Keywords
Cervical arthroplasty, cervical herniated disc, M6-C artificial disc
Abbreviations
UHWMPE: Ultra High Molecular Polyethylene; TPS: Titanium Plasma Spray
Introduction
During the past half century, there were an enormous number of advances in the treatment of cervical disc disease with cervical fusion. With the use of anterior cervical implants, fusion rates have surpassed 95% [1-3]. Limitations in the range of motion and adjacent segment degeneration are the major problems in the long-term clinical course of anterior cervical fusion.
Repeat surgical intervention is necessary for 2.9% of patients per year for symptomatic adjacent segment disease after anterior cervical decompression and fusion [4]. 25% of the patients reported symptoms from adjacent segment disease 10 years after anterior cervical decompression and fusion was performed [4,5]. Radiographic evidence of adjacent segment degenerative disc disease 5 years after surgery was been demonstrated in 92% of fused patients [6]. Cervical disc replacement and anterior cervical fusion are both safe procedures with a low incidence of significant adverse events related to the procedure [7,8].
Cervical disc arthroplasty could theoretically be beneficial to patients because it may avoid the incidence of adjacent segment disease by reducing the shear strains that occur at levels adjacent to anterior cervical fusions [5] and maintaining normal neck mobility [9]. Long-term prospective follow-up studies of cervical arthroplasty could reveal the benefits of motion preservation on adjacent segment degeneration.
Cervical Arthroplasty
In the past decades several new generations of artificial discs were created. The Cervical Spine Study Group developed a new nomenclature system for cervical arthroplasty [10]. Currently, artificial discs can be classified as nonarticulating, uniarticulating, or biarticulating. The artificial disc may consist of a metal on metal design, a metal on polymer design, such as polyurethane or ultra-high-molecular-weight polyethylene, a ceramic on polymer design, or a ceramic on ceramic design.
Discs are either modular, meaning that they have replaceable components, or they are non-modular, meaning that they have non-replaceable components. Some discs have supplemental vertebral body screw fixation, whereas others do not. Certain artificial disc designs promote biological bone ingrowth at the disc-endplate interface. Artificial discs may be constrained, semi constrained, or unconstrained in terms of motion.
Consequently, artificial discs may be categorized by the following criteria: articulation, material, design, fixation, and kinematics [11].
The M6-C artificial disc
The M6-C artificial disc is the first of non-fusion motion preservation products intended to replicate the anatomic and biomechanical attributes of a natural intervertebral disc. The M6 is the only artificial disc that mimics the natural disc’s design by incorporating an artificial nucleus and annulus into both its cervical and lumbar platforms.
The M6-C artificial disc is designed to replicate the anatomic structure and biomechanical performance of a natural disc. Its innovative design incorporates an artificial nucleus to allow axial compression and a woven fiber annulus for controlled range of motion in all 6 degrees of freedom.
The M6-C artificial disc contains a nucleus of viscoelastic polymer designed to simulate native nucleus and allows physiologic axial compression. It is retained between endplates and fiber annulus matrix and designed to enable a physiologic center of rotation.
The annulus consists of an ultra high molecular polyethylene (UHWMPE) fiber material which is intended to simulate native annulus and its performance. It provides controlled physiologic motion in all planes and axes. The robust fiber matrix with multiple layers is similar to native annulus. In addition, it contains a sheath which minimizes tissue in-growth and debris migration and allows for full range of motion.
However, to maintain its implanted position, the M6-C artificial disc uses a low profile tri-keel design rail of titanium to provide initial friction against migration of the implant and a titanium plasma spray (TPS) coating on its superior and inferior endplates to allow bony in-growth from the vertebral endplates onto the device (Figure 1).

Figure 1: The M6-C artificial disc uses a low profile tri-keel design rail of titanium to provide initial friction against migration of the implant and a titanium plasma spray (TPS) coating on its superior and inferior endplates to allow bony in growth from the vertebral endplates onto the device (Photos by courtesy of spinal kinetics).
The current concept of this cervical arthroplasty device has reached a high degree of safety and reliability. We present our technique for anterior cervical arthroplasty with the new M6-C device.
Indications and preoperative considerations
Patients with cervical radiculopathy secondary to disc herniations who have failed conservative therapies are potential candidates for anterior cervical arthroplasty [12,13].
Cervical arthroplasty only replaces the disc and requires intact and functional posterior elements, such as the facets and ligaments. Patients with degenerative cervical spondylosis, cervical spondylolisthesis with incompetent facets, severe osteoporosis, or cervical trauma are excluded from this procedure [10]. Therefore, patient selection is the most important step.
The implant might be overstrained and migrate because of abnormal local shear strains for patients with incompetent cervical facets, with spondylolisthesis and trauma, or with increased range of motion beyond normal anatomic constraints [11,14].
Patients with severe degenerative spondylosis or ankylosis are unlikely to experience the benefits of arthroplasty because their baseline cervical range of motion is very limited [11].
The implant could break through the weakened vertebral endplates in patients with osteoporosis.
The body habitus of the patient play an important role in intraoperative fluoroscopic visualization of the appropriate cervical level, which is necessary for precise implant placement. Patients with high standing shoulders and a short neck should be considered in being nominated for the M6 artificial disc.
Patient Positioning
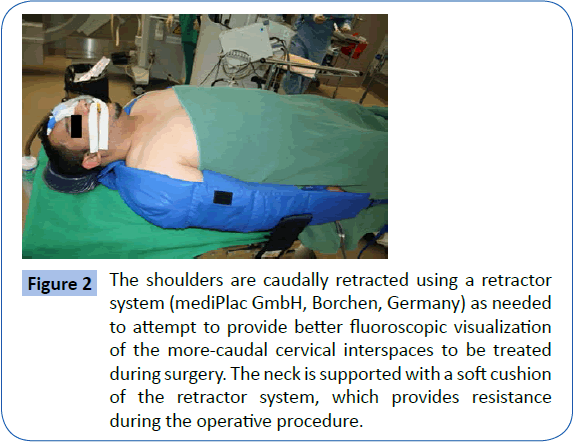
The M6-C artificial disc device is designed to be placed in a neutral cervical spine. For an appropriate placement of the implant the patient is positioned supine and the neck is extended and supported dorsally with a roll to position the neck in a neutral position. The shoulders are caudally retracted to help with intraoperative fluoroscopic visualization. We pull down on the shoulders and pull the arms in a caudal direction, toward the caudal end of the bed, using a retractor system (mediPlac GmbH, Borchen, Germany) as needed to attempt to provide better fluoroscopic visualization of the more-caudal cervical interspaces to be treated during surgery (Figure 2). The neck is supported with a soft cushion of the retractor system, which provides resistance during the operative procedure. Take care to avoid injury to the forearms, peripheral nerves, vasculature, wrists, and hands!
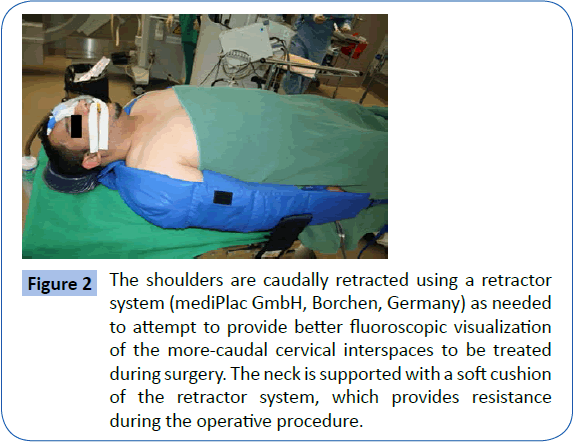
Figure 2: The shoulders are caudally retracted using a retractor system (mediPlac GmbH, Borchen, Germany) as needed to attempt to provide better fluoroscopic visualization of the more-caudal cervical interspaces to be treated during surgery. The neck is supported with a soft cushion of the retractor system, which provides resistance during the operative procedure.
Patients are administered a prophylactic antibiotic before starting surgery depending on the patient’s weight.
Operating Room Setup
The patient is positioned with the surgeon standing to the patient’s right side. The surgeon can choose a right or left sided approach. Habitually we prefer a right-sided skin incision. The endotracheal tube is placed in the left side of the mouth. The C-arm fluoroscope is positioned to obtain lateral and anteroposterior cervical X-ray views and is constantly in position during the operation.
Surgical Technique
An anterior cervical approach through a transverse right-sided incision is performed. For one- or two-interspace procedures, a skin incision is made in a skin fold in the right neck, centered over the anterior border of the sternocleidomastoid muscle, at the level of intended surgery, as confirmed by intraoperative fluoroscopy. A skin incision is made and an avascular dissection plane is developed between the esophagus/trachea, medially, and the sternocleidomastoid/carotid sheath, laterally. Hand held retractors might be utilized to provide initial exposure of the anterior vertebral column and the adjacent longus colli muscles.
The neurovascular bundles, the superior laryngeal nerve, and/or the recurrent laryngeal nerve, with associated vasculature, are preserved. Bipolar cautery is used to dissect the medial aspects of the longus colli musculature off of the ventral surfaces of the vertebral bodies. After the standard anterior cervical exposure is performed, we obtain a localizing fluoroscopic x-ray to identify and confirm the levels of intended arthroplasty. After localization of the appropriate levels, a self-retaining anterior cervical graphite retractor (Synthes GmbH, Solothurn, Switzerland) is placed under the elevated edges of the longus colli muscles. The monitoring of endotracheal tube cuff pressure and release after retractor placement may prevent injury to the recurrent laryngeal nerve during anterior cervical spine surgery [15].
We have to orient ourselves to the anatomic midline of the vertebral bodies and the lateral margins of the dissection. The goal, of course, is to place the implant exactly in the midline. On the other hand, we should avoid inappropriate, too-far lateral dissection to one side and inadequate decompression to the opposite side. Make certain that the curved lateral margins of the uncovertebral joints bilaterally identified so that too far laterally dissecting is avoided, increasing the subsequent risk of either vertebral artery injury, venous plexus bleeding, and/or nerve root injury.
Distraction posts are placed in the vertebral body above and below the interspace to enlarge the disc space. The use of anteroposterior intraoperative fluoroscopy can help during this step of the procedure to orient to the anatomical midline of the vertebral body.
These posts must be placed relatively high in the superior vertebral body and in the mid-portion of the inferior vertebral body and angled parallel to the superior plane of the superior endplate of the vertebral body in which they are inserted. This allows an unrestricted view past the posts and the distraction device and enough space to insert the implant.
Microsurgical rongeurs, curettes and kerrisons may be used to remove the disc material and cartilage to expose the posterior longitudinal ligament. We use the operating microscope to remove degenerative disc material at each interspace. The posterior longitudinal ligament is then removed to allow access to the cervical canal.
This procedure allows the canal to be completely decompressed. The dissection is performed laterally and bilaterally, to be sure that a thorough bony decompression has been accomplished and that both neuroforamen (and underlying nerve roots) have been decompressed. Intraoperative fluoroscopy allows us to confirm not only the level but the adequacy of the decompression. Contrast medium can be placed into the interspace to be certain that adequate bony decompression has been accomplished.
If the disc space has significant spondylotic changes, kerrisons may be used to remove the disc and osteophytes. The use of high-speed drilling of spondylotic changes carries the risk of bone dust particle which may cause heterotopic ossification and an early ossification surrounding the implant and therefore, should be avoided.
Implantation of the M6-C artificial disc
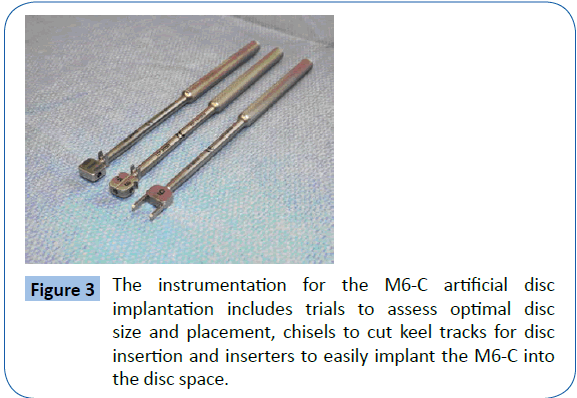
The M6 surgical instrumentation system was designed with surgeon feedback for simple, safe, and reproducible implantation of the M6-C cervical disc.
The instrumentation for the M6-C artificial disc implantation includes trials to assess optimal disc size and placement, chisels to cut keel tracks for disc insertion and inserters to easily implant the M6-C into the disc space (Figure 3).
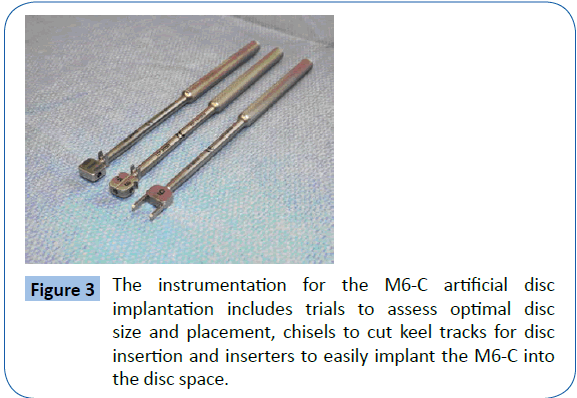
Figure 3: The instrumentation for the M6-C artificial disc implantation includes trials to assess optimal disc size and placement, chisels to cut keel tracks for disc insertion and inserters to easily implant the M6-C into the disc space.
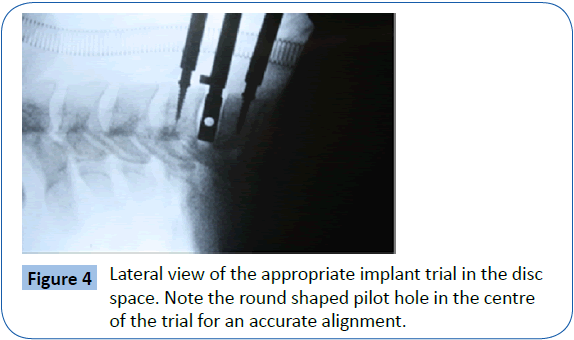
The appropriate implant trial is then placed into the disc space to confirm the size of the artificial disc that will be placed later (Figure 4). To accommodate the various anatomical ranges, the M6-C artificial cervical disc is available in 2 heights and 4 different sizes of endplate footprints.
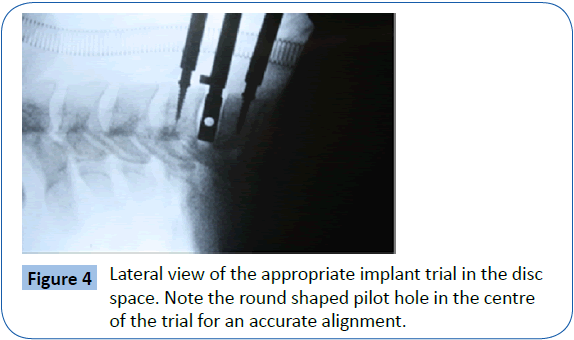
Figure 4: Lateral view of the appropriate implant trial in the disc space. Note the round shaped pilot hole in the centre of the trial for an accurate alignment.
The surgeon should avoid oversizing the trial because an oversized artificial disc may limit the normal range of motion. Anteroposterior and lateral fluoroscopic images are usually obtained to ensure that the trial fits and is centered in the disc space. The surgeon should take the time to align the fluoroscope to obtain images without parallax. The trial helps to align the fluoroscope with a pilot hole in the centre of the trial, which provides a round shaped image in an accurate alignment.
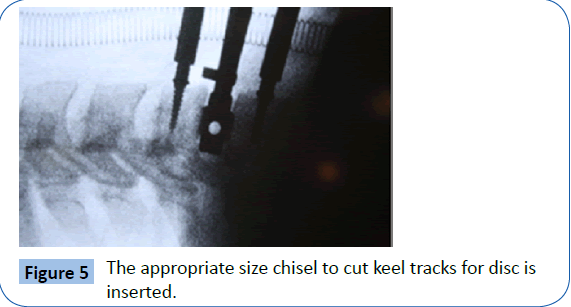
The appropriate size chisel to cut keel tracks for disc is then inserted with the help of a hammer (Figure 5). This maneuver creates keel tracks in the endplates for the rails of the M6-C artificial disc.
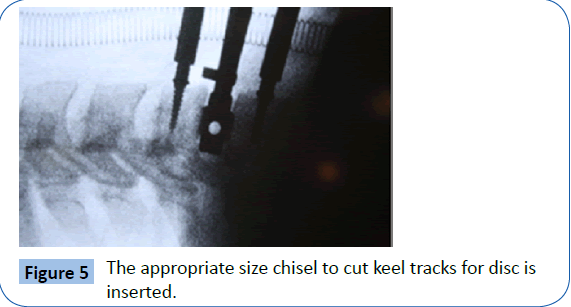
Figure 5: The appropriate size chisel to cut keel tracks for disc is inserted.
The M6-C is then inserted, taking care to align its rails with the channels cut into the endplates. The inserter is removed and lateral and anteroposterior fluoroscopy is generally used again to confirm appropriate positioning and size of the implant. The platysma is then closed, and the anterior cervical skin incision is closed with subcuticular suture.
You can flex and extend the patient’s neck manually on the operating table while imaging the implant with lateral fluoroscopy to ensure appropriate motion of the device.
Methods
Between January 2006 and March 2009 cervical artificial disc replacement has been performed in 55 patients. All the cases were operated according to the standard procedure for artificial disc replacement. Data were extracted from patient’s medical records, and the clinic’s electronic files. Long-term data were extracted from the clinic follow-up and outpatient reports. There were 31 males and 24 females. Age at surgery ranged from 19 to 65 years (average of 43.7 years). Clinical symptoms were on the left side in 29 patients (52.7%), on the right side in 22 patients (40%) and bilateral in 4 patients (7.3%). The used artificial discs were M6-C artificial disc (Spinal Kinetics Sunnyvale, CA).
Disc replacement was done in C 6/7 in 30 patients (54.5%), C5/6 in 14 patients (25.5%), C 4/5 in 4 patients (7.3%), 5 patients in two levels (9%), and 2 patients had 2 level operation in combination with a cage.
Results
4 patients have been re-operated; one patient was been reoperated due to problem related to the artificial disc, the patient had hyper-mobility of the operated level, the second one due to residual disc material. Within 7 months after surgery, 2 other patients were re-operated due to degeneration of the adjacent discs. No complications were experienced during the insertion of the prosthesis and no patients had deep infection or death related to either procedure.
Postoperative radiological findings showed limitation of the cervical mobility in the operated segment in 6, progression of degeneration of the adjacent discs in 3 patients: one of them was known before surgery, remnant spondylophyts at the level of surgery in 3 patients and slight kyphosis in one patient. Postoperative radiographics following surgery confirmed accurate placement of the prosthesis and preserved mobility of the functional spinal unit in 46 patients (83.6%).
Complication avoidance
We can reduce complications and failure rate of the cervical arthroplasty with the M6-C device by strict adherence to the illustrated surgical technique for implantation and the following key features.
1. During the positioning of the patient avoid cervical hyperextension which may lead to kyphotic position of the device when the cervical spine is back to a neutral position. A kyphotic position may lead to an inappropriately sized arthroplasty, which is usually too small for the disc space. Therefore the patient’s cervical spine should be positioned in a neutral position.
2. Ensure sufficient decompression of the exiting nerve roots to avoid nerve root impingement during extremes of flexion, extension, and rotation motions of the artificial disc.
3. The endplates should be prepared properly for the implant. Ensure that all disc material is removed from the endplates, taking care to avoid violating them. Intact endplates are necessary for an artificial disc analogous to anterior cervical fusion to avoid subsidence of the device.
4. Select the appropriate size for the arthroplasty. The smallest height is 6 mm so the risk for oversizing is greater than implantation of a too small sized device. It leads to inhibition of the normal range of motion of the implant because the facets and posterior ligaments are too splayed to function properly and due to overstretching it may cause neck pain.
5. The M6-C artificial disc device should be implanted in the midline and in alignment with the dorsal margin of the vertebral body. Eccentric placement of the device away from the center of rotation and the midline of the disc space may inhibit its normal range of motion. There is a greater need for surgical precision and proper alignment when performing M6-C artificial disc implantation compared with anterior cervical fusion.
Conclusion
The device is safe, and the clinical outcomes have been excellent. Clinical and radiographic results are encouraging. Radiographic results show that the M6-C artificial disc maintains motion at the treated level without adjacent-segment compromise. Our preliminary results from this limited number of patients indicate that the M6 disc is potentially a viable alternative to fusion for primary cervical disc disease; however, further clinical studies with larger sample sizes and long term outcome assessment will be required to show statistical benefits in preserving normal motion and decrease the incidence of adjacent level disease.
Cervical arthroplasty procedures selected appropriately for the patient can optimize the patient’s opportunity for neurological improvement and faster recovery than anterior cervical fusion techniques and presumably can reduce the progressive process of adjacent level degeneration. However the quality requirements for an arthroplasty device are one of the most challenging aspects. In this issue the M6-C artificial disc comes very close to the physiological cervical disc and shows great promise for preserving physiological spinal motion and for decrease of the incidence of adjacent level disease.
Appropriate patient selection and attention to surgical technique, as described in this article, are very important to reduce complications and optimize patient benefit from cervical arthroplasty.
7047
References
- Baskin DS, Ryan P, Sonntag V, Westmark R, Widmayer MA (2003) A prospective, randomized, controlled cervical fusion study using recombinant human bone morphogenetic protein-2 with CORNERSTONE-SR allograft ring and the ATLANTIS anterior cervical plate. Spine 28: 1219–1225.
- Boakye M, Mummaneni PV, Garrett M, Rodts G, Haid R (2005) Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. J Neurosurg Spine 2: 521-525.
- Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50: 229-236.
- Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81: 519-528.
- Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, et al. (1999) Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 24: 670-675.
- Goffin J, van Loon J, Van Calenbergh F, Plets C (1995) Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord 8: 500-508.
- Anderson PA, Sasso RC, Riew KD (2008) Comparison of adverse events between the Bryan artificial cervical disc and anterior cervical arthrodesis. Spine (Phila Pa 1976) 33: 1305-1312.
- Reyes-Sanchez A, Miramontes V, Olivarez L, Aquirre A, Quiroz A, et al. (2010) Initial clinical experience with a next-generation artificial disc for the treatment of symptomatic degenerative cervical radiculopathy. SAS 4: 9-15.
- Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, et al. (2002) Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg 96: 17-21.
- Mummaneni PV, Haid RW (2004) The future in the care of the cervical spine: interbody fusion and arthroplasty. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 1: 155-159.
- Mummaneni PV, Robinson JC, Haid RW Jr (2007) Cervical arthroplasty with the PRESTIGE LP cervical disc. Neurosurgery 60: 310-314.
- Sekhon LH1 (2003) Cervical arthroplasty in the management of spondylotic myelopathy. J Spinal Disord Tech 16: 307-313.
- Schonmayr R, Kim I, Maurer J C, Melzer M (2009) Cervical disc replacement Experiences with 4 different models.
- Cunningham BW, Hu N, Beatson HJ, Serhan H, Sefter JC, et al. (2009) Revision strategies for single- and two-level total disc arthroplasty procedures: a biomechanical perspective. Spine J 9: 735-743.
- Apfelbaum RI, Kriskovich MD, Haller JR (2000) On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976) 25: 2906-2912.