitek-2 system using the ID GN panel (bioMerieux, Marcy l’Etoile- France). The Minimum Inhibitory Concentration (MIC) was determined by Vitek-2 using N 090 panel. Nalidixic acid susceptibility testing was per- formed with the API system using ATBE(bioMerieux, Marcy l’Etoile- France). S. Typhi isolate was sensitive to ceftriaxone (MIC <=1μg/ml), ciprofloxacin (MIC = 1μg/ml) and resistant to nalidixic acid. The antigenic structure was 9, 12, Vi:d:- as per CRI, Kasauli.
Two sets each of pre and postoperative blood cultures, processed by the automated BacT/Alert system (bioMerieux, Marcy l’Etoile- France) were sterile after 5 days.
A repeat Widal test, pre operatively, showed increased titres of >1:640 for both S. Typhi O and H antigens.
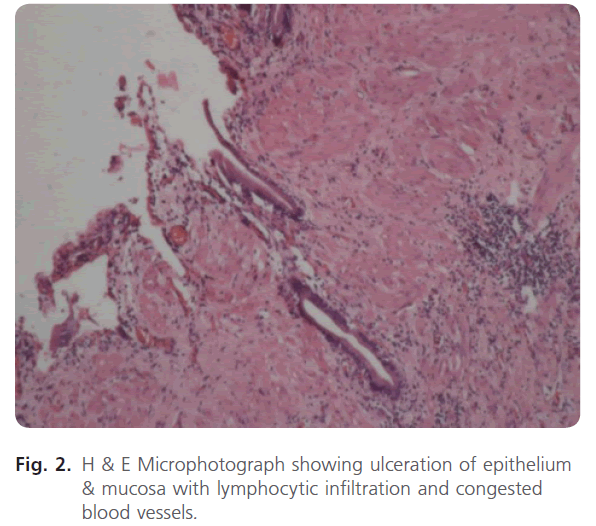
Histopathology of the gall bladder wall showed evidence of acute on chronic cholecystitis with perforation (Fig. 2).
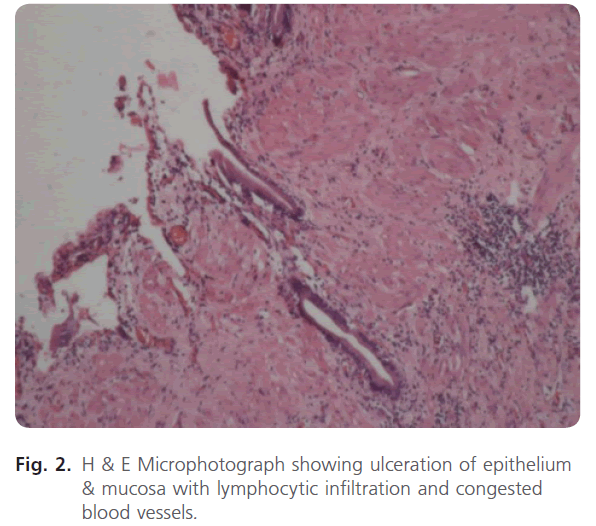
Figure 2: H & E Microphotograph showing ulceration of epithelium & mucosa with lymphocytic infiltration and congested blood vessels.
Based on the antibiotic susceptibility report, the patient was administered intravenous ceftriaxone 500 mg, twice daily, for 1 week. Widal test, repeated on seventh post- operative day, showed decreasing titres of 1:320 and 1:640 for S. Typhi O and H antigens respectively.
The postoperative period was uneventful, the surgical wounds healed well and the patient was discharged on the ninth postoperative day with double strength co-trimoxazole, 160/800 mg orally twice daily for 14 days. At follow up, after 15 days, the patient was doing well with no further complaints.
Discussion
Surgical complications of typhoid fever are uncommon and when they occur, they usually involve the small intestine, generally the ileum, than the gallbladder. [1] Such complications are more often seen in children and adolescents.
As typhoid GBP is a rare surgical sequel of typhoid infection [1, 5], it is rarely suspected preoperatively even in places where typhoid ileal perforation is rampant [5]. In a case of biliary peritonitis, the condition of the GB at surgery should be thoroughly assessed, often is an important clue to GBP.
The pathophysiology of GBP may be caused by an inflammatory reaction and weakness of its wall in the course of the disease due to multiplication of S. Typhi in high numbers in the bile [3]. The intense inflammation caused by the highly virulent S. Typhi leads to perforation. Such events are more often seen in immunocompromised states and in the young. The inflammation is associated with thrombosis of the blood vessels and a subsequent transmural necrosis and perforation [6]. .In the present case, collection of sludge in the GB and the prolonged typhoid carrier state probably led to GBP.
If no obvious hollow viscous perforation is found, a meticulous examination of the gall bladder particularly for any sign of patchy gangrene or impending perforation is recommended [5]. Surgical management is fairly straightforward in a GBP, as cholecystectomy is curative, as in the present case.
Through an extensive literature and PubMed search, only 21 publications on typhoid GBP were found since 1895 till date. The first published case of typhoid GBP was by Montagu.F et al in 1895. Subsequently, most of the typhoid GBP was reported from Asian countries (5 cases from India, 4 from Pakistan and 1 from Nepal) [1-7, 10]. Rest of the cases were reported from Europe (2 cases from London, 1 case from Germany) [8, 11], Africa (3 cases from Nigeria) [7, 10] and the United States of America (5 cases from Philadelphia)[9]. The outcome among most of these cases was generally good following timely management. Six more publications were found through PubMed search (Abstracts are not available) [12, 13, 14, 15, 16, 17].
Conclusion
The worldwide number of cases of typhoid GBP as documented, over the past century, indicates the rarity of this surgical complication of typhoid fever. GBP secondary to typhoid fever should be considered as a differential diagnosis in patients with suspected typhoid enteric perforation in endemic regions. [7]. Cholecystectomy is curative and will help to reduce morbidity and mortality in such cases.
128
References
- Memon, AA. Perforated gall bladder.A Case Report.J Surg Pakistan 2011; 6: 37.
- Bhandari, RS., Singh, KP. Gall Bladder Perforation by Typhoid Complication.J Nepal Health Res Counc.2009; 7: 52-53.
- Pandey, A., Gangopadhay, AN., Kumar, V. Gall bladder perforation as complication of typhoid fever. Saudi J Gastroenterol 2008; 14: 213.
- Shukla, VK.,Khandelwal, C., Kumar, M., Vaidya, MP. Enteric perforation of the gall bladder.Postgrad Med J. 1983; 59: 125-126.
- Saxena, V., Basu, S., Sharma, CL. Perforation of the gall bladder following typhoid fever induced ileal perforation. Hong Kong Med. J. 2007; 13: 475-477.
- Singh, S., Mohanty, D., Singh, B., Kumar Jain, B. Enteric fever with gall bladder perforation. Tropical gastroenterology 2010; 31: 48-49.
- Gali, BM., Ali, N., Agbese, GO.,Duna, VD. Gall bladder perforation complicating typhoid fever: report of two cases. Niger J Med. 2011; 20: 181-183.
- Hawkins, F. On Jaundice and on Perforation of the Gall-bladder in Typhoid Fever.Med Chir.Trans. 1987; 80: 131-140.
- Alexander, EG. Acute Perforation or Rupture of The Gall- Bladder. Annals Of Surgery 1927; 8: 765-770.
- Mirza, B., Ijaz, L., Saleem, M., Iqbal, S., Sharif, M., Sheikh, A. Management of biliary perforation in children. Ann Surg. 1907; 45: 34-41.
- Kiliani, OG. Typhoid with Double Perforation of Ileum and Perforation of Gallbladder: Intestinal Suture cholecystectomy. Afr J. Paediatr. Surg. 2010; 7: 147-150.
- Idjradinata, P., Suroto-Hamzah, E., Sugiri, S. A case of perforation of the gallbladder in association with typhoid fever (case report) PMID: 4427776. 1974.
- Strizhakov, NV. Perforation of the gall bladder into the free abdominal cavity at the height of typhoid fever. PMID: 5607603. 1967.
- Goldberger, A., Protic, MG. Gallbladder perforation as a complication of typhoid fever. PMID: 13377918. 1956.
- Veronesi, G. Gallbladder perforation in typhoid fever. PMID:13193785. 1954.
- Klein, K. Gall bladder perforation complicating typhoid fever in a child. PMID: 12982504. 1952.
- Vargas, M., Peña, A. Perforated viscera in typhoid fever: A better prognosis for children. Journal of Pediatric Surgery 1975; 8: 531-532.