Ana Nedic1*, Djurdjica Kasuba Lazic2, Jana Vrbanec3, Milan Milosevic4 and Milica Katic5
1Department of Internal Medicine, General Hospital Virovitica, Gajeva 21,Virovitica 33000, Croatia
2Department of Family Medicine, Andrija Stampar School of Public Health, School of Medicine, University of Zagreb, Rockfellerova 4, 10000 Zagreb, Croatia
3Cakovec Health Center, Ivana Gorana Kovacica 1e, 40000 Cakovec, Croatia
4Occupational and Sports Medicine specialist, Department of Environmental and Occupational Health, Andrija Stampar School of Public Health, School of Medicine, University of Zagreb,Rockfellerova 4, 10000 Zagreb, Croatia
5Department of Family Medicine, Andrija Stampar School of Public Health, School of Medicine, University of Zagreb, Rockfellerova 4, 10000 Zagreb, Croatia
- *Corresponding Author:
- Ana Nedic
Department of Internal Medicine, General Hospital Virovitica
Gajeva 21, Virovitica 33000, Croatia
Tel: 00385919862840
E-mail: ana.nedic25@gmail.com
Received date: December 14, 2015 Accepted date: January 09, 2016 Published date: January 15, 2016
Citation: Nedic A, Lazic DK, Vrbanec J, et al. Challenges for GP in Longitudinal Care for Chronic Patients: An 18-Year Follow-Up. Arch Med. 2015, 8:2.doi: doi number
Keywords
Chronic diseases, Multimorbidity, Polypharmacy, GP visits, General medicine
Key Messages
- Chronic diseases, multimorbidity and polypharmacy have become a leading and growing problem of family care services.
- It is important to think of multimorbidity as a concept.
- There is a need for implementation of new, efficient models of care for chronic patients with multimorbidity in family medicine.
Introduction
Multimorbidity is usually defined as co-occurence of two or more chronic diseases in the same individual. Recently, multimorbidity is defined as a new concept encompassing all the medical conditions of an individual patient [1]. General practitioner (GP) has a leading role in an integrated management of patients with multimorbidity and provides comprehensive and patient-focused care [2]. Apart from being a burden to the patient in terms of disability and reduced quality of life, multimorbidity is a major burden in all developed societies of the world due to the high costs of health care for these patients, frequent and sometimes unjustified use of health care services as well as high consumption of drugs [3]. Until now it is known that multimorbidity is often associated with an older age, but it is noticed that the incidence is increasing in younger age, especially in socially deprived areas [4].
In terms of aging of human population a new studies about multimorbidity dynamics and prevalence are constant demand in order to better adapt primary care resources to patients with multiple chronic diseases. Also, multimorbidity is a great scientific challenge because it represents one of the major health problems in the modern medicine and has a clear impact on public health.
Polypharmacy is one of the most common consequences of multimorbidity. It is defined as the use of three or more drugs in an individual patient and it is classified as low (use od 2-3 drugs), moderate (use od 4-5 drugs) and high (use of>5 drugs) [5]. Polypharmacy is often associated with inappropriate prescribing, the occurence of adverse side effects and drug interactions [6]. Basic principle of the rational drug prescription is choosing the most effective drug with the least risk and the least cost while respecting the patient's choice [7]. In the case of care for patients with multimorbidity this is a particular challenge and that is why the cohort studies, either population-based, either on a singlepractice are important. Their goal should be to raise awareness about the extent of polypharmacy and its impact on everyday work organization.
Polypharmacy is often accompanied by polypragmasy which indicates excessive use or the use of unnecessary drugs. Polypragmasy is a complex problem which can be caused by GPs, other specialists and even patients, but mostly by the interaction of all three [8]. In the context of polypharmacy, polypragmasy is often disregard and unrecognized although also has a major and clear impact on public health and health policy.
The objectives of this cohort study are to research the dynamics of development of multimorbidity and its consequences on the content of health care on the population of chronic patients of one GP practice during 18 years, likewise the impact of multimorbidity on the frequency of the use of family medicine services and polypharmacy.
Methods
Study design
This research is a continuation of retrospective cohort study of chronic diseases carried out in the period from 1994 to 2003 on a sample population of chronic patients which in 1994 had one or more chronic diseases registered in their medical records. The data were collected from paper and electronic medical records in a teaching practice of one family physician at the Department of Family Medicine at the School of Medicine in Zagreb, Croatia. For the purpose of continuation of the research we collected new data during the period from 2003 to 2012 which was the second phase of this research.
Selection of study subjects
At first we defined chronic disease as a long-lasting condition of slow progression in which a progressive disorder of organs, organ system or whole organism leads to a serious difficulties of psychological, physical and social functioning of individuals and disenable the patients to complete their daily activities.
The inclusion criteria was that the patient has at least one chronic disease registered in its medical record.
Collection of data
In the phase one of the study (1994-2003) we collected data on the age and gender of patients and all registered chronic diseases during 10-year period marked with a code according to the International Classification of Diseases and Related Health Problems (ICD-10). We also collected data on the use of services of the family physician. In the phase two of the study (2003- 2012) we collected data on new chronic diseases registered in the medical records according to the ICD-10, visits to the GP in each year of the research for period during 2003-2012, and additionally we collected data on the number and type of prescribed and used drugs for chronic diseases in years 2003 and 2012. The type of drugs included in the study were chronic drugs, thus we analyze the total number of chronic drugs used according to gender in years 2003 and 2012.
Sample selection
When the study began in 1994 there were 560 chronic patients in our sample population. In 2003 there were 289 chronic patients of the researched sample and in 2012 there were 183 chronic patients from the same population (51 men and 132 women).
The reasons for that decrease of a sample size are natural demographic changes such as death of a part of the population, change of residence and change of GP in the part of the population and consequences of the civil war which was in Croatia in the beginning of this study. Some of the patients were the refugees who eventually move back to their homes and GPs according to their place of living so that also influenced on a reduction of sample size.
Statistical analysis
Data were shown in tables and pictures. Differences between age groups and gender regarding each investigated year were analyzed with chi square test (categorical values) and Kruskal-Wallis test (quantitative values). All P values below 0,05 were considered significant. Data analysis software system IBM SPSS Statistics, version 21.0 (www.spss.com) was used in statistical analyzes.
Results
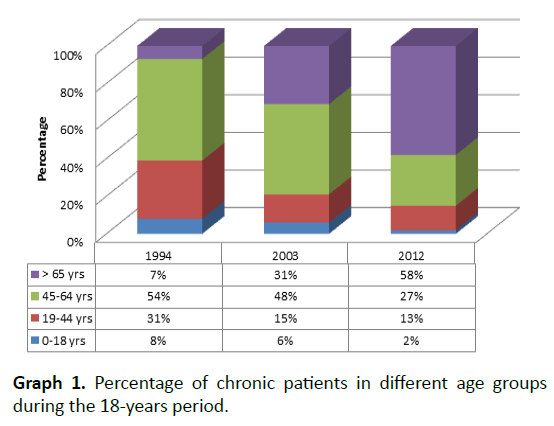
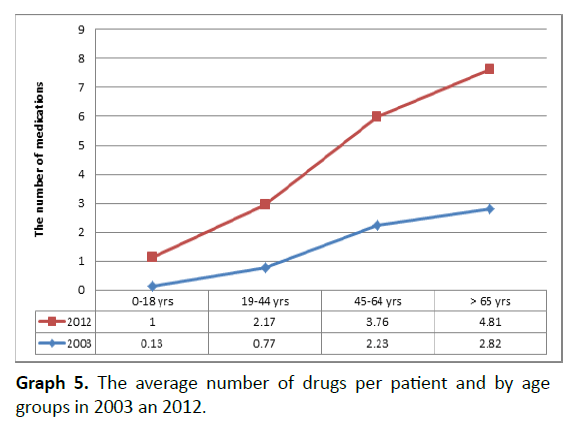
The changes in the structure of population were recorded in an 18-years follow-up (Graph 1).
Graph 1. Percentage of chronic patients in different age groups during the 18-years period.
During the research period, the number of patients changed in all age groups which is very illustrative shown in the graph above. There is a decrease in the number of patients registered in all age groups except in group of 65 and older. Only in that age group there was an increase in number of patients for 51%.
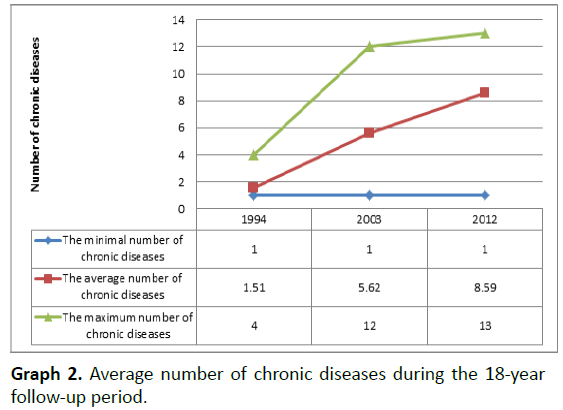
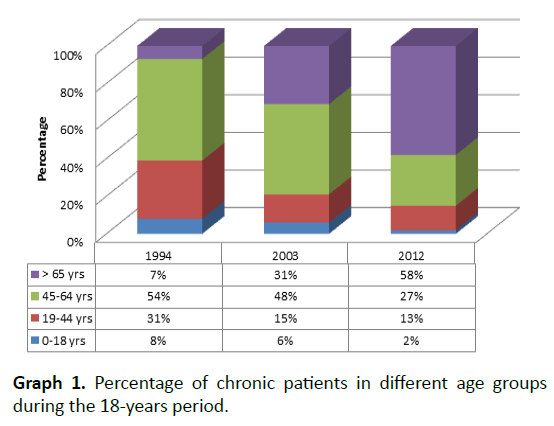
The aging of patients brought in new chronic diseases, which is clearly presented on the next graphs.
During the research period, an increase in the number of chronic diseases per patient was noticed. The average number of chronic diseases per patient increased from 1.51 to 8.59 as registered in 1994 and 2012, respectively. Thus, in 2012 the number of chronic diseases per patient was five times greater when compared to 1994. The maximum number of chronic diseases in the beginning of the research was 4, while at the end of the research it was 13 which is almost a threefold increase and it is shown in the Graph 2.
Graph 2. Average number of chronic diseases during the 18-year follow-up period.
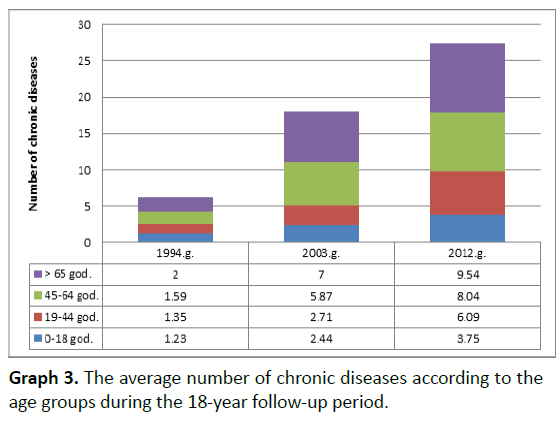
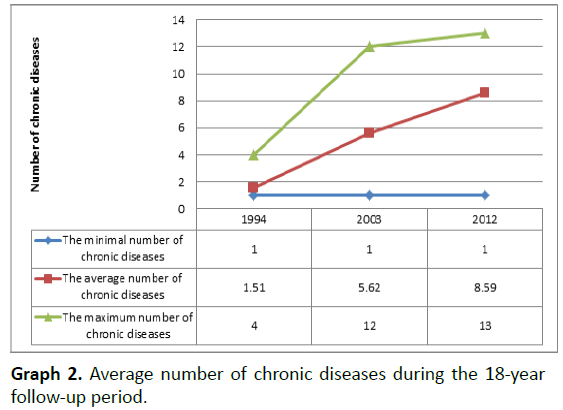
The constant increase of the average number of chronic diseases in the older age groups is obvious. In the age group 0-18 years the average number of chronic diseases increased 3 times; in the age group 45-64 it increased more than 5 times, whereas in the age group older than 65 the number of chronic diseases increased more than 4.5 times (Graph 3).
Graph 3. The average number of chronic diseases according to the age groups during the 18-year follow-up period.
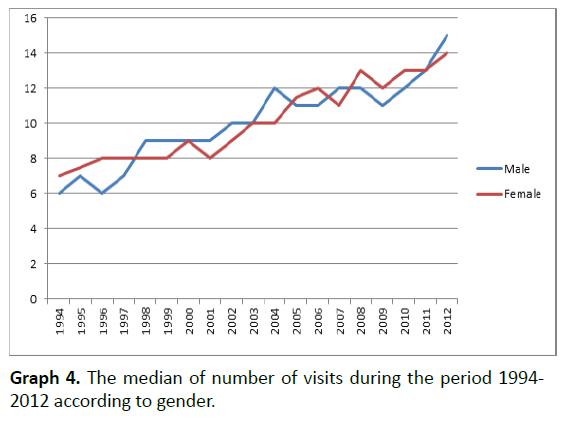
Chronic patients are frequent visitors to the GPs. In this study the incidence of visits to GP was observed according to gender. There was an increase of visits in both genders (Graph 4).
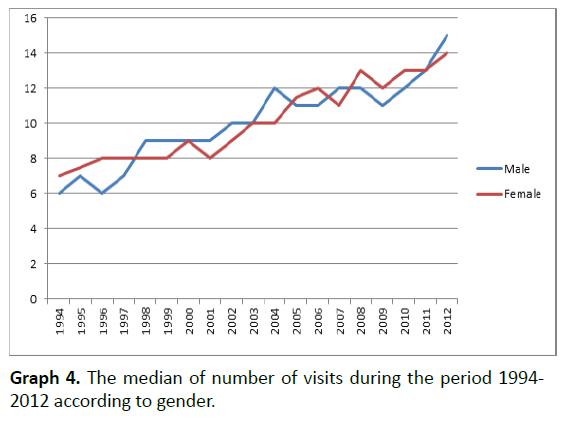
Graph 4. The median of number of visits during the period 1994- 2012 according to gender.
Concerning gender, there was a statistically significant increase in the number of visits in both genders (P<0.001).
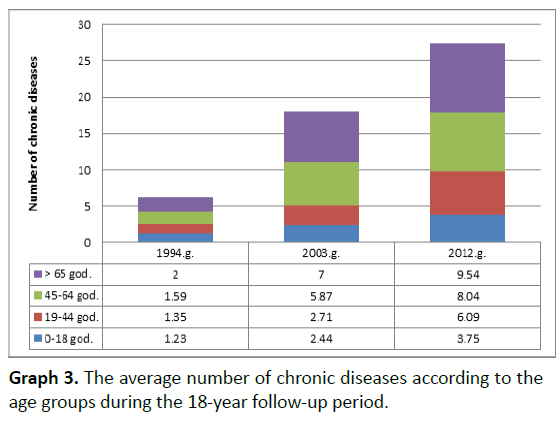
Consequently with the increased number of chronic diseases, the increased number of drug prescriptions was also noticed (Graph 5).
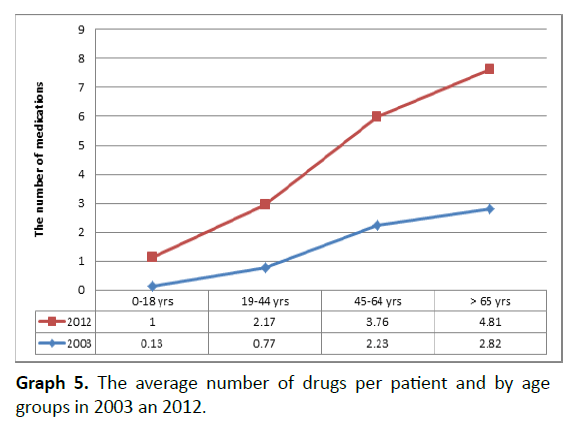
Graph 5. The average number of drugs per patient and by age groups in 2003 an 2012.
The most significant increase was noticed in the age group of those older than 65. In 2003 there were 2.82 medications per chronic patient prescribed, while in 2012 the number was 4.81. The highest number of drugs used per chronic patient was noticed in the same group; it was 11 for both years, 2003 and 2012. Also, related to gender, in the ten-year period the drug prescription increased for both genders.
Discussion
Main findings
This study demonstrates the existence of the problems considering multimorbidity and polypharmacy in general medicine. General practitioner (GP) is known as a „gate keeper“ of a national healthcare system and consequently endures the burden related to multimorbidity and polypharmacy which are rapidly increasing.
It is obvious that human population is aging. It is expected that life expectancy expands to 83 years by year 2050 [9]. In Croatia according to the 2011 census there was 17.2% of the population older than 65 years [10]. Our study, although on a small sample, also demonstrates an increasing trend of aging and all the consequences related to it such as: increased number of chronic disease, increased visits to GP, increased number of drug prescription. For example: in 18-year follow-up period the number of chronic disease per patient increased five times. Consequently, the statistically significant increase in the number of visits to GP was noticed and also an increase in the number of prescribed drugs was registered, too. The average number of medications per participant doubled in ten-year period. These findings are related to a burning issue of a complex patient with multimorbidity in everyday practice. As the clinical situation of the patient becomes more complex and requires intervention of different specialists, the likelihood of a lack of coordination among professionals is higher [6]. The results of our study are trying to illustrate the extent of problems that GPs encounters everyday in its practice.
Strengths and limitations of the present study
The main strength of our study is a long follow-up period of 18 years of the same population. Also, the study was performed in a teaching practice of family physician with great experience and knowledge at the Department of Family Medicine at the School of Medicine in Zagreb, Croatia. We purposively sampled experienced GP to ensure sufficient exposure to the multimorbidity and polypharmacy. This means that data about participants were very accurate and detailed registered in their paper and electronical medical records.
The greater limitation of this study is a decreasing of a sample size during the research period. There are a various reasons but mainly, there were natural demographic changes such as death of the part of the population, change of residence and change of GP in the part of the population. Also, one important reason is a civil war which was in Croatia in the beginning of this study. Some of the patients in our sample were the refugees who eventually move back to their homes and GPs according to their place of living. So, that also influenced on a reduction of a sample size. Partially, this is an explanation why in our study the percentage of older than 65 years was 7% at baseline (in 1994) which is rather low compared to other European settings at that time where they conform 10-15% of the primary care population [9]. First, the research practice is in Zagreb which is the capital and there is more young, working people and families according to the other smaller towns or rural parts of the country. Secondly, as we already mentioned during the civil war the refugees were part of the patient population and they were mainly mothers with children while the elderly usually refused to leave their homes.
Interpretation of the study results in relation to an existing literature
Although the number of studies which investigate the multimorbidity of chronic diseases with its consequences increases, still most evidence on chronic diseases has been collected for a single disease. There is a growing need for evidence-based answers to multimorbidity especially in primary care settings.
Multimorbidity prevalence is ranging from about 45% in less developed countries to more than 80% in very developed countries, most usually in population older than 65 [11,12]. In our study it was 58% of older than 65 with multimorbidity, but more impressive is the increase over a period of 18 years which was 51%. According to Croatian Health Statistics Yearbook in 2001 there were 6 664 236 chronic diseases, while in 2012 there were 11 860 284 chronic diseases which is almost double increase [13,14]. The improvement in the diagnosis and registry of chronic diseases is likely to be a major driving force for such an increase of multimorbidity.
Patients with multimorbidity of chronic diseases frequently visit their GP. The number of consultations is progressively higher in the last two decades which correlates with our results [15]. Also, according to Croatian Health Statistics Yearbook in 1990 in Croatia there were a total of 15 907 836 visits to GP per year, while in 2012 there were 31 047 097 visits per year which is more than double increase, like in our study [14,16].
The causes are increased number of chronic diseases, number and availability of GPs, education of physicians, national health legislation and programs, economic, health and social development [17]. Earlier studies showed that frequent visitors have more chronic diseases, suffer from mental disorders and psychological stress, have worse health beliefs and have a great need for confirmation and advice than the so-called rare visitors [17,18].
All of that has a great influence on GPs work organization and efficiacy and it is imperative to realize the importance of this problem.
Multimorbidity is a major and essential risk factor for polypharmacy and the literature speaks of „two sides of the same coin“ [6]. Most of the former researches of polypharmacy agree that there is a lack of adequate guidelines for treatment of patients with multimorbidity and polypharmacy [19]. Evidence-based medicine results needs improvement. The available evidence regarding the efficiacy of medications have been generated by clinical trials involving patients completely different from those currently treated at GPs: much younger, affected by a single disease and managed in highly controlled environment [20]. Often question in GPs practice is „What to give the patient who already has everything?“ Using clinical guidelines in the management of patients with multimorbidity can lead to the prescription of multiple and sometimes conflicting medications which leads to polypragmasy. Usually GPs respond to conflicts in the management of patients with multimorbidity by making compromises between patient-centred and evidence-based care [21].
Rates of polypharmacy are increasing. In one big retrospective study on a sample of 180 815 25, 2% received one to three drugs, 11% recevied four to six drugs, 5,19% received seven to nine drugs and 4,6% received more than ten drugs [22]. In our study the highest number of drugs used per patient was 11 both in years 2003 and 2012. In the ten-year period drug prescription doubled, which is according to a sample size significant increse. The average number of drugs per patient older than 65 was 4,81 drug. It is known from the other literature that the number of used drugs is significantly higer after 65 years [23].
Polypharmacy significantly increases the risk of inappropriate prescription of drugs and the occurence of side effects. According to the literature, co-administration of two drugs makes the prospect of interaction of more than 5%; if five drugs are applied the probability of interactions are ten times greater-up to 50%; and if an older patient applies eight drugs at the same time the probability for interaction is 100% [24]. According to the research by Kaufman, 57% of women over 65 use five or more medications, while a research conducted in Europe found that 51% of patients in the average age of 82 use six or more medications [25,26]. There are numerous risk factors for polypharmacy: those which we cannot influence are age, gender and level of multimorbidity, while those which we can influence are the frequency of visits to GP and refferal to specialists. Each new specialist who participates in the care of patients with multimorbidity increases the likelihood of side effects of drugs for 12-28% [27].
Polypharmacy can very easy and often exceed to polypragmasy, which is defined as irrational prescribing by a doctor, or irrational taking by a patient of many types of medications. Polypragmasy often leads to adverse interactions and side effects. It is known that drug side effects are expressed in 5,5% to 34,7% of the population who take more than five drugs [28].
Multimorbidity is strongly related to occurence of adverse drug events, insofar as it requires the intervention of multiple specialists and the prescription of multiple medications [6].
Conclusion
In our study we demonstrated the development of multimorbidity over a period of 18 years. The results show that the number of chronic disease increased five times mostly in older patients. Also the number of visits to the GP was more than two time greater in a research period, while a presciption of medications doubled in a ten year period.
The aim of our study was to confirm our objectives that there is a rapid increase of burden related disease and burden related polypharmacy in family medicine. Evidence based medicine which includes patient situation, scientific evidence and doctor's expertise needs adjustment to this new trend of aging of the population and all consequences related to this phenomenon.
In the clinic, a thorough assessment of the patient preferences, and physical, mental and social functioning in combination with increased level of physician's experience can increase the quality of care for older patients with multimorbidity and polypharmacy.
8459
References
- Le ResteJY, Nabbe P, Manceau B, Lygidakis C, Doerr C, et al. (2013) The European General Practice Research Network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. J Am Med 14:319-325.
- Lazic D (2008) Prevalence of multimorbidity and characteristics of co-morbidity of chronic diseases in the population of general practice patients.
- Moffat K, Mercer SW (2015) Challenges of managing people with multimorbidity in today's healthcare systems. BMC FamPract 16: 129.
- McLean G, Gunn J,Wyke S, Guthrie B, Watt GC, et al. (2014) The influence of socioeconomic deprivation on multimorbidity at different ages: a cross-sectional study. Br J Gen Pract 64: e440-447.
- Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM (2000) The development of polypharmacy. A longitudinal study. FamPract 17: 261-267.
- Calderon-Larranaga A, Poblador-Plou B, González-Rubio F, Gimeno-Feliu LA, Abad-DíezJM, et al. (2012)Multimorbidity, polypharmacy, referrals, and adverse drug events: are we doing this well? Br J Gen Pract62:e821-e826.
- Katic M (2013) Prescription of drugs in family medicine. Textbook of Family medicine.
- KasubaLazic D (2015)Polypharmacy in family medicine – the growing problem of 21st century.
- World Health Organization. Health statistics and health information systems.
- Croatian National Institute of Public Health. Croatian Health Service Yearbook 2011.
- Pati S, Swain S,Hussain MA,Kadam S, Salisbury C4 (2015) Prevalence, correlates, and outcomes of multimorbidity among patients attending primary care in Odisha, India. Ann Fam Med 13: 446-450.
- Van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, et al. (2011) Which chronic diseases and diseases combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health 11:101.
- Croatian National Institute of Public Health. Croatian Health Service Yearbook 2001.
- Croatian National Institute of Public Health. Croatian Health Service Yearbook 2012.
- Smith SM, O'Kelly S, O'Dowd T (2010) GPs' and pharmacists' experiences of managing multimorbidity: a 'Pandora's box'. Br J Gen Pract 60: 285-294.
- Croatian National Institute of Public Health. Croatian Health Service Yearbook 1990.
- Carney TA, Guy S, Jeffrey G (2001) Frequent attenders in general practice: a retrospective 20-year follow-up study. Br J Gen Pract 51: 567-569.
- Luciano JV,Fernández A, Pinto-Meza A, Luján L, Bellón JA, et al. (2010) Frequent attendance in primary care: comparison and implications of different definitions. Br J Gen Pract 60: 49-55.
- Doos L, Roberts EO, Corp N, Kadam UT (2014) Multi-drug therapy in chronic condition multimorbidity: a systematic review. Eur J Intern Med 25:710-716.
- Mannucci PM, Nobili A; REPOSI Investigators (2014) Multimorbidity and polypharmacy in the elderly: lessons from REPOSI. Intern Emerg Med 9: 723-734.
- Sinnott C, Hugh SM, Boyce MB, Bradley CP(2015) What to give the patient who has everything? A qualitative study of prescribing for multimorbidity in primary care. Br J Gen Pract 65: e184-191.
- Payne RA, Abel GA, Avery AJ, Mercer SW, Roland MO (2014) Is polypharmacy always hazardous? A retrospective cohort analysis using linked electronic health records from primary and secondary care. Br J ClinPharmacol 77:1073-82.
- Schuling J,Gebben H, VeehofLJ, Haaijer-Ruskamp FM (2012) Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC FamPract 13: 56.
- Durakovic Z (2011) Geriatric pharmacotherapy. C.T. Business information.
- Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA (2002) Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA 287: 337-344.
- Fialová D,Topinková E, Gambassi G, Finne-Soveri H, Jónsson PV, et al. (2005) Potentially inappropriate medication use among elderly home care patients in Europe. JAMA 293: 1348-1358.
- Marengoni A,Angleman S, Melis R, Mangialasche F, Karp A, et al. (2011) Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 10: 430-439.
- Stark RG, John J, Leidl R (2011) Health care use and costs of adverse drug events emerging from outpatient treatment in Germany: a modelling approach. BMC Health Serv Res 11: 9.