Keywords:
Femoral head fracture; Associated injuries; MBI; Sex; Height; Weight
Introduction
In 1895, an autopsy was performed on a 35-year-old woman who had fallen from 2nd floor story building by John [1]. He observed prior to the procedure that the left leg was inverted and slightly shorter than the right leg. This was the first report of femoral head fracture (FHF) in history. FHF is very uncommon, some literature has reported occurrence rates as two cases per one million [2]. Hence large patient study, metaanalysis and validated outcomes are difficult to find [3-6]. However, the recognition of this injury has led to their classification systems, standardized treatment approaches and last but not the least conduction of studies in this field. Reported causes of FHF include simple falls (especially in elderly), fall from heights and sports injury but the most common is vehicular motor accidents. Fracture diagnosis and classification are mostly done through radiographic analysis. Complications include heterotopic ossification (2%-54%), femoral head necrosis (0%-24%), peripheral nerve damage (7%-27%) and post-traumatic degenerative disease (0%-72%) [7-9].
Anatomically the femoral head is part of the complex structures of the hip. Hip fracture is fast growing due to increase in road accidents [10]. It has been estimated that by 2050 there will be 4.5 to 6.3 million incidence of hip fracture [11,12]. And posterior hip fractures have about 4%-17% association with FHF [13-18].
Age, sex, weight, height and BMI have been documented in some literatures as risk factors in the occurrences of hip fracture. Evidence of these reports is inconclusive and furthermore, there has been no association of these parameters with FHF. We therefore conducted this study to investigate the relationship in these patients using Pipkin Femoral head classification system.
Materials and Methods
We did a retrospective study of all FHF patients registered in our hospital database between January 2003 to September 2017. We collected selected variables from the computerized hospital records such as age, sex, height, weight, BMI, length of hospital stay, with associated injuries (AI) or not and time of follow-up. Injuries here were defined as major traumas to the head, trunk and to the lower and upper limbs that needed medical attention like those to nerves, ligaments, bone fractures, internal bleeding and others. Minor injuries like bruises and lacerations were excluded. Patients who received diagnosis of FHF but had no radiological findings were excluded. Exclusion criteria also included patients with pathological fractures and unavailable details of clinical records. FHF was classified using Pipkin classification system. The Pipkin classification system uses fracture pattern to categorize femoral head fracture as follows;
• Type I is a facture below the fovea capitis femoris.
• Type II is a fracture above the fovea capitis femoris.
• Type III is a Type I or Type II fracture with femoral neck fracture.
• Type IV is a Type I or Type II fracture with acetabulum fracture.
All medical records, radiographs and classifications were reviewed at least twice by qualified orthopedic specialist.
In cases where the BMI were unknown, height and weight ascertain from the medical record were used in calculating the BMI by dividing weight in Kilograms by height in meters squared. The patients were divided in two groups; group with associated injury (AI) and the group without other associated injury. These two groups where then statistically studied against the following variables; BMI (<23 kg/m2 and >23 kg/ m2), age (<50 and >50 years), weight (<57 kg and >57 kg), height (<167 cm and >167 cm), and location of FHF on either the left and right leg.
Data were analyzed using IBM SPSS version 19 (SPSS Inc. Chicago Illinois, USA). Student’s t test was used for comparing quantitative variables between the groups with and without other associated injuries. An association between the two groups was assessed using Chi-square test. A P value of <5% was considered as statistical significance. Origin 8E software was used in plotting the graphs.
Results
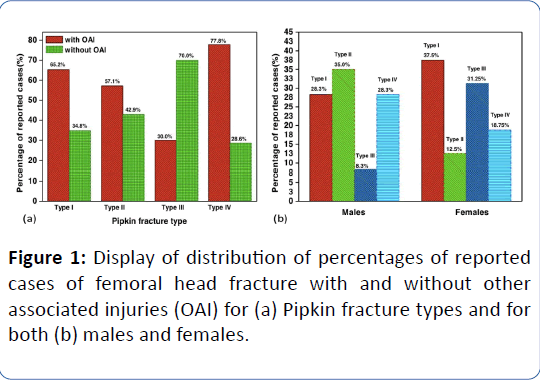
Between January 2003 and September 2017 there were a total of 72 patients eligible for the study with an average follow-up of 17 months (from 1/2 month-122 months). Two patients had bilateral Pipkin type I fractures. There were 57 males (79.2%) and 15 females (20.8%). We had 25 cases (33.8%) type I, 21 cases (28.4%) type II, 10 cases (13.5%) type III and 18 cases (23.3%) of type IV fractures. Details of medical records retrieved have been shown in Table 1. Figures 1-3 show the plotted graphs of results retrieved from our dataset.
| |
Pipkin Classification |
| |
Type I |
Type II |
Type III |
Type IV |
| Age/Years |
36.2+12.7 |
38.1+16.7 |
53.7+23.9 |
43.5 ± 13.0 |
| Height/cm |
168.7+7.2 |
171.1+5.5 |
163.6+8.0 |
168.5+7.8 |
| Weight/cm |
60.5+12.1 |
59.4 ± 18.2 |
49.1+16.2 |
69.1+16.0 |
| BMI/(kg/m2) |
21.0+3.3 |
20.2 ± 5.4 |
18.9+4.9 |
24.8+7.4 |
| Hospital stay/days |
19.9 ± 2.1 |
13.1+9.0 |
13.5+3.5 |
25.7 ± 6.5 |
Table 1: Showing clinical variables obtained from 72 patients. Numerical data expressed as mean ± standard deviation.
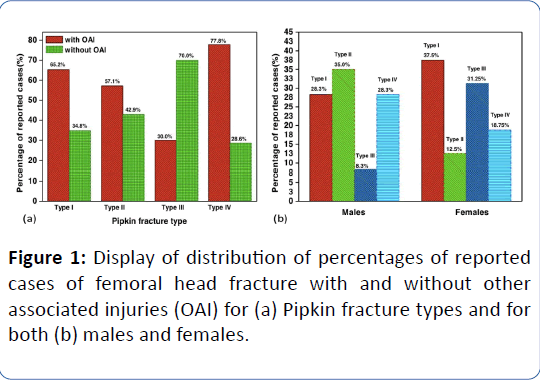
Figure 1: Display of distribution of percentages of reported cases of femoral head fracture with and without other associated injuries (OAI) for (a) Pipkin fracture types and for both (b) males and females.
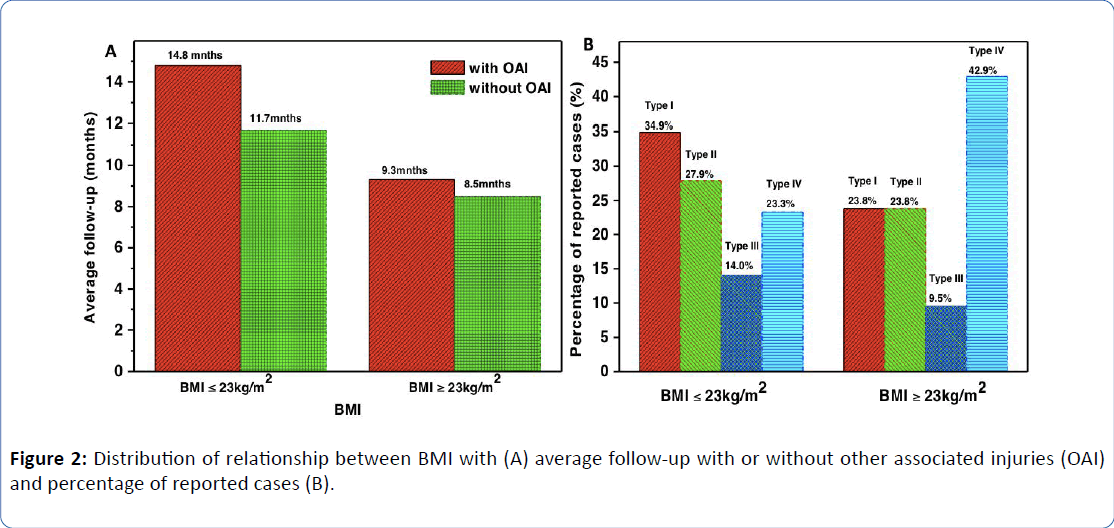
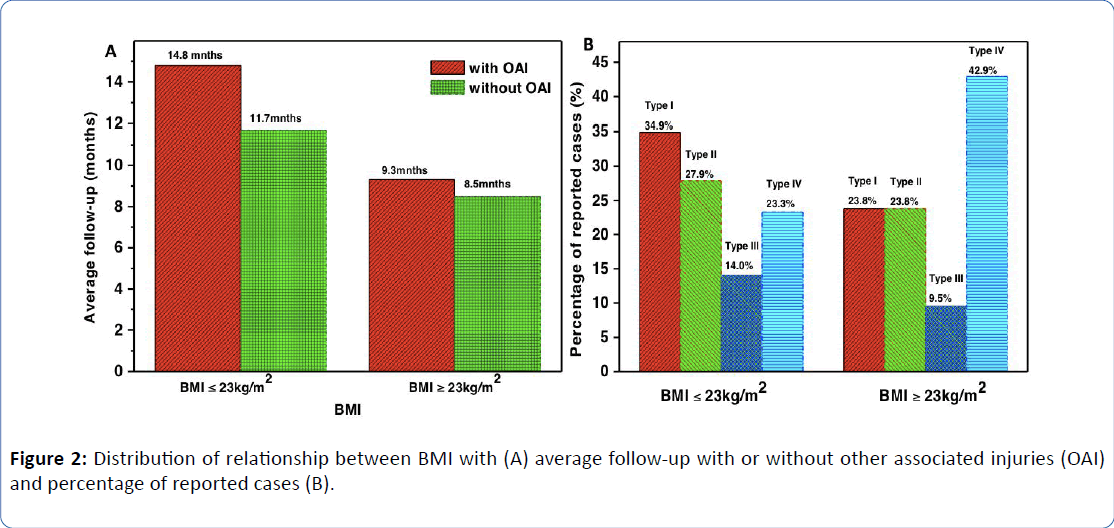
Figure 2: Distribution of relationship between BMI with (A) average follow-up with or without other associated injuries (OAI) and percentage of reported cases (B).
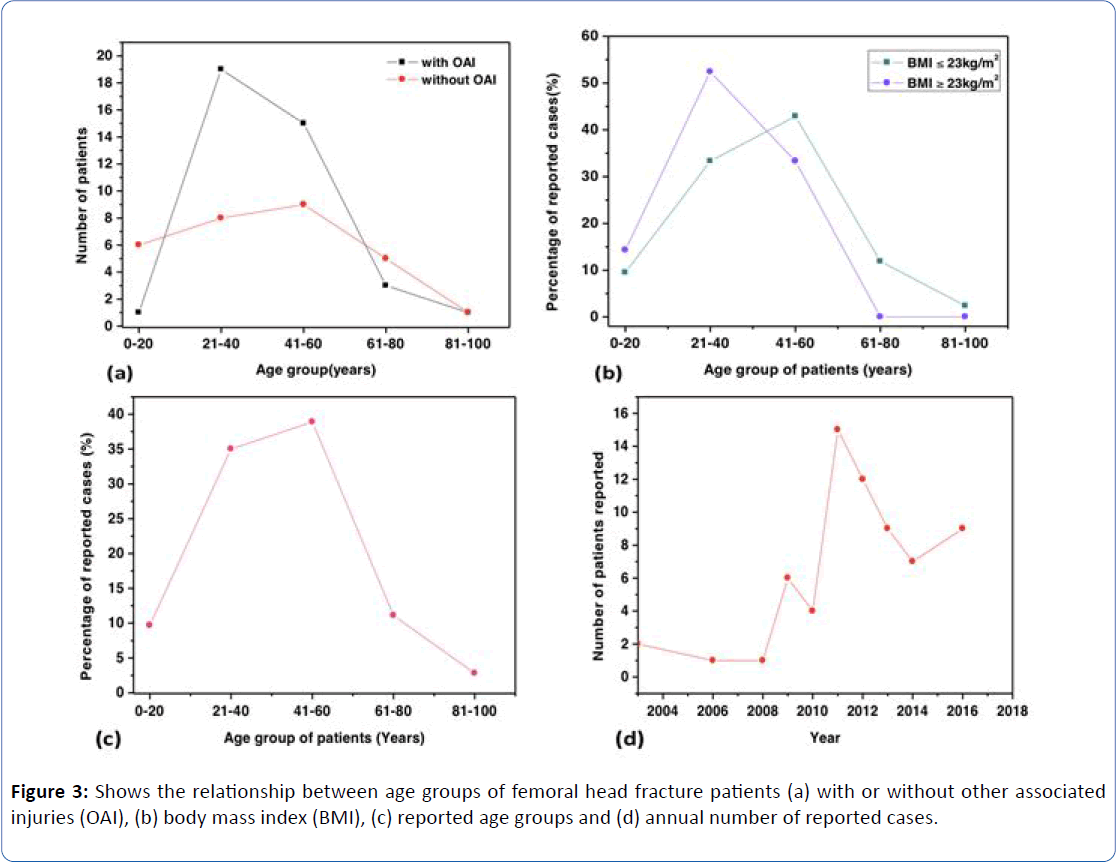
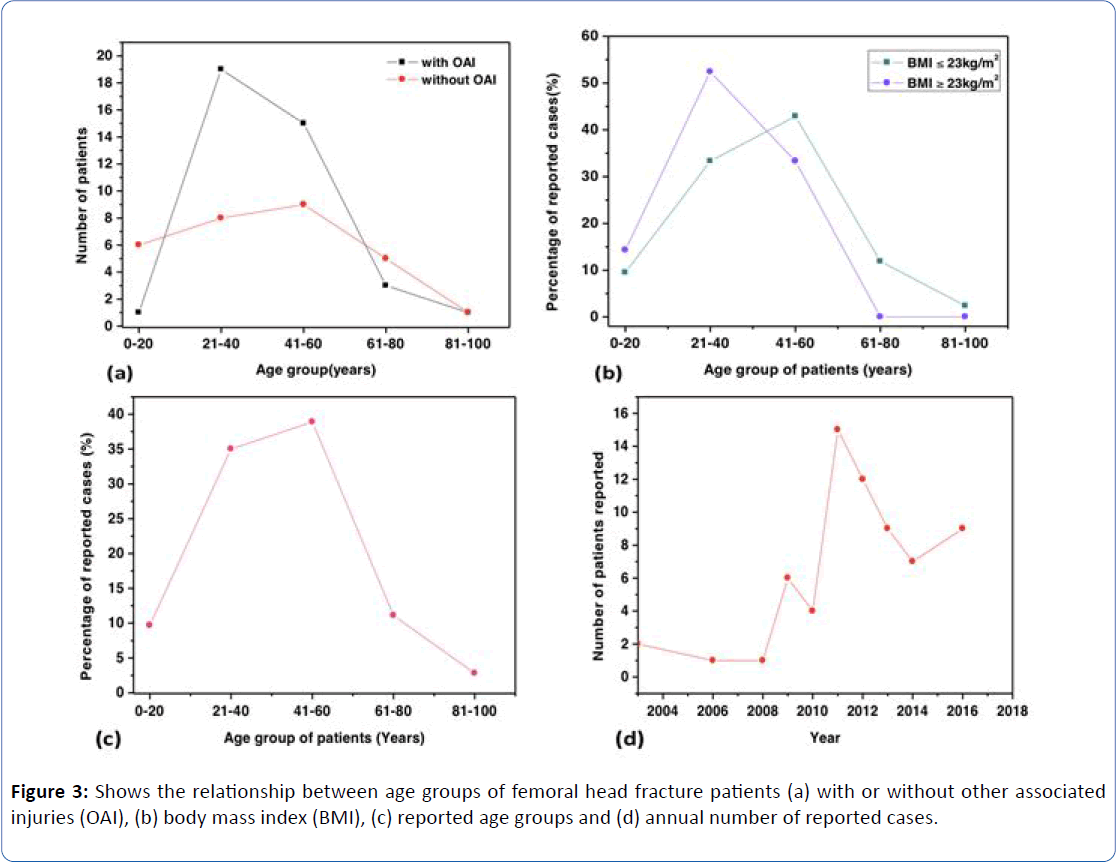
Figure 3: Shows the relationship between age groups of femoral head fracture patients (a) with or without other associated injuries (OAI), (b) body mass index (BMI), (c) reported age groups and (d) annual number of reported cases.
For statistical analysis using Chi-square test, the P value for the groups with and without AI for height was 0.872, weight was 0.055, Age was 0.217, Sex was 0.505 and location of FHF (right or left) was 0.081.
The level of significance is shown on Tables 2 and 3. The data indicates that taller patients (171 ± 5.5 cm) mostly suffered from Pipkin type II fractures, followed by type I (168 ± 7.2 cm), then closely by type IV (168.5 ± 7.8 cm) while type III fractures were mostly common in shorter patients (163.6 ± 8.0 cm). Furthermore, the average calculated weight for Pipkin type I was 60 ± 12.1 kg, type II 59.4 ± 18.0 kg, type III 49.1 ± 16.2 kg and type IV 69.1 ± 16.0 kg.
| Group (%) |
| Variables |
with OAI |
without OAI |
P value |
Comment |
| Age |
0.217 |
No association found |
| <50 years |
61.2 |
38.8 |
|
|
| >50 years |
45 |
55 |
| Sex |
0.505 |
No association found |
| Female |
20 |
80 |
|
|
| Male |
28.6 |
71.4 |
| Location of FHF |
0.083 |
No association found |
| Right leg |
70.3 |
29.7 |
|
|
| Left leg |
50 |
50 |
FHF: Femoral Head Fracture, OAI: Other Associated Injuries
Significance level was set at 5% (p<0.05) |
Table 2: Statistical assessment of age, sex and location of FHF (left and leg).
| Group (%) |
| Variables |
with OAI |
without OAI |
P value |
| Weight |
| <57 kg |
48 |
52 |
0.055 |
| 57 kg |
72.2 |
27.8 |
| Height |
| <167 cm |
72.2 |
27.8 |
0.872 |
| >167 cm |
72.3 |
25.7 |
| BMI |
| <23 kg/m2 |
53.8 |
46.2 |
0.024 |
| >23 kg/m2 |
84.2 |
15.8 |
BMI: Body Mass Index, OAI: Other Associated Injuries
Significance level was set at 5% (p<0.05) |
Table 3: Statistical data.
The data showed no association between occurrences of AI in FHF patients with regards to their height, weight, Age, Sex, and location of FHF respectively.
The P value for the association between BMI and the two groups (with and without AI) was 0.024 (P<0.05), showing a significant association. Meaning FHF patients with BMI less than 23 kg/m2 had higher chances of suffering from other related injuries.
Discussions
To our knowledge, this study is the first of its kind to assess the association of age, sex, fracture location, height, weight and BMI on FHF patients with or without other injuries acquired at time of accident. Our results suggest there is an association between the BMI of FHF patients and their injuries incurred during the time of accident. Patients with BMI less than 23 kg/m2 suffered more from injuries like hip fractures, head trauma, lower and upper limb injuries as well as those to the torso. Moreover, apart from having a longer accumulative length of stay in hospital, these patients also had averagely longer follow-up period of 15 months (1/2 month-122 months) compared to their counterparts with BMI more than 23 kg/m2 who had average follow-up of 13 months (1/2 month-45 months). However, we found no association of age, sex, weight and height with FHF injuries. The location of the FHF (left or right) was also neither a contributory factor.
Several studies have reported significant relationship of BMI on fracture injuries. Our results are consistent with several published reviews and meta-analysis which have concluded that there is an inverse association between BMI and fracture injuries [19-23]. A case-control study reported that a group of patients with significantly low BMI had more fractures occurring than the group without fracture [24]. Haakon and colleagues reported a lower BMI is important risk factor for fatal hip fractures [25] and a higher BMI was protective against subsequent hip fracture [26]. In a study by Kaze et al. an increase in BMI was associated with 15% reduction in vertebral fracture in men but not in women [27]. Obese women (classified by BMI) have been indicated to reduce hip fracture risks than their non-obese counterparts [28]. But it is worth mentioning that there are other authors who in contrast have reported that the risk of hip fracture increases with increasing BMI [29-32]. Overall, our study demonstrated a lower BMI increased the likelihood of other associated injuries.
Height which is a non-modifiable characteristic has been reported in several epidemiological studies to have potential risk factor for fracture. There has been the correlation of the geometric feature of the adult height with hip axis, angle of neck shaft and radius of femoral head [32]. It has also been argued that the center of gravity is higher in taller people than in shorter people and also the high risk due to reduced cortical thickness and bigger impact when falling caused possible heavier injuries [33-35]. Armstrong et al study in over 790,000 patients indicated that a proportionate increase of femoral neck fracture risk with increasing in height of 48% per 10 cm [35]. Furthermore, a meta-analysis by Xiao et al. also found a positive association between height and increased risk of hip fracture [36]. In contrast, this present study found no significant association of height with FHF. This could be because of the small population size due to the rare occurrence of FHF. However, it is important to note that when the height of the two groups with and without injury were analyzed, the two compared heights <167 cm and >167 cm had 72.2% and 72.3% reported cases of other associated injuries respectively. These indicated the taller and the shorter groups were equally affected and hence being tall or short was not a privilege against occurrences of other injuries.
When it comes to weight, it has been assumed that the overweight may have poorer balance which may increase risk of fall and therefore increasing risk of injury. The decrease in relative bone strength due to high ratio of weight to bone mass and bone area as well as a higher proportion of fat relative to muscle have been indicated in possible cause of fracture injuries. In our study groups however, when the weights were compared with having AI or not, there was a ratio of about 2:3 chances of injury for the lighter (<57 kg) and heavier (>57 kg) patients respectively. Pipkin classification was successfully used to classify all encountered fractures. For reported cases of FHF among the males and females (Figure 1b), type IV fracture was more common in men (35.0%) while type III was for the women (31.3%). Both females and males had similar reported cases of 20%-28.6% respectively for groups with other associated injuries. Hence, sex was not a protective factor against AI in FHF patients. When it came to the location of FHF, there was a 50%-50% reported cases of with and without AI for the left leg. The right leg however showed 70.3% of AI and 29.7% with no AI. This data adds to the sparse published works in this field of study.
It is interesting to note that the highest reported cases were found in 41-60 year group (Figure 3c). We have shown for the first time that FHF was more common among the middle ages (after young adulthood and before beginning of old age) than we traditionally thought was associated with the much younger patients. On the comparison with and without AI age groups, we found patients at 21-40 year group had more AI, this can be attributed to not just only the highly energy expenditure and physically active but also the increased exposure of the adult life to accidents. On the other hand, decline in number of cases was seen as the population ages (>60 years). This can be attributed to decreased physical activity in this age group that may decrease the level of exposure to injury and subsequently reduce risk of FHF.
Despite our finding on the relationship between BMI and associated injury in FHF patients, the exact mechanism of the association remains to be established. Several studies on BMI and injuries have made mention of possibilities like body fat mass distribution predicting bone mineral density [37], the influence of bone development and adult height intrauterine or childhood factors [38]. There has been also other implications of increased body mass in increasing bone mineral density that contribute to the integrity of bone structure [39], the protective value of obesity against fractures [40], effect of adipose tissue preservation on bone mineral density by endogenous estrogens [41] and their complex effects on bone quality, mass and strength. Robinovitch et al. have proposed that the state of the muscle activity at time of impact could be important in the risk of fracture by fall than the thickness of the hip soft tissue [42].
Our findings had limitations that deserve consideration. First is the standard limitation of any retrospective study. Second, the small patient numbers as FHF occurrence is very rear. And third, the quality of data was dependent on the completeness of patient history including the availability of medical images or radiographs for classification. A further prospective multicenter study setting would be helpful.
Conclusions
This manuscript thoroughly submerses the possible predictions for other injuries in FHF. We recommend for FHF patients with BMI <23 kg/m2 extra caution should be considered when investigating other accompanying injuries. Beside the clinical complications related to FHF, the association of BMI with injury is highly relevant to better understand the dynamics in this field. This finding has good implication for patients and the orthopedic community. The present evidence suggests that FHF is much common in the middle age group that we thought was for much younger patients.
Funding
This research received no funding.
Conflict of Interest
Ghamor-Amegavi Prince Edem, Pan Zhijun, Wu Jiaqi and Jiangjun Jiang declare that have no conflicts of interest.
23687
References
- Birkett J (1869) Description of a dislocation of the head femur com-plicated with its fracture, with remarks. Med Chir Trans 53: 133-188.
- Kelly PJ, Lipscomb PR (1958) Primary vitallium-moldarthroplasty for posterior dislocation of the hip with fracture of the femoral head. J Bone Joint Surg 40: 675-680.
- Marecek GS, Scolaro JA, Chip JB (2015) Management of syndesmotic disruption in ankle fractures: A critical analysis review. JBJS Reviews 23: 2.
- Tonettia J, Ruattia S, Lafontanb V, Loubignacc J, Chironb P, et al. (2010) Is femoral head fracture-dislocation management improvable: A retrospective study in 110 cases. Orthopaedics & Traumatology, Surgery & Research OTSR 96: 623-631.
- Philipp H, Peter K, Klaus AS (2007) Femoral head injuries: Which treatment strategy can be recommended? J Injury 1: 23.
- Daubigne RM, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36: 451-475.
- Stockenhuber N, Schweighofer F, Seibert FJ (1994) Diagnosis, therapy and prognosis of Pipkin fractures (femur head dislocation fractures). Chirurg 65: 976-981.
- Epstein HC, Wiss DA, Cozen L (1985) Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res 201: 9-17
- Schonweiss T, Wagner S, Mayr E, Ruter A (1999) Late results after fracture of the femoral head. Unfallchirurg 102: 776-783.
- Panigrahi R, Mahapatra AK, Palo N, Priyadarshi A (2015) Neglected PipkinÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¾ÃÂâs fracture dislocation with bilateral femoral shaft fractures: An unusual combination. JSCR 3: 1-5.
- Cooper C, Campion G, Melton LJ (1992) Hip fractures in the elderly: A worldwide projection. Osteoporos Int 2: 285-289.
- Gullberg B, Johnell O, Kanis JA (1997) Worldwide projections for hip fracture. Osteoporos Int 7: 407-413.
- Roeder LF, DeLee JC (1980) Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res 147: 121-130.
- Thompson VP, Epstein HC (1951) Traumatic dislocation of the hip: A survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg 33: 746-778.
- Butler JE (1981) Pipkin type-II fractures of the femoral head. J Bone Joint Surg Am 63: 1292-1296.
- Lang-Stevenson A, Getty CJM (1987) The Pipkin fracture-dislocation of the hip. Injury 18: 264-269.
- Epstein HC (1974) Posterior fracture-dislocations of the hip. Long-term follow-up. J Bone Joint Surg Am 56: 1103-1127.
- Armstrong JR (1948) Traumatic dislocation of the hip joint. J Bone Joint Surg Br 30: 430-445.
- Migliaccio S, Greco EA, Fornari R (2011) Is obesity in women protective against osteoporosis? Diabetes Metab Syndr Obes 4: 273-282.ÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂè
- De Laet C, Kanis JA, OdÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂén A (2005) Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos Int 16: 1330-1338.
- Johansson H, Kanis JA, OdÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂén A (2014) A meta-analysis of the association of fracture risk and body mass index in women.ÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂèJ Bone Miner Res 29: 223-233.
- Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 309: 71-82.
- Pagani RC, Kunz RE, Girardi R, Guerra M (2014) Body mass index as a prognostic factor for fracturing of the proximal extremity of the femur: A case-control study. Rev Bras Ortop 49: 461-467.
- Meyer E, Tverdal A, Falch A (1995) Body height, body mass index, and fatal hip fractures: 16 years' follow-up of 674,000 Norwegian women and men. Epidemiology 6: 299-305.
- Sogaard AJ, Holvik K, Omsland TK, Tell GS, Dahl C, et al. (2016) Age and sex differences in body mass index as a predictor of hip fracture: A NOREPOS study. Am J Epidemiol 184: 510-519.
- Kaze AD, Rosen HN, Paik JM (2018) A meta-analysis of the association between body mass index and risk of vertebral fracture. Osteoporos Int 29: 31-39.
- Compston JE, Watts NB, Chapurlat R, Cooper C, Boonen S, et al. (2011) Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med 124: 1043-1050.
- Liu B, Balkwill A, Banks E, Cooper C, Green J, et al. (2007) Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology 46: 861-867.
- Obesity: Preventing and managing the global epidemic (2000) WHO Technical Report Series 894, World Health Organization, Geneva.
- Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, et al. (2011) BMI and fracture risk in older men: The osteoporotic fractures in men study (MrOS). J Bone Miner Res 26: 496-502.
- Fini M, Salamanna F, Veronesi F, Torricelli P, Nicolini A, et al. Role of obesity, alcohol and smoking on bone health. Front Biosci 4: 2686-2706.
- Nissen N, Hauge EM, Abrahamsen J, Jensen JE, Mosekilde L, et al. (2005) Geometry of the proximal femur in relation to age and sex: A cross-sectional study in healthy adult Danes. Acta Radiol 46: 514-518.
- Bjornerem A, Bui Q, Ghasem-Zadeh A, Hopper J, Zebaze R, et al. (2013) Fracture risk and height: An association partly accounted for by cortical porosity of relatively thinner cortices. J Bone Miner Res 28: 2017-2026.
- Armstrong ME, Kirichek O, Cairns BJ, Green J, Reeves GK, et al. (2016) Relationship of height to siteÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂÃÂspecific fracture risk in postmenopausal women. J Bone Miner Res 31: 725-731.
- Xiao Z, Ren D, Feng W, Chen Y, Kan W, et al. (2016) Height and risk of hip fracture: A meta-analysis of prospective cohort studies. Biomed Res Int 2016: 2480693.
- Stevens J, Katz EG, Huxley RR (2010) Associations between gender, age and waist circumference. Eur J Clin Nutr 64: 6-15.
- Cooper C, Walker-Bone K, Arden N, Dennison E (2000) Novel insights into the pathogenesis of osteoporosis: The role of intrauterine programming. Rheumatology 39: 1312-1315.
- Hla MM, Davis JW, Ross PD, Wasnich RD, Yates AJ, et al. (1996) A multicenter study of the influence of fat and lean mass on bone mineral content: Evidence for differences in their relative influence at major fracture sites. Am J Clin Nutr 64: 354-360.
- Cunha DF, Cunha SFC, Piloto PE, Santos NP, Barros JW (1998) Estado ÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂènutricional e resposta de fase aguda em pacientes com fratura do terc ÃÂÃÂÃÂâÂÂÃÂâ¦â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂço proximal do fÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂêmur. Rev Bras Ortop 33: 321-234.
- Armstrong ME, Spencer EA, Cairns BJ, Banks E, Pirie K, et al. (2011) Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res 26: 1330-1338.
- Robinovitch SN, Hayes WC, McMahon TA (1991) Prediction of femoral impact forces in falls on the hip. J Biomech Eng 113: 366-374.