Case Report - (2023) Volume 15, Issue 6
Chest wall tumor - An unusual presentation
Mehwish Aslam*
Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad, Pakistan
*Correspondence:
Dr.
Mehwish Aslam, Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad,
Pakistan,
Tel: + 92 9054627867,
Email:
Received: 01-Dec-2023, Manuscript No. ipaom-23-14334;
Editor assigned: 04-Dec-2023, Pre QC No. P-14334;
Reviewed: 18-Dec-2023, QC No. Q-14334;
Revised: 22-Dec-2023, Manuscript No. R-14334;
Published:
29-Dec-2023
Abstract
The chest wall consists of soft tissues, cartilage and bones. A large
part of the masses originates from soft tissue. Chest wall tumours
constitute 5% of thoracic and less than 1% of all primary tumours;
40% and 60% are malignant. Tumours may originate primarily in
the chest wall and metastasize to or extend into it via local invasion
from adjacent structures. Morbidity and mortality are specific to
the particular tumour type. We report a case of a 42-year-old male
with complaints of a painful lump on the right chest wall, which,
after surgical removal, showed spindle cell sarcoma stage 2. Primary
Spindle Cell Sarcoma (SCS) is an extremely rare entity and one of
the least reported tumours. It is a type of connective tissue tumour
that generally begins in layers of connective tissue under the skin,
between muscles and surrounding organs. Only a handful of cases
have been reported around the world from a variety of body parts.
Keywords
Sarcoma; Chest wall tumour; Spindle cell carcinoma;
Surgery
Introduction
Neoplasms of the chest wall comprise a heterogeneous
group of lesions that are challenging to diagnose and
treat. Chest wall neoplasms may be either primary or
metastatic, with a malignancy rate of ∼50% and these
can be symptomatic or asymptomatic, with ∼20% found
incidentally on chest radiographs [1,2]. Extra thoracic
lesions are more likely to present as a growing mass (Fig.
1). Pain is the most common symptom for both benign
and malignant tumours. Chest radiography, Computed
Tomography (CT), Magnetic Resonance Imaging (MRI)
and Positron Emission Tomography (PET) can all be
used to assess a chest wall tumour. Chest X-ray can detect
calcification, ossification or bone destruction, location and
size but is limited in detail. CT can provide information
about the vascularity of a tumour if contrast is used, as well
as a more detailed appraisal of the mass's extent, location
and composition [3]. Depending on diagnosis, staging and
age, therapy has to be tailored for each patient, as discussed
in a multidisciplinary team setting; however, radical
resection is, in most cases, the significant component
of treatment, along with the use of chemotherapy and
radiotherapy if needed.

Fig. 1. Chest wall carcinoma.
Case Presentation
I present a 42 years old male, a driver by occupation,
resident of Karachi, came to us in Emergency Department
at Abbasi Shaheed Hospital Karachi, Pakistan on
Sept/18/2018, with complaints of a painful lump on the
right side of the chest wall for ten days (Sept/09/2018), the
swelling was gradually increasing in size and was painful
and warm. There was no history of trauma, weight loss,
cough and shortness of breath.
His past medical and surgical history were nonsignificant.
However, he was a smoker of about 20 packs/
year but quit 20 years ago.
On examination, he was a pale-looking man lying on
bed uncomfortably with vitals of:
Pulse: 90 /min.
BP: 120/70 mmHg
R/R: 16 breaths/minute
Temperature: 101 °F
A swelling was about 10 × 5 cm (longitudinal and
transverse) at the mid-clavicular line starting from the fifth
rib; covered by skin, fluctuating, erythematous and warm
with no discharge. However, respiratory and abdominal
examinations were normal.
His initial laboratory reports were:
Hb: 8.9 mg/dl
TLC: 14.6%
Platelets: 311,000
His other labs such as serum urea, creatinine,
electrolytes, PT and INR were normal. However, his Anti-
HCV came out positive incidentally.
Chest x-ray revealed soft tissue swelling from the 5th to
8th ribs on the right side of the chest wall, with no breaching
of lungs or ribs.
In the emergency Operation Room (OR), we operated
patient under the impression of an abscess and drained
about 500 cc of frank blood with clots; there was a 5 cm
cauliflower appearance mass adherent to the chest wall
excised and skin was left open for secondary healing and
specimen was sent for histopathology (which got misplaced
by his attendant).
Postoperatively, 2 pints of blood were transfused and
his Hb. built up to 10g/dl. He was kept on antibiotics
which were ceftriaxone and pain killers. After nine days, he
got discharged with the advice of daily dressings and oral
antibiotics and follow-up in OPD.
On Oct/17/2018, he came again to OPD with
complaints of a mass protruding from the previous
area, around 7 × 7 cm, tender, with rough edges, soft in
consistency, cauliflower-like appearance, foul-smelling
with bleeding from edges (Fig. 1). No lymph nodes were
palpable.
This time he was looking pale and his vitals were:
Pulse: 88/min
BP: 110/80 mmHg
Temp: 99 °F
R/R: 15 breaths/min.
His Hb was 9.2g/dl with a TLC of 15.4% and platelets
of 256,000 with normal Pt, INR, APTT, Serum Urea,
Creatinine, Electrolytes and LFTs, although his ESR was
60 mm/hr.
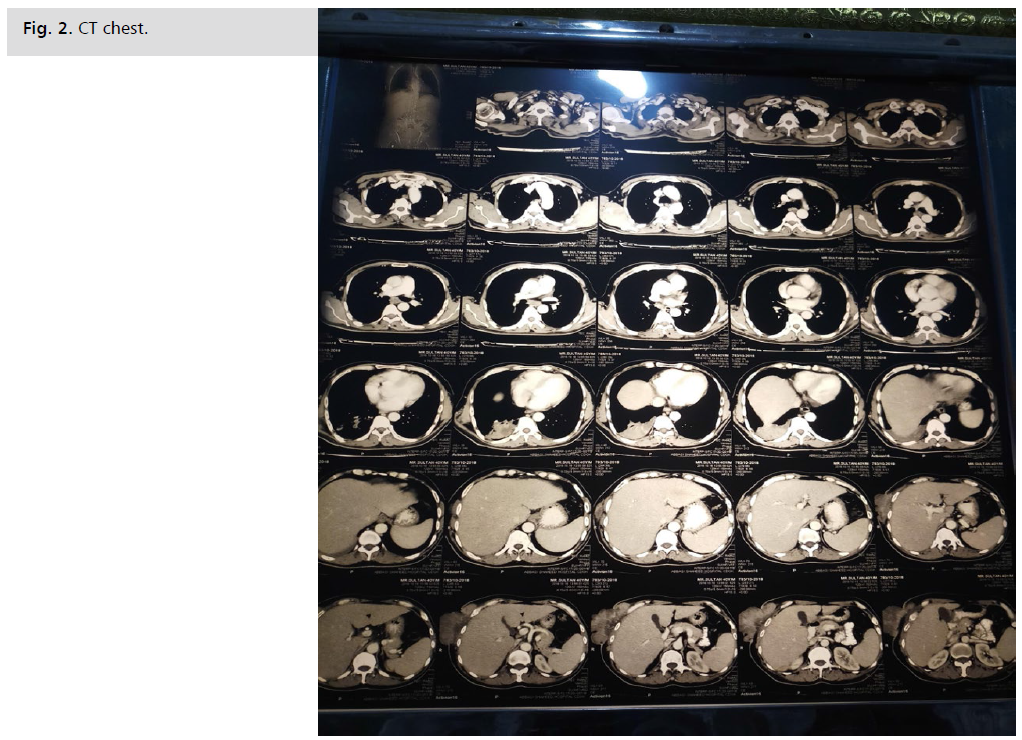
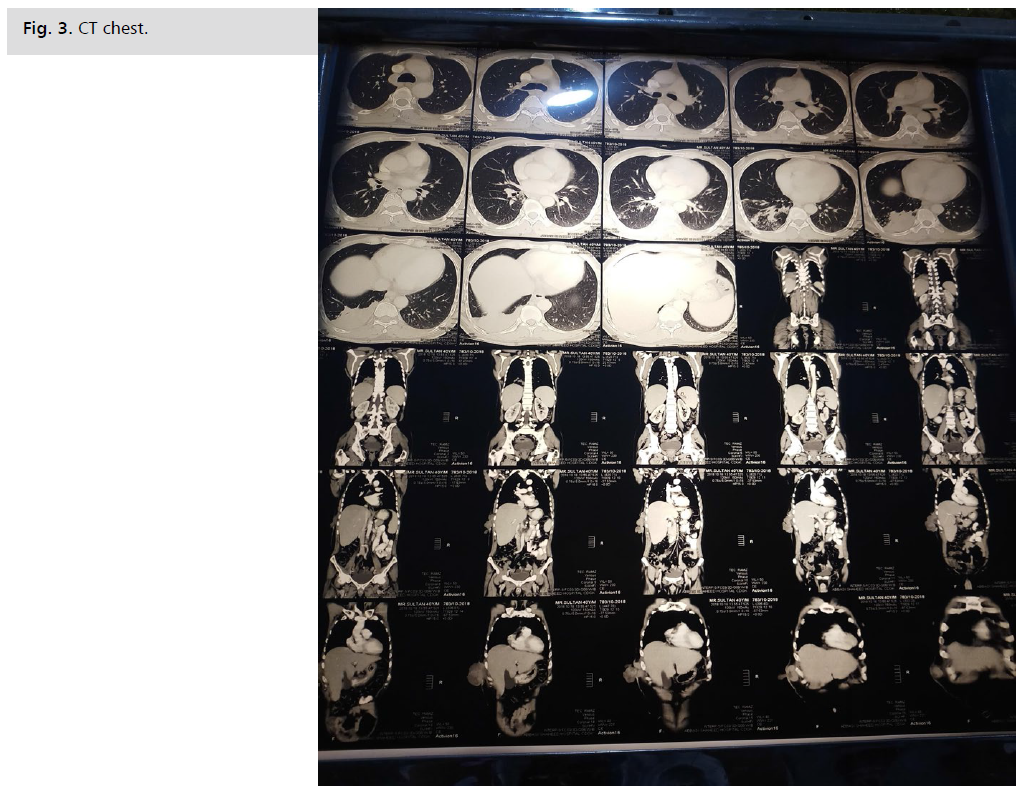
His CT scan findings were: Soft tissue enhancing mass
involving muscles and abutting adjacent ribs without
evidence of bony erosions; margins of the lesion are
lobulated and suggestive of the neoplastic lesion (Fig. 2
and Fig. 3).
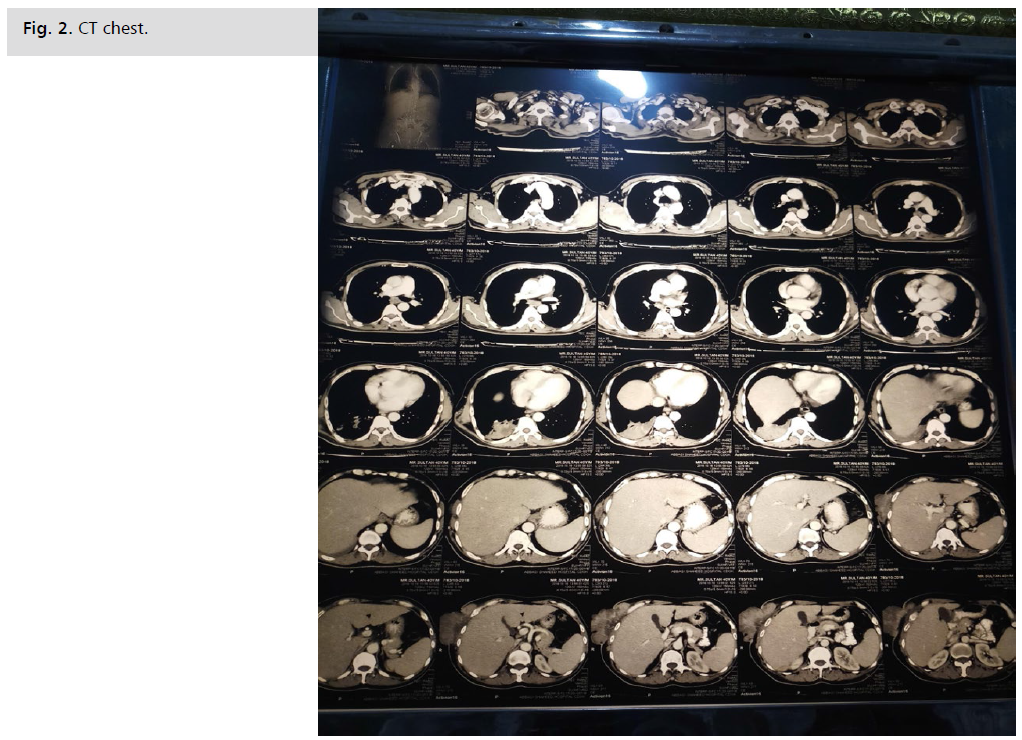
Fig. 2. CT chest.
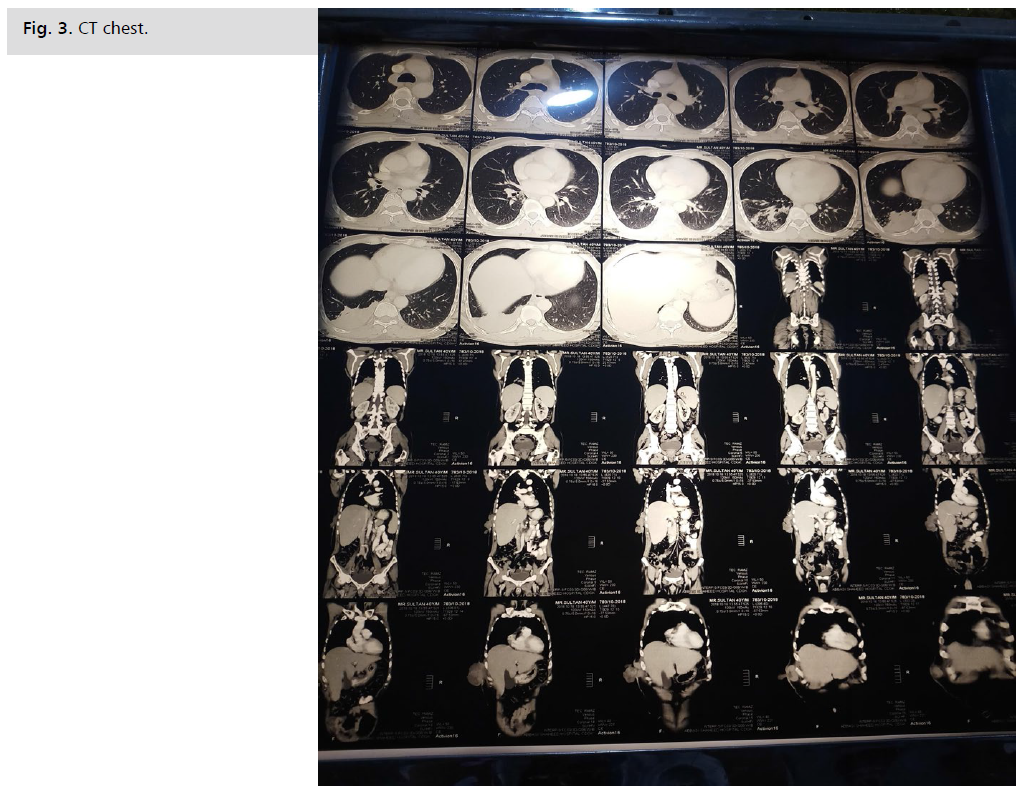
Fig. 3. CT chest.
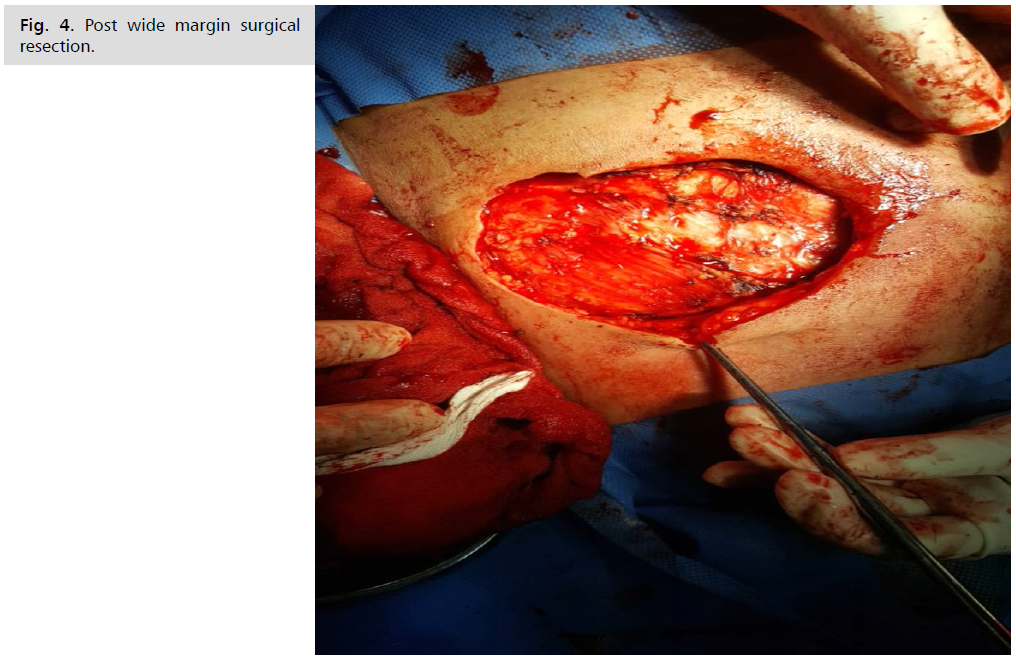
After his workup, we planned for wide margin excision,
performed on the Oct/23/2018. Mass was excised till the
healthy chest wall (Fig. 4), hemostasis secured and the
cavity was washed with hydrogen peroxide and normal
saline. Chest wall muscles were approximated, skin closed
with prolene in mattress fashion (Fig. 5) and the specimen
was sent for histopathology. We gave him injection
ceftriaxone and gentamicin post-operatively.
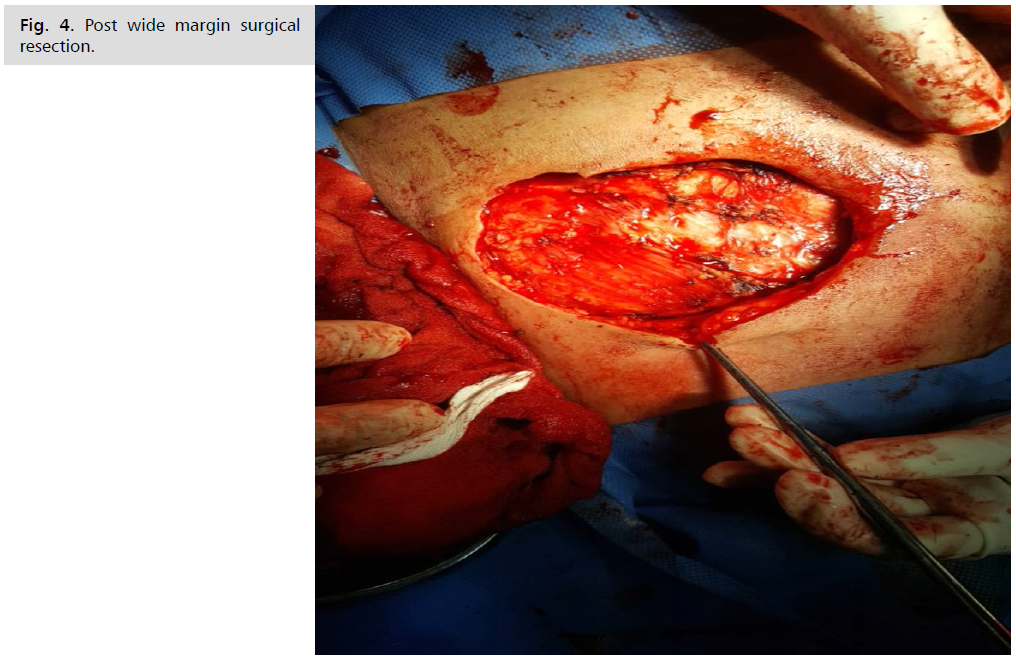
Fig. 4. Post wide margin surgical resection.

Fig. 5. Secondary healing with prolene.
On the 10th postoperative day, he developed
erythematous swelling around the incision, which
was fluctuant; on needle aspiration, around 50 cc
serosanguinous fluid was drained, which was sent for
culture and sensitivity, which depicted the wound was
sensitive with colistin and vancomycin. On Nov/04/2018,
we started vancomycin 1gm along with the advice of high
protein diet.
His histopathology report showed Spindle Cell
Sarcoma. However, the margins showed healthy tissue.
Therefore, we referred the patient to Jinnah Postgraduate
Medical Center Karachi, Pakistan, for an oncologist's
opinion, where his bone scan showed no bony metastasis.
Results and Discussion
As stated previously, more than 50% of chest wall
neoplasms are malignant and most of these malignancies
represent direct invasion from adjacent lung, breast, pleura
and mediastinal tumours. The most common primary
malignancies of the chest wall are sarcomas. At presentation,
older patients tend to have large, aggressive, malignant
chest wall neoplasms, whereas younger patients tend to
have small, benign abnormalities [3]. Approximately 20%
of chest wall tumours may be detected initially at chest
radiography. A plain chest X-ray can make the diagnosis.
However, Computed Tomography (CT) or Magnetic
Resonance (MR) imaging best detects the carcinoma.
Ultrasonography has a limited role in detection as it can be used to take a biopsy. A PET scan helps plan the course of
the definitive treatment [4]. Treatment depends on staging;
Stage I soft tissue sarcomas are low-grade tumours of any
size. Small (less than 5 cm or about 2 inches across) tumours
of the arms or legs can be treated with surgery alone. Most
stage II and III sarcomas are high-grade tumours. They tend
to grow and spread quickly. Some stage III tumours have
already spread to nearby lymph nodes; therefore, surgically
removing the tumour is the primary treatment. Lymph
nodes will also be removed if they contain cancer cells.
Radiation may be given after surgery as the local recurrence
rate is high. A sarcoma is considered stage IV when it has
spread to distant sites (M1). Stage IV sarcomas are rarely
curable; chemotherapy and radiotherapy are used to relieve
symptoms [5]. A retrospective study at the University of
Washington Medical Center has shown that as compared
with surgery alone, disease-free survival at both 5 and 10
years improved by 92% with the addition of radiation
therapy to surgery. It is increased by 82% with the addition
of chemotherapy to surgery and by 89% and 90% with the
addition of both chemotherapy and radiation therapy at 5
and 10 years, respectively [6].
Conclusion
Chest wall tumors are rare and present as a clinical
challenge for surgeons. In addition to rarity, symptoms
are usually non-specific as this patient presented with
fluctuant, erythematous, rapidly growing swelling. This
case report highlights the importance of prompt using
of accurate radiological testing (e.g., CT) in making an
accurate diagnosis in patients with significant chest wall
swelling and pain. After diagnosing a patient with a tumor
on the chest wall, the patient’s case should be discussed by
a multidisciplinary group including surgeons, pathologists,
radiologists, radiotherapists, medical oncologist and plastic
surgeons, to plan optimal treatment and reconstructive
possibilities.
Acknowledgement
None.
Conflict of Interest
None.
References
- Harati K, Kolbenschlag J, Bohm J, et al. Long-term outcomes of patients with soft tissue sarcoma of the chest wall: Analysis of the prognostic significance of microscopic margins. Oncol Lett. 2018;15(2):2179-2187.
Google Scholar, Crossref, Indexed at
- D'addario G, Früh M, Reck M, et al. Metastatic non-small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21:v116-v119.
Google Scholar, Crossref, Indexed at
- David EA, Marshall MB. Review of chest wall tumors: A diagnostic, therapeutic and reconstructive challenge. Semin Plast Surg 2011;25:016-024.
Google Scholar, Crossref, Indexed at
- Carter BW, Benveniste MF, Betancourt SL, et al. Imaging evaluation of malignant chest wall neoplasms. Radiographics. 2016;36(5):1285-1306.
Google Scholar, Crossref, Indexed at
- https://www.cancer.gov/types/soft-tissue-sarcoma/patient/adult-soft-tissue-treatment-pdq
- Burt A, Berriochoa J, Korpak A, et al. Treatment of chest wall sarcomas: A single-institution experience over 20 years. Am J Clin Oncol. 2015;38(1):80-86.
Google Scholar, Crossref, Indexed at