Sandra Vuignier, M.D.1; Takanori fukushima, M.D.2
Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan.
Department of Neurosurgery, Duke Raleigh Hospital and Carolina Neurosciences Institute, North Carolina, United States.
*Corresponding Author:
Sandra Vuignier
M.D,Sandra Vuignier, MD, Place du Gabon, 1971 Grimisuat, 08038563108
E-mail: sandravuignier@gmail.com
Key words
Cavernous malformation; optic pathways; visual loss; total resection
Introduction
Lesions in the suprasellar region can interfere with optic nerve functions. The most common lesions are pituitary adenoma, craniopharyngioma, meningioma, carotid aneurysm and optic and hypothalamic gliomas [1, 10, 12, 13, 19]. In addition many uncommon neoplastic and infiltrative diseases affect this area, including germinoma, lymphoma, leukemia, chordoma, metastasis, nasopharyngeal carcinoma, sarcoidosis and histiocytosis X. CM of the ON, OC and OT is a very rare cause of visual deficits. Our case is particular because of the unusual location of the tumor, the unusual presentation of unilateral sudden loss of vision and the first pediatric age case in a series of 50 cases of cerebral cavernomas. Here we describe the case with the clinical and radiological characteristics and review the literature about CMs in the ON, OC and OT.
Case report
History and Examination
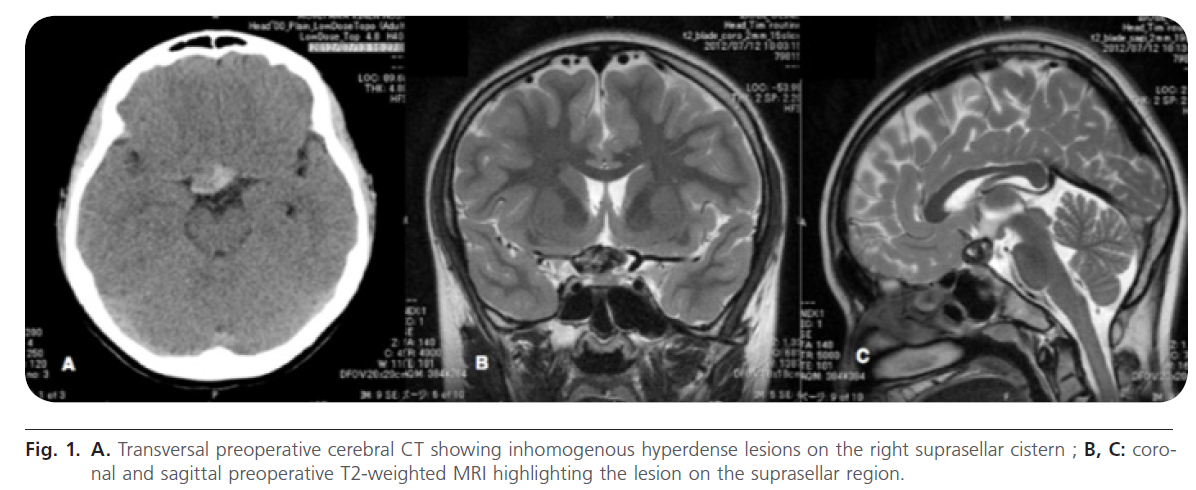
A 11-year-old male woke up with right dysopsia and headache. He went to a local eye clinic where left homonymous hemianopsia was highlighted. In the eye examination his right visual acuity was 0.03 and his left visual acuity was 1.2. Other neurological examinations showed no abnormalities and until that event the patient has always been healthy. There is no known family history of intracranial vascular malformations. Two days later he was sent to a local clinic where a cerebral CT and MRI were obtained that showed a heterogeneous mass lesion in the right suprasellar region (Fig. 1).
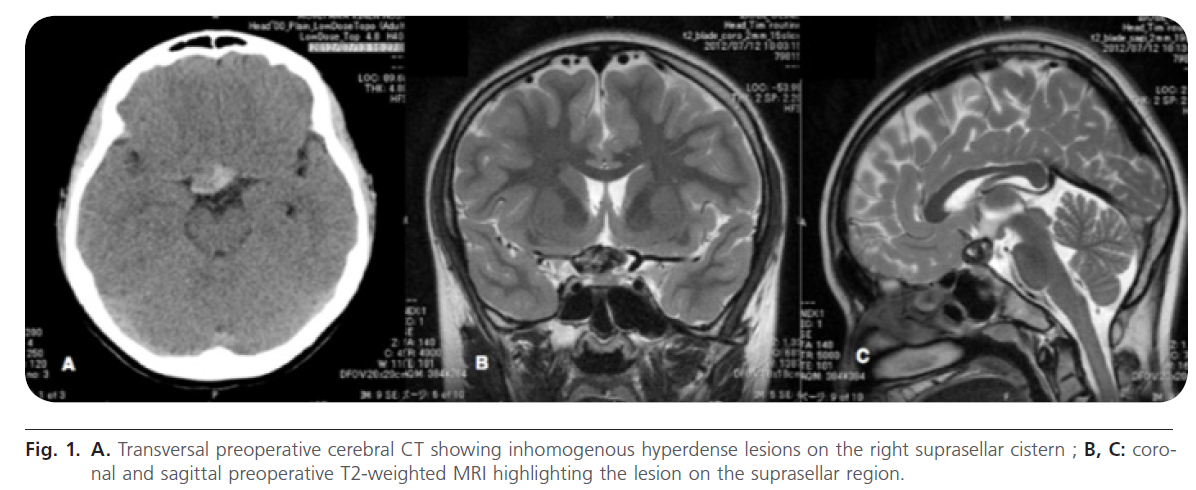
Figure 1: A. Transversal preoperative cerebral CT showing inhomogenous hyperdense lesions on the right suprasellar cistern ; B, C: coronal and sagittal preoperative T2-weighted MRI highlighting the lesion on the suprasellar region.
At that time optic glioma, craniopharyngioma and germinoma were suspected. He was therefore referred to our hospital for surgical management. We clarified the risks and the benefits of the surgery by explaining that decompression of the right ON is necessary because of the risks of permanent blindness by compression of the mass lesion. Moreover the pathological diagnosis is essential and can only be made if the surgery is performed. The patient and his family accepted the surgery.
Surgery
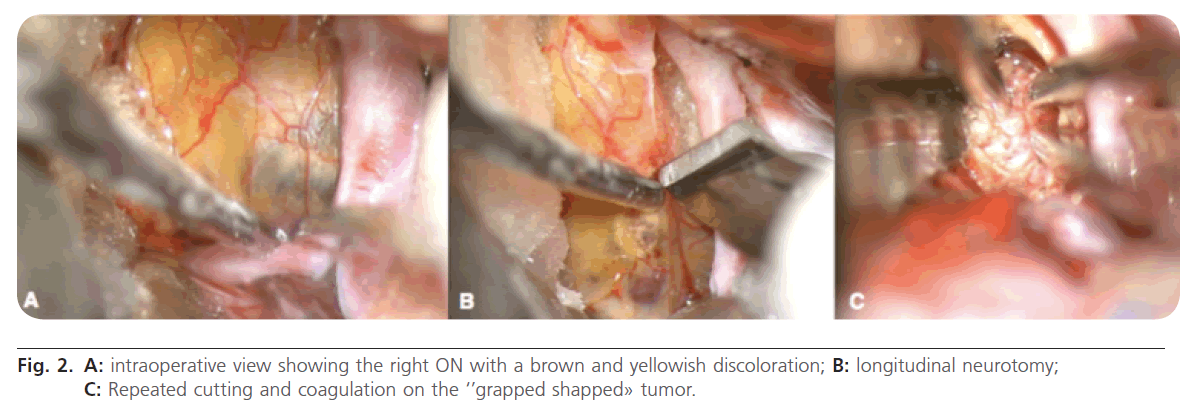
Operation was perfomed using a typical right semicoronal skin incision and a frontotemporal craniotomy. Meticulous dissection of the sylvian fissure from distal to proximal was done. The right middle cerebral artery (MCA), the internal carotid (IC) , the ON, OC and OT were exposed. The right ON, OC and OT appeared with a brown and yellowish discoloration (Fig. 2).
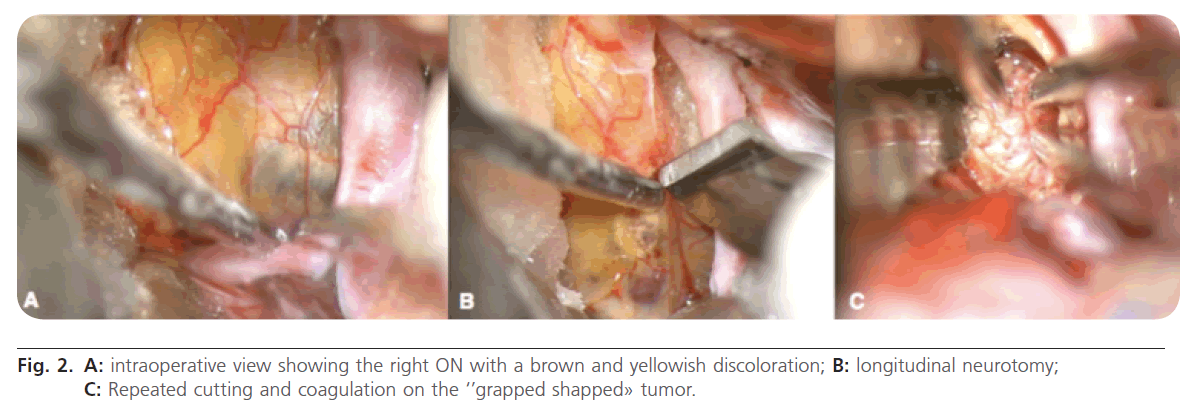
Figure 2: A: intraoperative view showing the right ON with a brown and yellowish discoloration; B: longitudinal neurotomy; C: Repeated cutting and coagulation on the ‘’grapped shapped» tumor.
The lesion consisted in «grapped shaped’’ vessels that were suggestive of a CM. Later we could confirm the CM by pathologist’s exmaination. The first step of the decompression consisted in the relaxation of the right ON by the resection of the falciform ligament. Secondly, a longitudinal neurotomy on the most discolored part was carried out along ON fibers allowing us to approach the cavity of the angioma. With precautious dissection around the tissues and repeated cutting and coagulation we could remove the lesion totally. Finally duralplasty was done with galeal tissue and the bone flap was repositionned in a cosmetic manner using Fixsorb plates. Skin closure was done in layers and a subdural drain was placed to help ensure that all of the blood products are removed.
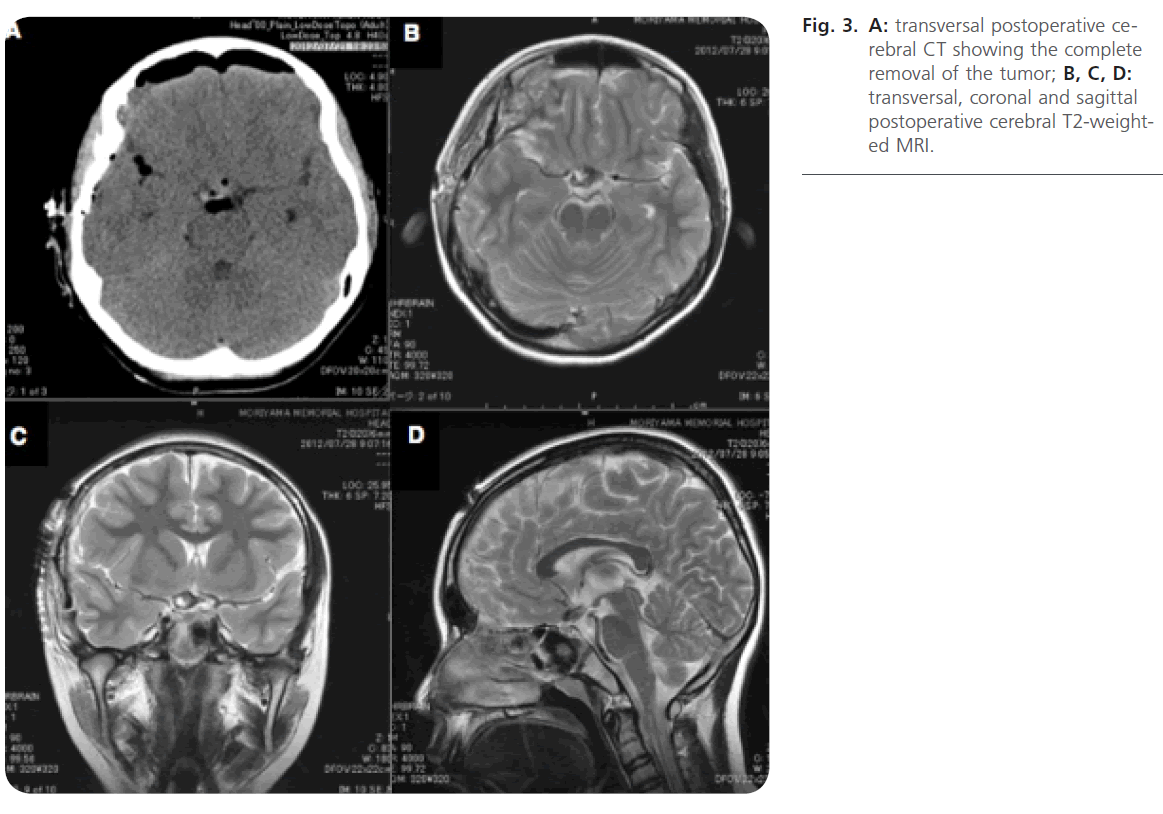
Postoperative courseThe postoperative course was uneventful with a dramatic improvement in the right vision. Left homonymous hemianopsia stayed stable. The postoperative cerebral CT and MRI showed total removal of the tumor (Fig. 3).
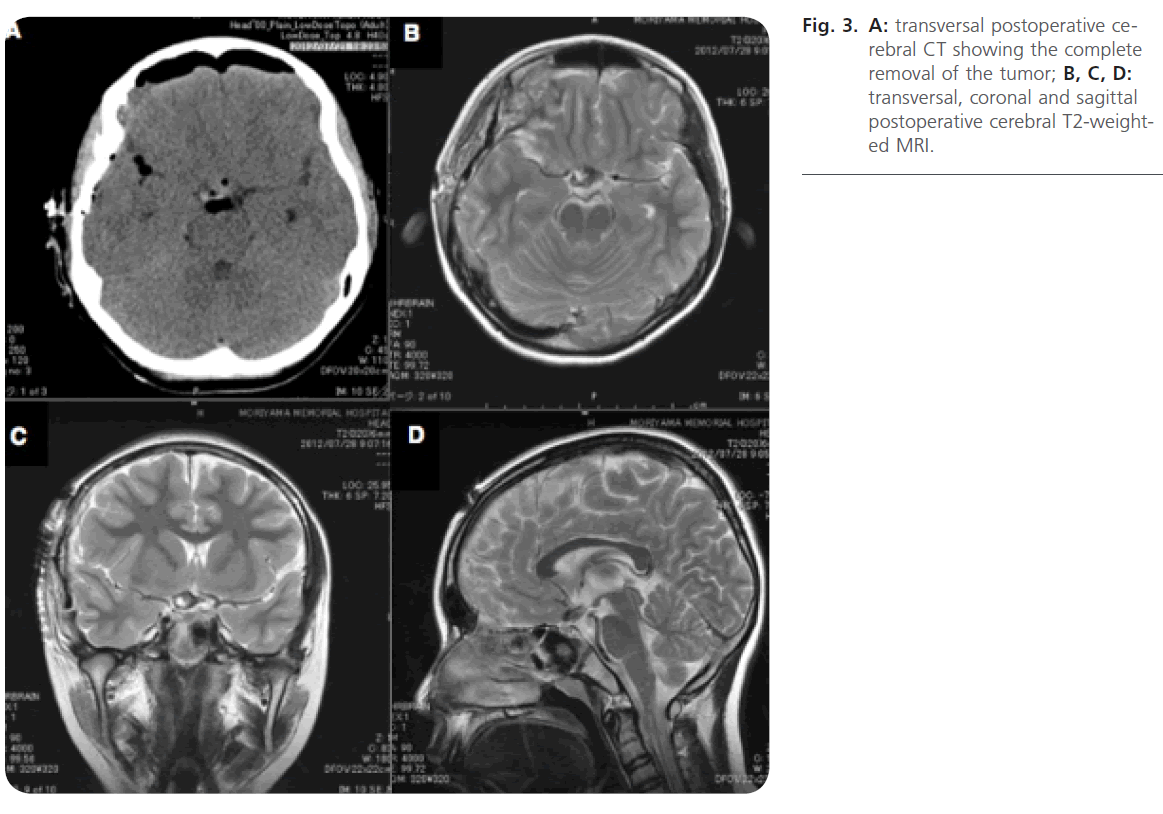
Figure 3: A: transversal postoperative cerebral CT showing the complete removal of the tumor; B, C, D: transversal, coronal and sagittal postoperative cerebral T2-weighted MRI.
After 9 days the patient was discharged and able to go back to daily life activities.
Discussion
CMs are benign lesions consisting of clusters of thin-walled immature veins [4, 18]. They occur with an incidence of 0.3 to 0.5% and constitue 10 to 20% of all vascular malformations including arterioveinous malformations, veinous malformations and capillary telangectasis [11, 15]. Unike the arterioveinous malformations, CMs have low flow and are angiographically occlut [2, 4]. These lesions may be observed in either sporadic or familiar form [1,2]. Clinical manifestations of such tumors lie mainly in the 3rd and 4th decade [16]. Most lesions occur in the supratentorial compartment (80%) followed by infratentorial lesions (15%) and lesions within the spinal cord (5%) [5].
CMs arising from the anterior optic pathways are rare [1, 4, 12, 18]. In the literature we inventoried 60 cases reported by Liu J.K. et al in a study analysis of 65 cases of CM in the optic pathways and the hypothalamus [8]. 46% lied in the left side of the brain, 44% in the right side and 10% extended to both side. Only 2 cases (5%) involved the OC, ON and OT on the right hemisphere, as in our case. One case is from [20]. He descrived a case of a 43-year-old male with subacute visual loss who underwent surgery with gross total resection. The outcome nevertheless worsened. The other case is from Manz et al. [20]. He reported the case of a 30-year-old male with acute visual loss and headache who underwent a biopsy. The outcome improved.
There is no doubt that our case is rare. The unilateral sudden loss of vision, the excellent outcome after total removal as well as the young age make this case unique.
Conclusion
CMs involving the optic pathways are very rare, so the diagnosis may be difficult. A rapid mangement decision is essential to avoid permanent blindness. Microsurgerical resection is the only one curative management and may provide functional improvement. During surgical excision, the gliotic interspace between the vascular malformation and the surrounding neural tissue provides a plane of cleavage for dissection which permits total excision without causing new deficits. Complete removal of the lesion is essential because of the possibility of recurrence [2-3, 6-7, 12, 14, 17]. This current case emphasises the importance of a rapid diagnosis and surgery of an anterior visual pathaway CM. The boy arrived nearly blind and was discharged after 9 days with righ vision much better improved and could return to his daily life activities.
Aknowledge
The author wants to thank Dr Fukushima for giving her the case.
Conflict of interest
The author declares that they have no conflict of interest.
2106
References
- Christoforidis, GA., Bourekas, EC., Baujan, M., Drevelangas, A., Tzalonikou, M. Neuroradiology case of the day. AJR Am J. Roentgenol 2000; 175: 888-890.
- Deshmukh, VR., Albuquerque, FC., Zabramski, JM., Spetzler, RF. Surgerical management of cavernous malformations involving the cranial nerves. Neurosurgery 2003; 53: 352-357.
- Ercan, O., Orhan, K., Kemal, Y., Serafettin, C. Optochiasmatic Cavernous Angioma. Neurol Med Chir. 2007; 47: 128-131.
- Newman, H., Nevo, M., Constantini, S., Maimon, S., Kesler, A. Chiasmal Cavernoma: A rare cause of acute visual loss imporved by prompt surgery. Pediatric Neurosurgery 2008; 44: 414-417.
- Hassler, W., Zentner, J., Wilhelm, H. Cavernous angiomas of the anterior visual pathways. J Clin Neuroophthalmol 1989; 9: 160-164.
- Hempelmann, RG., Mater, E., Schröder, F., Schön, R. Complete resection of a cavernous haemangioma of the optic nerve, the chiasm, and the optic tract. Acta Neurochir. 2007; 149: 699-703.
- Lehner, M., Fellner, FA., Wurm, G. Cavernous haemangiomas of the anterior visual pathways. Short review on occasion of an exceptional case. Acta Neurochir. 2006; 148: 571-578.
- Liu, J.K., Lu, Y., Raslan, A., Gultekin, S.H., Delashaw, J.B. Cavernous malformations of the optic pathway and hypothalamus: Analysis of 65 cases in the literature. Neurosurg Focus 2010; 29.
- Manz, HJ., Klein, LH., Fermaglich, J., Kattah, J., Luessenhop, AJ. Cavernous hemangioma of optic chiasm, optic nerves, and right optic tract. Virchows Arch A Pathol Anat Histol. 1979; 383: 225-231.
- Maruoka, N., Yamakawa, Y., Shimauchi, M. Cavernous hemangioma of the optic nerve. Case report. J Neurosurg 1988; 69: 292-294.
- Moriarity, JL., Wetzel, M., Clatterbuck, RE., Javedan, S., Sheppard, JM., Hoenig-Rigamonti, K. et al. The natural history of cavernous malformations: A prospective study of 68 patients. Neurosurgery 1999; 44: 1166-1173.
- Muta, D., Nishi, T., Koga, K., Yamashiro, S., Fujioka, S., Kuratsu, JI. Cavernous malformation of the optic chiasm: Case report. Br J Neurosurg 2006; 20: 312-315.
- Ozer, E., Kalemci, O., Yücesoy, K., Canda, S. Optochiasmatic cavernous angioma: Unexpected diagnosis. Case report. Neurol Med Chir. 2007; 47: 128-131.
- Pollock, BE., Garces, YI., Stafford, SL., Foote, RL., Schomberg, PJ., Link, MJ. Stereotactic radiosurgery for cavernous malformations. J Neurosurg. 2000; 93: 987-991.
- Porter, RW., Detwiler, PW., Spetzler, RF., Lawton, MT., Baskin, JJ., Derksen, PT. et al. Cavernous malformations of the brainstem: Experience with 100 patients. J Neurosurg. 1999; 90: 50-58.
- Robinson, JR., Awad, IA., Little, JR. Natural history of the cavernous angioma. J Neurosurg. 1991; 75: 709-714.
- Son, DW., Lee, SW., Choi, CH. Cavernous malformation of the optic chiasm: Case report. J Korean Neurosurg Soc. 2008; 44: 88-90.
- Werner, H., Zentner, J., Peterson, D. Cavernous Angioma of the Optic Nerve, case report. Surg Neurol. 1989; 31: 444-447.
- Wilms, G., Lammens, M., Marchal, G., Van Calenbergh, F., Plets, C., Van Fraeyenhoven, L. et al. Thickening of dura surrounding meningiomas: MR features. J Comput Assist Tomogr. 1989; 13: 763- 768.
- Yoshimoto, T., Suzuki, J. Radical surgery on cavernous angioma of the brainstem. Surg Neurol. 1986; 26: 72-78.