Merola J*, Jain A, Ziad F and Hussain Z
Neurosurgery Department, Waikato Hospital, Hamilton, New Zealand
*Corresponding Author:
Dr. Joseph Merola
Neurosurgery Department, Waikato Hospital, Hamilton, New Zealand, 3210
Tel: 02920814000
E-mail: merola.joe@gmail.com;merolaj@doctors.org.uk
Received date: May 27, 2016; Accepted date: June 21, 2016; Published date: June 24, 2016
Keywords
Calcified pseudoneoplasm of the neuraxis; CAPNON; Oedema; Brain stone
Case Report
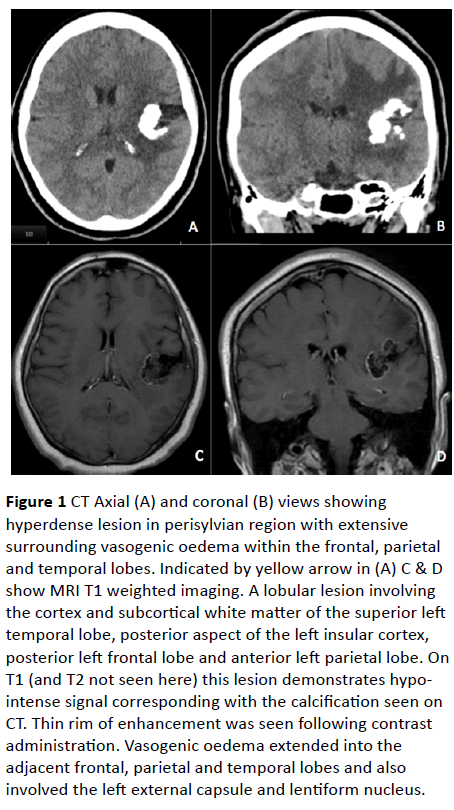
A 39-year-old, right hand dominant, female presented with tingling sensation in her right arm followed by a first-time, selfterminating generalized tonic-clonic seizure. There was no previous medical history and no regular medications. Detailed neurological examination was unremarkable and there were no signs elicited from cardiorespiratory or abdominal examination. Computed tomography (CT) of the brain revealed a hyper dense calcified mass in the left perisylvian region (Figure 1). Magnetic Resonance Imaging (MRI) showed hypointense signal on T1 and T2-weighted images in the region of calcification as seen on CT. Extensive vasogenic oedema was also noted in adjacent lobes and extended into the external capsule and lentiform nucleus. Prominent vessels were seen surrounding the lesion but no vascular anomaly was noted on Magnetic Resonance Angiography (MRA). A Digital Subtraction Angiogram (DSA) ruled out aneurysm or arterio-venous malformation (AVM). The differential diagnosis remained lowgrade astrocytoma versus oligodendroglioma.
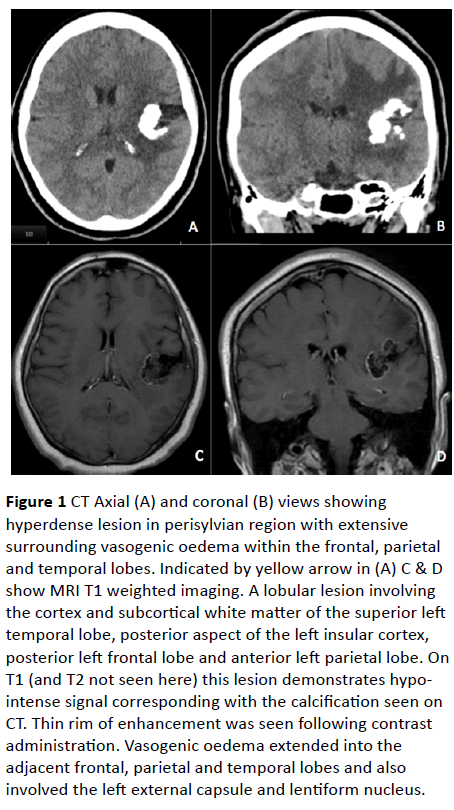
Figure 1: CT Axial (A) and coronal (B) views showing hyperdense lesion in perisylvian region with extensive surrounding vasogenic oedema within the frontal, parietal and temporal lobes. Indicated by yellow arrow in (A) C & D show MRI T1 weighted imaging. A lobular lesion involving the cortex and subcortical white matter of the superior left temporal lobe, posterior aspect of the left insular cortex, posterior left frontal lobe and anterior left parietal lobe. On T1 (and T2 not seen here) this lesion demonstrates hypointense signal corresponding with the calcification seen on CT. Thin rim of enhancement was seen following contrast administration. Vasogenic oedema extended into the adjacent frontal, parietal and temporal lobes and also involved the left external capsule and lentiform nucleus.
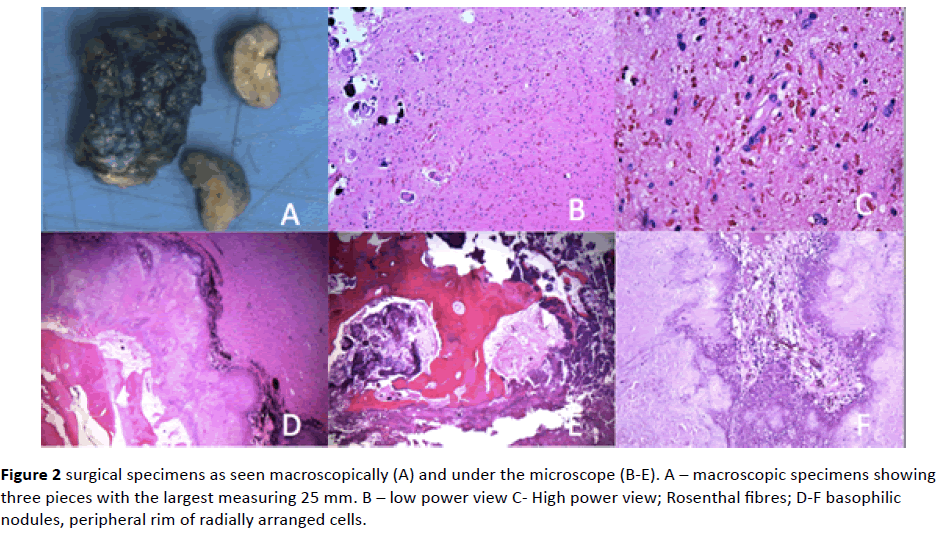
Following multidisciplinary discussion surgical intervention was recommended. The patient underwent a left frontotemporal craniotomy and gross total resection of the calcified mass. The sylvian fissure was noted to be wide open and surrounded by prominent vessels. The calcified mass was removed in three pieces and abnormal looking surrounding brain was biopsied; it had a rubbery consistency with greyyellow appearance. Post-operatively the patient was noted to be significantly weak in the right upper and lower limbs. MRI confirmed restricted diffusion in the parietal lobe. Histological diagnosis confirmed a calcified pseudoneoplasm of the neural axis (Figure 2).
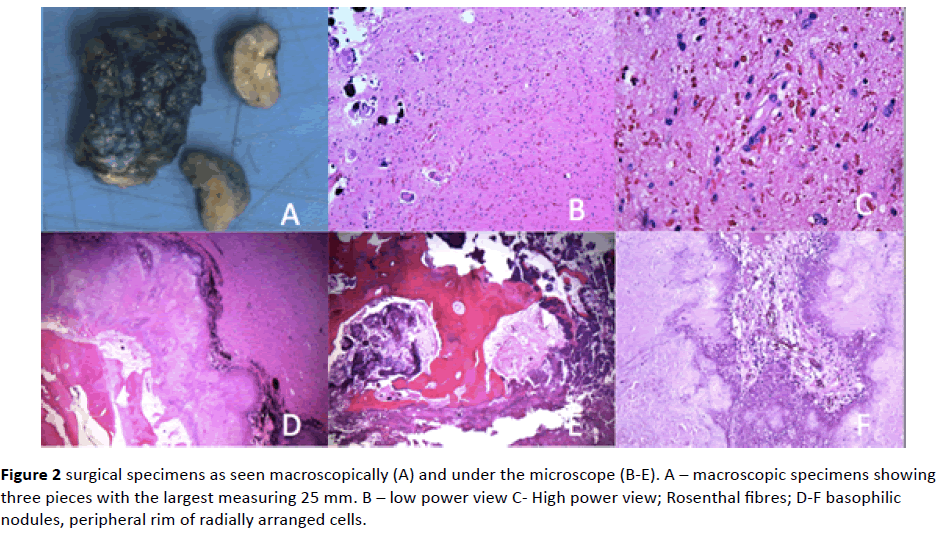
Figure 2: surgical specimens as seen macroscopically (A) and under the microscope (B-E). A – macroscopic specimens showing three pieces with the largest measuring 25 mm. B – low power view C- High power view; Rosenthal fibres; D-F basophilic nodules, peripheral rim of radially arranged cells.
At one month follow up the patient remained densely monoplegic in the right upper limb but now able to move antigravity in the right lower limb. She remained on anti-seizure medication and continued intensive Neuro-rehabilitation.
Discussion
Calcified pseudoneoplasm of the neuraxis (CAPNON) is a rare entity and is considered benign. Review of previous reports suggests similar incidence in both sexes occurring in different locations intra-and extra-axially [1]. To our knowledge none have previously been reported in the perisylvian region. Presentation varies depending on location but can involve, as seen in this case, sensorimotor deficit or seizures [2].
CAPNON is typically mistaken for more common neoplastic or non-neoplastic lesions and CT/MRI helps to distinguish between the different types. On CT, CAPNON is classically hyper dense given the calcification while on MRI imaging lesions tend to show hypo-intense signal on T1 and T2 weighted sequences [1]. Surrounding vasogenic oedema is not commonly reported and would not typically be expected from a benign lesion. Grabowski et al. reported vasogenic oedema in their case report and suggest seizures as the possible cause [2]. Similarly our patient presented with seizures although the cerebral oedema was more extensive.
Histologically CAPNON contains variable portions of fibrous stroma, bone, palisading spindle and epithelioid cells and a chondromyxoid-like matrix [1]. The etiology and natural history of CAPNON is unclear and thought to result from a reactive process. This is suggested by associated granulomatous inflammation typically surrounding the calcified mass [3].
Rodriguez et al. support this theory in their description of an unusual case of co-existing CAPNON and a low-grade cerebellar ependymoma associated with marked piloid gliosis on histology. The authors conclude that CAPNON is a result of tumefactive reaction rather than metaplasia [3]. The histological descriptions from our case are typical of those for CAPNON and are shown in Figure 2.
There is widespread acceptance that while surgical resection may provide symptom relief, histological diagnosis and prevention of recurrence, it does not come without risk. In our case there was significant postoperative right upper limb weakness as a result of infarction-postoperative MRI demonstrates an area of restricted diffusion extending postero-laterally from the surgical resection site to the left posterior parietal lobe.
Conclusion
CAPNON must be considered in the differential diagnosis of calcified lesions in the brain. The decision to proceed with surgical intervention must be influenced by the clinical presentation. The type of approach (e.g. biopsy versus total resection) should be discussed at a multidisciplinary level to mitigate the inherent risks of surgical intervention.
Conflicts of Interest
None declared
9773
References
- Aiken AH, Akgun H, Tihan T, Barbaro N, Glastonbury C (2009) Calcifying pseudoneoplasms of the neuraxis: CT, MR Imaging and Histologic features AJNR 30: 1256-1260.
- Grabowski M, Recinos P, Chen T, Prayson R, Vogelbaum M (2013) Calcifying pseudoneoplasm of the neuraxis overlying the corpus callosum: A case report and review of the literature Clinical Neuropathology 32: 515-521.
- Rodriguez FJ, Scheithauer BW, Fourney DR, Robinson CA (2008) Ependymoma and intraparenchymal calcifying pseudoneoplasm of the neural axis: Incidental collision or unique reactive phenomenon? ActaNeuropathol 115: 363-366.