Andi Muhammad Ichsan1,2*, Linda Minar Herawati1, Anastasia Vanny1, Junely Vimala Jaury1, Habibah Setyawati Muhiddin2 and Budu2
1Department of Ophthalmology, Siloam Hospitals Makassar, Indonesia
2Faculty of Medicine, Department of Ophthalmology, Hasanuddin University, Kota Makassar, Sulawesi Selatan, Indonesia
*Corresponding Author:
Andi Muhammad Ichsan
Department of Ophthalmology, Siloam Hospitals Makassar, Indonesia
Tel: (+62) 81342280880
E-mail: am_ichsan@yahoo.com
Received: March 28, 2018; Accepted: April 04, 2018; Published: April 07, 2018
Citation: Ichsan AM, Herawati LM, Vanny A, Jaury JV, Muhiddin HS, et al. (2018) Central Retinal Artery Occlusion and Partial Ophthalmoplegia Caused by Hyaluronic Acid Injection Filler Cosmetic. Ann Clin Lab Res Vol.6: No.1: 230. doi: 10.21767/2386-5180.1000230
Keywords
Central retinal artery occlusion; Hyaluronic acid filler; Partial ophthalmoplegia
Introduction
Central retina artery occlusion (CRAO) is a very rare condition that happens in 1.9/100000 in the United States [1,2]. This event is sudden and devastating that leads to visual acuity from counting fingers or less [3,4]. Although autologous fat injection is considered safe, retinal artery occlusion in young healthy patients has been reported after this procedure [1,3]. In addition to autologous fat, the most popular fillers for cosmetic surgery are composed of partially cross-linked hyaluronic acid. Most cases of cosmetic facial fillers injection associated central retinal artery occlusion resulted blindness in the affected eye [1-9].
In this report we present a sudden visual loss and partial ophthalmoplegia just after injection of the hyaluronic acid filler.
Case Report
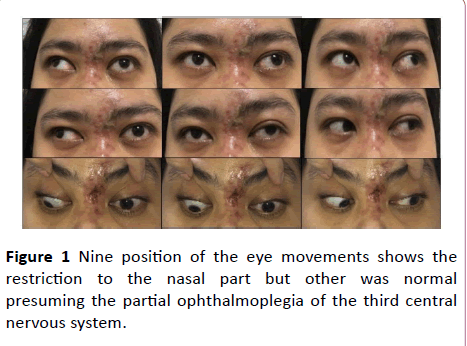
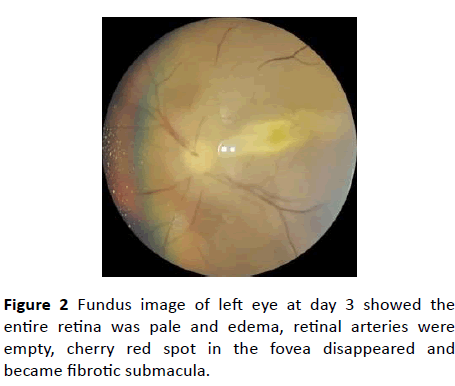
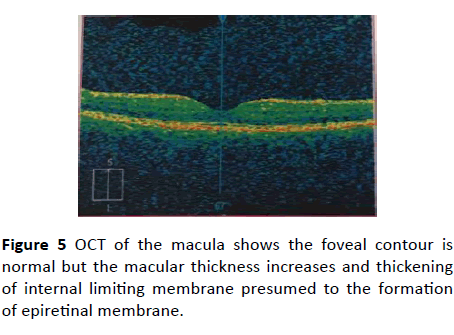
A 30-year-old young woman complained sudden visual loss at her left eye after being injected by 0.2 ml hyaluronic acid at the dorsum nasal area as filler cosmetic. It accompanied with headache and vomitus. There was no history of trauma, hypertension and other systemic diseases. Ophthalmological examination revealed light perception visual acuity at the affected eye, and 20/100 uncorrected visual acuity at the fellow eye. Restriction of the eye movement to the nasal was also observed (Figure 1). Anterior segment and intraocular pressure were normal. Funduscopic examination at the left eye revealed a total retinal edema with a cherry red spot at the fovea (Figure 2).
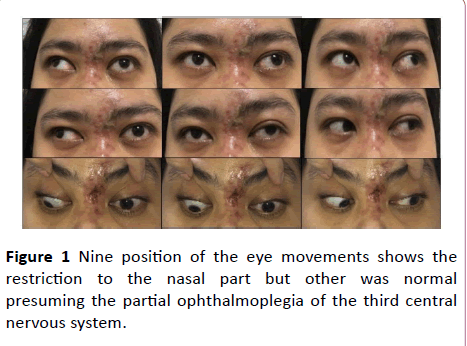
Figure 1: Nine position of the eye movements shows the restriction to the nasal part but other was normal presuming the partial ophthalmoplegia of the third central nervous system.
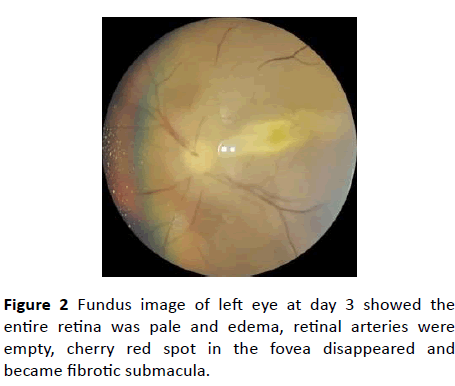
Figure 2: Fundus image of left eye at day 3 showed the entire retina was pale and edema, retinal arteries were empty, cherry red spot in the fovea disappeared and became fibrotic submacula.
Based on the history taking and ophthalmological examination, a clinical diagnosis of central retinal artery occlusion was established. An immediate ocular massage had done and then the patient urgently transferred to the operating theatre for aqueous humour paracentesis. The procedure of paracentesis was done in 90 minutes after initial onset using a-27 Gauge with 1 ml syringe inserted to the anterior chamber above the iris, radially away from the lens to avoid iatrogenic traumatic cataract, then amount of 0.3 ml of the aqueous humor was aspirated until the eyeball became hypotonic.
This patient was consulted to the internist to rule out for any systemic causes, but the laboratory findings were normal.
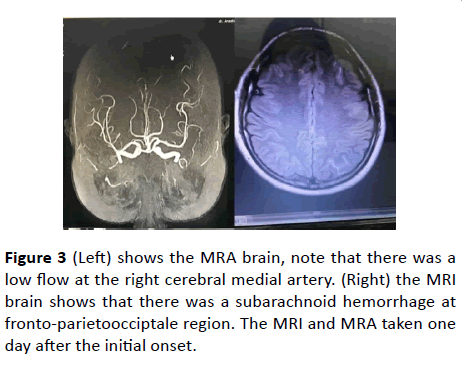
Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the brain revealed subarachnoid hemorrhage in the left frontoparieto-occipitale then conservative treatment by neurologist including citicholine 500 mg twice daily, methycobalt for once daily, tranexamic acid for three times a day were given (Figure 3).
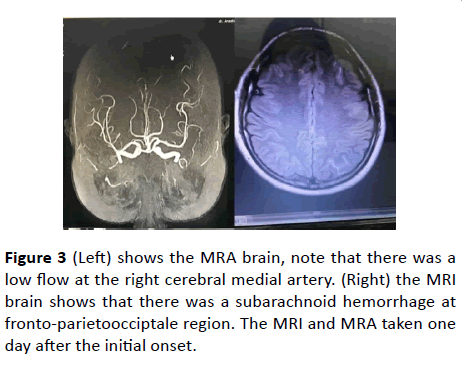
Figure 3: (Left) shows the MRA brain, note that there was a low flow at the right cerebral medial artery. (Right) the MRI brain shows that there was a subarachnoid hemorrhage at fronto-parietoocciptale region. The MRI and MRA taken one day after the initial onset.
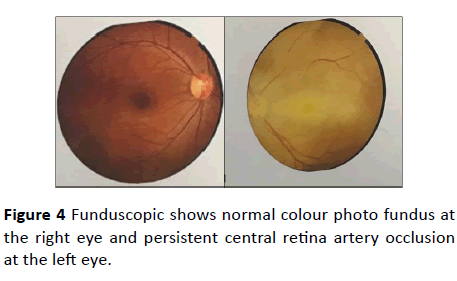
Six days after admitted visual acuity was improved to hand motion. The retina at the left eye seems more reddish and there was a pulsation in it. The optical coherence tomography (OCT) showed that there was a total edema at the macula. After approximately less than a month, the ophthalmoplegia has been improved. There is no restriction of the eye movement to the nasal region. (Figures 4 and 5)
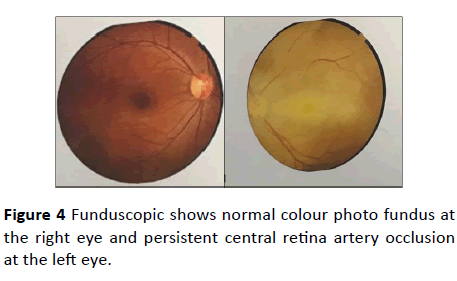
Figure 4: Funduscopic shows normal colour photo fundus at the right eye and persistent central retina artery occlusion at the left eye.
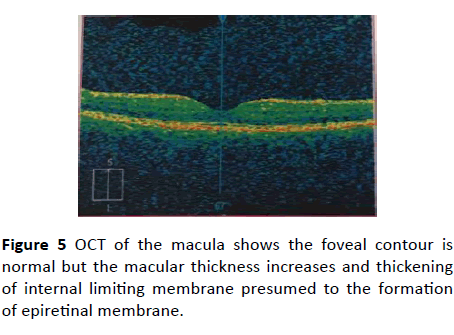
Figure 5: OCT of the macula shows the foveal contour is normal but the macular thickness increases and thickening of internal limiting membrane presumed to the formation of epiretinal membrane.
Discussion
Central Retinal Artery Occlusion (CRAO) was first described by Von Graeves in 1859. It is an analogue of acute stroke of the eye and is an ocular emergency [1,2,6]. Blindness and ophthalmoplegia following facial filler injections were the focus of this case report. Globally at least 50 cases of blindness after aesthetic facial injection has been reported [3,7] Cohen reported vascular complications are fortunately rare, about 0.001% of all performed dermal filler treatment.
The worldwide use of dermal filler for rejuvenation and facial reshaping is showing an increase over the last decade. Hyaluronic acid (HA) fillers are the most commonly used fillers, accounting for 78.3% of all filler treatments. HA is a fundamental component of extracellular matrix of cells, glycosaminoglycan. When injected into tissues, HA can provide structure and elasticity by binding collagen and elastin. This is the primary reason for its popularity in use, biocompability and reversibility. In this case 0.2 ml of hyaluronic acid HA were injected at dorsum nasal area as a filler cosmetic.
The vascularization of the face and the eye are highly complex [5]. The main sources of the orbita supply itself is ophthalmic artery which arise from the first branch of the internal carotid artery [1,4,5]. Some various anatomy of the ophthalmic artery can arise from the middle meningeal artery [5]. The supratrochlear, supraorbital, dorsal nasal artery and angular artery of the nose are distal branches of the ophthalmic artery [1,4,5]. The anastomosis of the dorsal nasal arteries with the ophthalmic arteries occurs at the medial canthus and from here blood can access the central retinal arteries via the ophthalmic arteries. The ophthalmic artery is a branch of the internal carotid, and turn supplies its orbital group, consisting of central retinal arteries. Excess pressure on the plunger during injection of fillers can overcome the anastomosis between facial and ocular circulation and reflux through to ophthalmic artery or its branches. Resulting ischaemia of the ophthalmic artery by blockage with dermal filler leading to lack of blood supply of any branches that it supplies can cause ophthalmoplegia, blepharoptosis and loss of vision. In this case sudden vision loss and partial ophthalmoplegia were found.
Coleman SR, believe that sharp, small cannulas, and also needles are much more likely to perforate the wall of an artery and then enter the artery itself causing the emboli and can travel retrograde to the ophthalmic artery and following systolic pressure the material may be removed and pushed distally along the ophthalmic artery itself in to central retina artery or any area supplied by internal carotid artery [10]. There all could cause blindness [1].
Our case reported that CRAO was found in a 30-year-old woman, Transatit et al, Considering the incidence of ocular complications however, there does seem to be a weighting towards complications in younger individuals, all subjects documented with vision loss because of HA filler treatment were under the age of 45. It is thought that younger individuals may be at increased risk of ocular complications due to an increased number of patent cutaneous arterial anastomoses. Large facial cutaneous arteries can be cannulated easily in filler treatment. When pressure is exerted on the plunger, and this is sufficient to cause retrograde flow, the ophthalmic artery can be reached from augmentation sites in nose and nasolabial areas.
Though many authors say that retrograde emboli could cause the problem of CRAO, Vos JA et al says that anterograde thromboembolism could also cause the problem of CRAO that related to major vascular procedures such as carotid artery stenting or cerebral aneurysm coil embolization. They are all could cause blindness [1-6]. Other researchers have reported that ophthalmophlegia, pain, skin necrosis at the injected area, ptosis and corneal edema could be the symptoms [4]. Park et al, 2012, linked occlusion of the ophthalmic artery to severe pain, whereas central retinal artery occlusion and branch retinal artery occlusion can present without pain. It appears that the smaller the vessel occluded, the less pain results due to less tissue supplied. In this case CRAO was present with sudden vision loss with ocular pain.
The funduscopic findings reported a cherry-red spot (90%), macular edema, and pale retina [1-7]. Based on the history and ophthalmologic examination, diagnosis was made for central retina artery occlusion caused by hyaluronic acid filler injection.
Some authors believe that there is a 60 to 120- minute window period to dissolve the filler material within the artery before the irreparable of visual loss [4,6,9,10]. The patient was immediately given the ocular massage, anterior chamber paracentesis, and then carbon dioxide-oxygen therapy. There was no systemic intervention in this patient. The patient was consulted to internist but had no treatment and laboratory findings were normal.
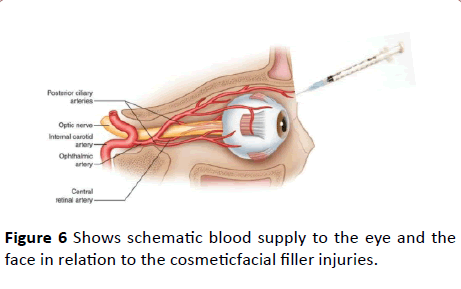
Conservative treatment by neurologist using citicholine, methycobalt and tranexamic acid were given based on MRI and MRA findings. After six days hospitalization, her visual acuity improved to hand motion. Figure 6 shows schematic blood supply to the eye and the face in relation to the cosmeticfacial filler injuries
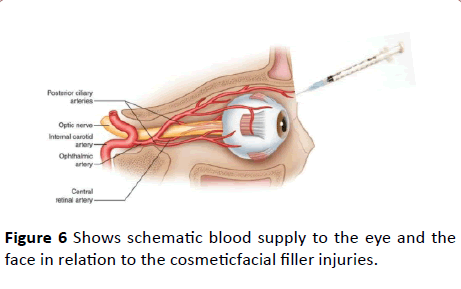
Figure 6: Shows schematic blood supply to the eye and the face in relation to the cosmeticfacial filler injuries.
Once CRAO existed, even the ocular massage and humor aqueous paracentesishad done in golden period but the visual loss can’t be recovered. Occlusion due to HA cannot be dislodged by its properties which expand and fill the lumen of artery even though its already dilated. In this case, CRAO due to hyaluronic acid has a worse prognosis than CRAO due to cholesterol thrombus [11-15].
Conclusion
In summary, our case illustrates a presentation of a visual loss and partial ophthalmophlegia after being injected by hyaluronic acid filler cosmetics. It is important to the physician to know the sign and symptoms, and immediate and proper treatment because it seems that “time is issue” in this case.
Central retinal artery occlusion can occur after hyaluronic acid injection filler cosmetics. Sudden vision loss and ophthalmoplegia can be the comorbid symptoms. Careful attention should be taken and always be aware of severe complications following this procedure.
22349
References
- Varma DD, Cugati S, Lee AW, Chen CS (2013) A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond) 27: 688-697.
- Cugati S, Varma DD, Chen CS, Lee AW (2013) Treatments option for central retina artery occlusion. Curr Treat Options Neurol 15: 63-77.
- Park SW, Woo SJ, Park KH, Huh JW, Jung C, et al. (2012) Iatrogenic retinal artery occlusion caused by cosmetic facial fillers injection. Am J Ophthalmol 154: 653-656.
- Lin YC, Chen WC, Liao WC, Hsia TC (2015) Central retinal artery occlusion and brain infarctions after nasal filler. QJM 108: 731-732.
- Li X, Du L, Lu J (2015) A Novell Hypothesis of visual loss secondary to cosmetic facial filler injection. Ann Plast Surg 75: 258-260.
- Loh KT, Chua JJ, Lee HM, Lim JT, Chuah G, et al. (2016) Prevention and management of vision loss relating to facial filler injections. Singapore Med J 57: 438-443.
- Townsend A (2016) Blindness after facial injection. J Clin Aesthet Dermatol 9: E5-E7.
- Carle MV, Roe R, Novack R, Boyer DS (2014) Cosmetic Facial Fillers and severe vision loss. JAMA Ophthalmol. 132:637- 639.
- Lazzeri D, Agonstini T, Figus M, Nardi M, Pantaloni M (2012) Blindness following cosmetic injections of the face. Plast Reconstr Surg 129: 995-1012.
- Coleman SR (2002) Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J. 22: 555-557.
- Hueston JT, Heinze JB (1974) A second case of relief blindness occurring after blepharoplasty. Case Report. Plast Reconstr Surg. 53: 430-431.
- Park SH, Sun HJ, Choi KS (2008) Sudden unilateral visual loss after autologous fat injection into nasolabial fold. Clin Ophthalmology. 2: 679-683.
- Peter S, Mennel S (2006) Retinal branch artery occlusion following injection of hyaluronic acid. Clin experiment Ophthalmology 34: 363-364.
- Cohen JL, Biesman BS, Dayan SH, DeLorenzi C, Lambros VS, et al. (2015) Treatment of Hyaluronic acid filler-induced impending necrosis with hyaluronidase: Consensus recommendations. Aesthet Surg Journal. 35: 844-849
- Tansatit T, Moon HJ, Apinuntrum P, Phetudom T (2015) Verification of embolic channel causing blindness following filler injection. Aesthetic Plast Surg. 39: 154-161.