Miry Achraf1*, Tiabi ElMehdi1, Malki Samia1, Rahou Fatima-Zahra2, Bennani Amal1 and Bouziane Mohamed2
1Pathology Department, Mohammed VI University Hospital, Oujda/60000, Morocco
2General Surgery Department, Mohammed VI University Hospital, Oujda/60000, Morocco
- Corresponding Author:
- Miry Achraf
Ph.D Scholar, Mohammed VI University Hospital, Morocco
Tel: +212671278817
E-mail: achrafmiry@outlook.com
Received Date: January 09, 2020; Accepted Date: January 25, 2020; Published Date: February 01, 2020
Citation: Miry A, Tiabli EM, malki S, Rahou F-Z, Bennani A (2020) Granular Cell Tumor: A Rare Entity of the Perianal Region. Arch Cancer Res. Vol.8 No.1:8 doi:10.36648/2254-6081.8.1.198
Copyright: © 2020 Miry A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Granular cell tumor; Gastro-intestine; Buccal Mucosa; Prognosis
Introduction
Granular cell tumor is a pathological entity that was first described by Abrikossof in 1926. Many locations were described. The most frequent one is the buccal mucosa especially on the tongue, dermis and subcutaneous tissue [1,2]. Granular cells tumor is rarely located in the perianal region [3]. Granular cell tumors often occur between the 4th and 6th decades with a male predominance that can reach up to 68% [4,5]. Although a malignant variant of this tumor exists, it barely presents 2% of all cases. The diagnosis of malignancy requires an accurate analysis of the histological feature and investigations in order to identify metastases [4,6]. The basic treatment is surgical excision with local recurrence being the only possible complication when the resection is incomplete [4,6]. In our work, we report the case of a granular cell tumor of the perianal region that was clinically taken for a squamous cell carcinoma. 6 months after surgery, the patient had a good evolution, without any sign of local recurrence. We also discuss the most important features of this entity.
Case Report
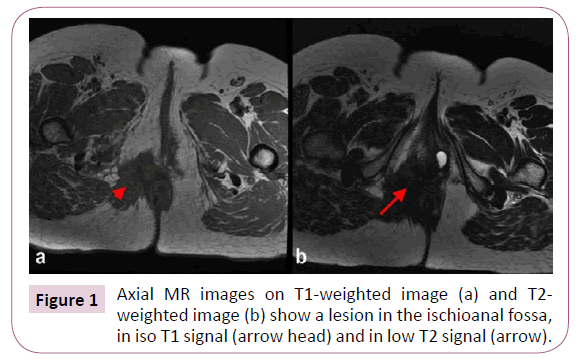
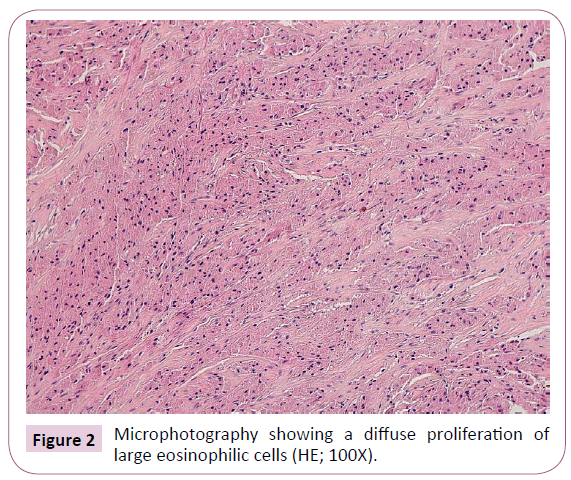
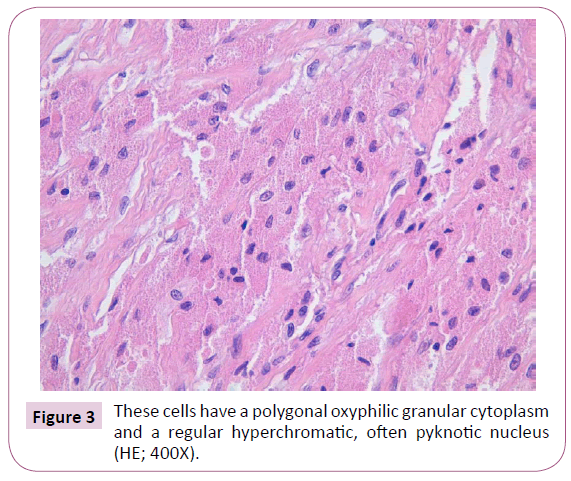
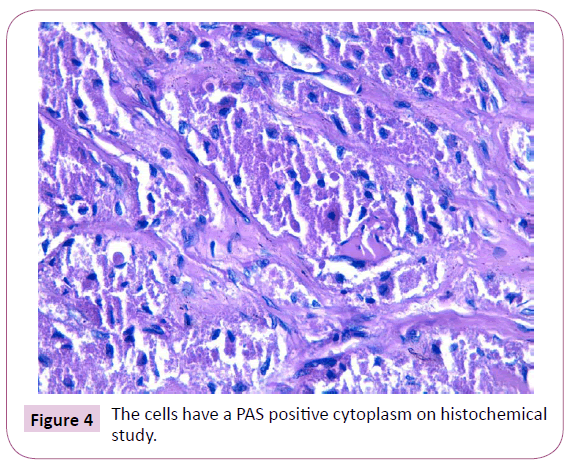
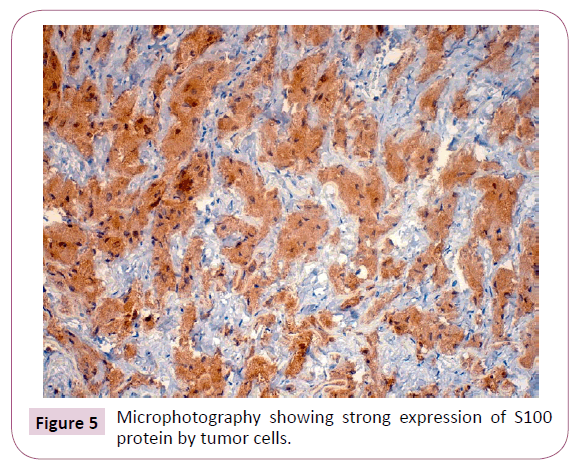
Our patient is a 52 years old female, married, with no clinical or surgical morbidities. No relevant family neoplastic history was found. She complained for about one year of perianal pain, without diarrhea, abnormal evacuations, rectal bleeding or fever. The patient has previously received anti-hemorrhoid therapy for more than 2 months without any improvement. She was then admitted in our hospital, where rectal examination has revealed a right perianal nodule without local inflammatory changes. No hemorrhoids or other lesions were identified. General examination of the patient was normal. We performed a pelvic MRI with contrast, which identified a lesion of the ischioanal fossa that appeared isointense on T1 weighted images and hypo intense on T2 weighted images (Figure 1). The lesion showed progressive and delayed enhancement on T1 weighted images with fat saturation with contrast. It was in an intimate contact with levator ani and gluteus maximus mascules. Other investigations included colonoscopy, laboratory tests and chest X ray and were found to be normal. An entire macroscopic surgical excision and the surrounding subcutaneous tissue under local anesthesia were performed. The used local anesthetic was Marcaine 25%, with a security marge of 0.5 cm around the mass. Pathological examination of the resection specimen, a 5,5x4,5x2cm of subcutaneous tissue, has revealed a diffuse proliferation of large cells. These cells have a polygonal oxyphilic granular cytoplasm and a regular hyperchromatic, often pyknotic nucleus. The tumoral stroma was essentially fibrous without an inflammatory infiltrate. No mitotic activity neither necrosis was observed. The proliferation locally invades skeletal muscle (Figures 2 and 3). The cells have a PAS + cytoplasm on histochemical study (Figure 4). On immunohistochemical study, tumor cells were positive to CD68 and S100 protein (Figure 5). 6 months after surgery, the patient had a good evolution, without any sign of local recurrence.
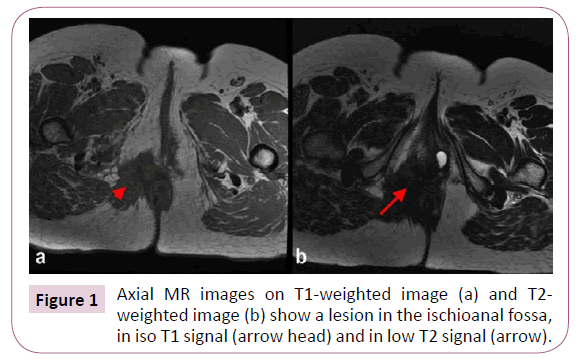
Figure 1: Axial MR images on T1-weighted image (a) and T2-weighted image (b) show a lesion in the ischioanal fossa, in iso T1 signal (arrow head) and in low T2 signal (arrow).
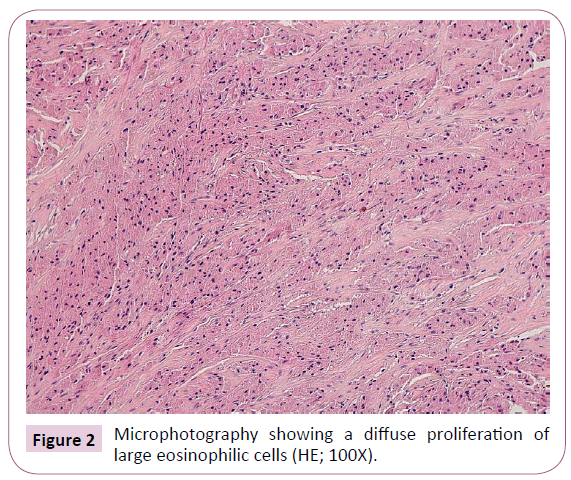
Figure 2: Microphotography showing a diffuse proliferation of large eosinophilic cells (HE; 100X).
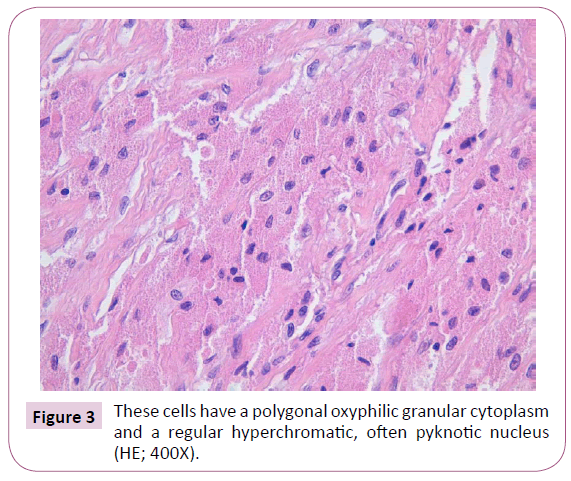
Figure 3: These cells have a polygonal oxyphilic granular cytoplasm and a regular hyperchromatic, often pyknotic nucleus (HE; 400X).
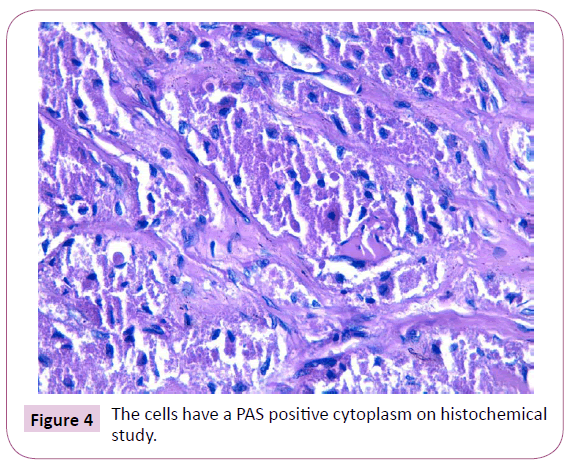
Figure 4: The cells have a PAS positive cytoplasm on histochemical study.
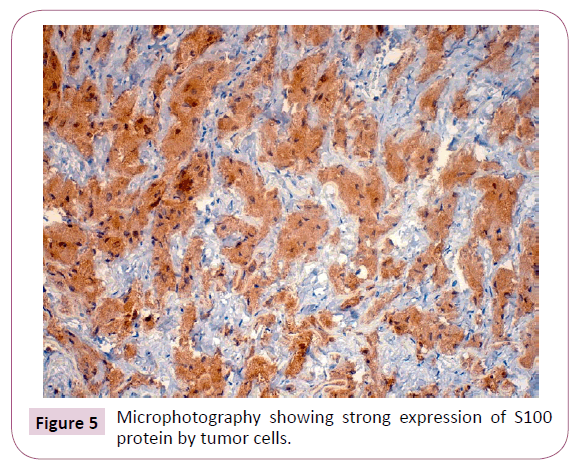
Figure 5: Microphotography showing strong expression of S100 protein by tumor cells.
Discussion
Granular cell tumor is a tumor that occurs especially on the buccal mucosa (Particularly on the tongue), the skin and subcutaneous tissue. Nevertheless, it can occur on any location [4,5]. In up to 8,5%, these tumors can occur in a multifocal fashion [4,5]. The diagnosis is most often obtained on resection specimen and rarely on biopsy specimens [4,5-7]. Granular cell tumors occur in the gastrointestinal tract in only 5 to 19% of all cases [4,5]. The largest series of granular cell tumors was reported by Lebranchu et al. He reported 263 cases, showing man predominance at about 68%, and among all cases, only one patient had a perianal location, whereas the others frequent locations were skin (38%), esophagus (19%) and tongue (10%). A high incidence rate in African descent patients were found in up to 29% of cases in a study done by Lack et al about 110 patients [4]. Most interestingly, at least in our case, the largest number of perianal location for this tumor was reported in a series of 74 cases of gastrointestinal granular cell tumors. This study has found only 48 patients to have a perianal location. The median patient’s age was of 39 years old for the gastrointestinal location [3].
In a 2016 review of literature made by Araújo et al. among 48 cases of recto-anal localized granular cell tumor, 40 had an anal/ perianal location [8]. Another case of peri-anal granular cell tumor was recently reported by Emily F Kelly et al. [9]. When this tumor is located on the perianal area, it manifests most often in form of a painful nodule as in the case reported in our work, although the identification of a nodule was possible only one year after the beginning of symptoms. Other reported symptoms include rectal bleeding and also incidental discovery of the tumor when its symptoms are hidden by those of other perianal pathologies such as hemorrhoids and perianal fissures [3,10]. On histopathological level, the granular cell tumor is non-capsulated and typically made of large granular eosinophilic cells [3]. The tumor cells are known to express the S-100 protein, neuron specific enolase (ENA) and CD-68, thus justifying a both neural and macrophage/histiocytic origin for this tumor, although it was initially thought to have a muscular origin [2,3,5]. The link to histiocytes/macrophage is more supported by morphological and structural features. Nevertheless, the histogenesis of granular cell tumors is not completely elucidated [11]. Main differential diagnosis include on the clinical level, abscess of the perianal region [3]. On pathological level, the positivity of tumor cells to S-100 protein is not specific and is therefore a reason to have in mind the different S-100 protein positive tumors, such as melanomas, neural tumors, histiocytosis and clear cells sarcoma. Granular cell tumor can also be confounded with squamous cell carcinoma since its frequent association to some degree of pseudoepitheliomatous epithelium hyperplasia [3,5]. Although granular cell tumors are almost all benign, a small proportion (2%) is malignant, with approximately 50 reported cases in the literature and three of them were reported on the anal/perianal area [2,11-14]. The diagnosis of malignancy is based on both histological features and the occurrence of distant metastasis. The histological features that favor malignancy are vesicular morphology of the nucleus, prominent nucleolus, spindle morphology of the tumor cells instead of epithelioid morphology and presence of necrosis or brisk mitotic activity [6]. Most frequent metastatic sites are lymph nodes and lung occurring respectively in 70% and 50% of cases. It is sometimes hard to differentiate between a benign and malignant Granular cell tumor [11]. When granular cell tumors are malignant, they frequently affect deep soft tissues, larynx, esophagus, peripheral nerves and peritoneal nerves. These tumors recur in up to 70% of the cases [6]. Compared to the malignant variant, benign granular cell tumors recur in proportions that are different depending on state of the surgical margins: from 2-8% when margins are negative to over 20% when margins are positive [12]. Surgical excision is the preferred diagnostic and therapeutic tool [4,5]. The diagnosis of malignant granular cell tumor justifies other investigations: Chest X rays, Bone scintigraphy, liver ultrasonography, thoracic, abdominal and pelvic CT scan [15]. There was no need for further investigations in our case since the tumor was having totally benign histological features.
Conclusion
In our work, we report a case of perianal granular cell tumor in a 52 years old female evolving during a period of one year. We also discuss the most important epidemiological, clinical, pathological, therapeutic and prognostic features of this rare entity.
Data Availability
Not applicable
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
26331
References
- Dupuis C, Coard KCM (2009) A review of granular cell tumors at the university hospital of the West Indies. West Indian Med J 58: 138- 41.
- Francesco VD, Avellini C, Pappalardo S, Proscia D, Piccirillo F (2010) Malignant granular cell tumor of the anal perianal region and suprarenal hyperplasia: a casual association? Indian J Dermatol 55: 403-5.
- Johnston MJ, Helwig EB (1981) Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Dig Dis Sci 26: 807-16.
- Lebranchu VB La (1999) tumeur à cellules granuleuses. ÃÂÃÂÃÂÃÂâÂÂÃÂâââÂÂìÃÂ
áÃÂÃÂââ¬Ã
¡ÃÂâââÂÂìÃÂðpidémiologie de 263 cas. Clin Exp Pathol 47: 26-30.
- Lack EE, Worsham GF, Callihan MD, Crawford BE, Chun B, et al. (1980) Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol 13: 301-16.
- Jardines L, Cheung L, LiVolsi V, Hendrickson S, Brooks JJ (1994) Malignant granular cell tumors: report of a case and review of the literature. Surgery 116: 49-54.
- Strong EW, McDivitt RW, Brashfield RD (1970) Granular cell myoblastoma. Cancer 25: 415- 522.
- Araújo, Angelo Fontes (2016) Granular cell tumor of anal border. J Coloproctology 36: 115- 118.
- Mourra N, Werbrouck A, Bauer P (2011) Anal region: an unusual location of granular cell tumour. Int J Colorectal Dis 26: 811-12.
- Le BH, Boyer PJ, Lewis JE, Kapadia SB (2004) Granular cell tumor: immunehistochemical assessment of inhibin-alpha, protein gene product 9.5, S100 protein, CD68, and Ki-67 proliferative index with clinical correlation. J Arch Pathol Lab Med 128: 771-75.
- Crowe D, Ayli EE, Gloster HM (2012) A malignant granular cell tumor excised with mohs micrographic surgery. Case Rep Oncol Med: 4535-569.
- Mnasri H, Bouchoucha S (2005) Granular cell tumor of the perianal region: which therapeutic attitude? J Acta Chir Belg 105: 112-13.
- Bouraoui S, Letaief H, Mestieri H, Chadly-Debbiche A, Ben Zineb S, et al. (1999) Malignant granular cell tumor. J Ann Pathol 19: 151-52.
- Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG (1998) Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol 22: 779-94.
- Tsuchida T, Okada K, Itoi E, Sato T, Sato K (1997) Intramuscular malignant granular cell tumor. J Skeletal Radiol 26: 116.