Yahya Mohd Aripin1,*, Nora Julianna Osman1, Suraya Othman1, Muhammad Abid Amir2, Adli Azam Mohammad Razi2, Mohd Zamrin Dimon2, Nadia Hanom Ishak3 and Karis Misiran3
1 Discipline of General Surgery, Faculty of Medicine UiTM, Sungai Buloh Campus, Sungai Buloh, Selangor Darul Ehsan, Malaysia
2 Discipline of Cardiothoracic and Vascular Surgery , Faculty of Medicine UiTM, Sungai Buloh Campus, Sungai Buloh, Selangor Darul Ehsan, Malaysia
3 Discipline of Anaesthesiology, Faculty of Medicine UiTM, Sungai Buloh Campus, Sungai Buloh, Selangor Darul Ehsan, Malaysia
*Corresponding Author:
Yahya Mohd Aripin
Discipline of General Surgery
Faculty of Medicine UiTM
Sungai Buloh Campus
Sungai Buloh, Selangor Darul Ehsan, Malaysia.
Tel: +603 6126 5000
Fax: +603 6126 5224
E-mail: mayahya3@gmail.com
Received date: May 24, 2018; Accepted date: May 25, 2018; Published date: June 02, 2018
Citation: Aripin YM, Osman NJ, Othman S, Amir MA, Razi AAM, et al. (2018) Combined Total Thyroidectomy and Coronary Artery Bypass Grafting: An Endocrine Surgeon Perspective. J Univer Surg. Vol.6 No.2:15
Keywords:
Thyroidectomy; Coronary artery bypass grafting
Introduction
Coronary artery disease may be complicated with presence of thyroid enlargement. Both are not related in terms of the pathogenesis, but the later carries risk of airway obstruction during the perioperative period. Thus, the consideration whether to perform concurrent thyroidectomy during coronary artery bypass grafting (CABG) is a valid decision making to be made.
Combined thyroidectomy and coronary arterial bypass grafting (CABG) have been reported to be feasible and safe. However, how the procedure should be performed was not explicitly explained. We present our experience with a patient and provide relevant important points pertaining to the patient.
Case report
A 66 year old lady presented to the cardiology clinic with progressive exertional dyspnoea and bilateral pedal oedema for six months. Echocardiography showed severe hypokinetic inferior and infero-lateral cardiac wall with left ventricular function of 28 percent. Coronary angiography revealed severe triple-vessel disease while dobutamine stress echocardiography showed ischemic but viable anterior wall, necessitating early coronary artery bypass grafting.
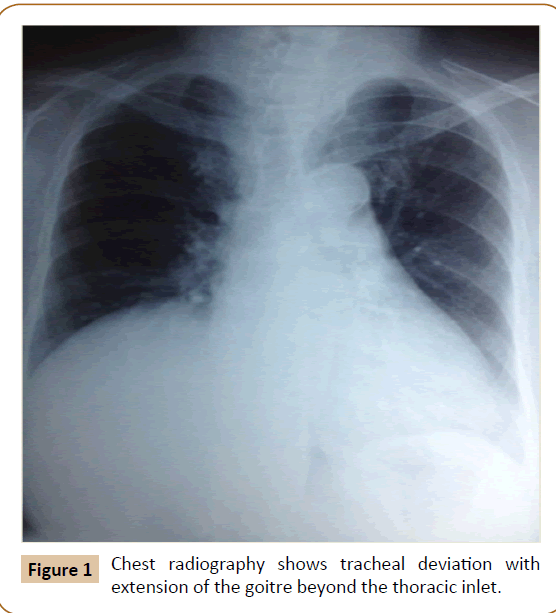
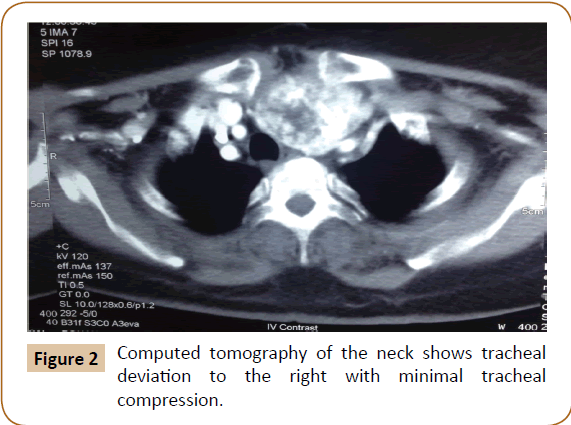
She was referred to an endocrine surgeon when a sizable thyroid swelling was noticeable during physical examination. Symptoms related to the thyroid swelling include recurrent dry cough and feeling of compression to the throat especially while lying down. Further assessment of the goitre revealed subclinical hyperthyroidism and computed tomography (CT) scan of the neck revealed grossly enlarged thyroid gland with multiple nodules predominantly in the left lobe and isthmus. There was tracheal deviation to the right with minimal tracheal compression, and the narrowest diameter of the trachea was 0.8 cm. The enlarged thyroid lobe extended inferiorly 3 cm beyond the thoracic inlet (Figure 1 and Figure 2).
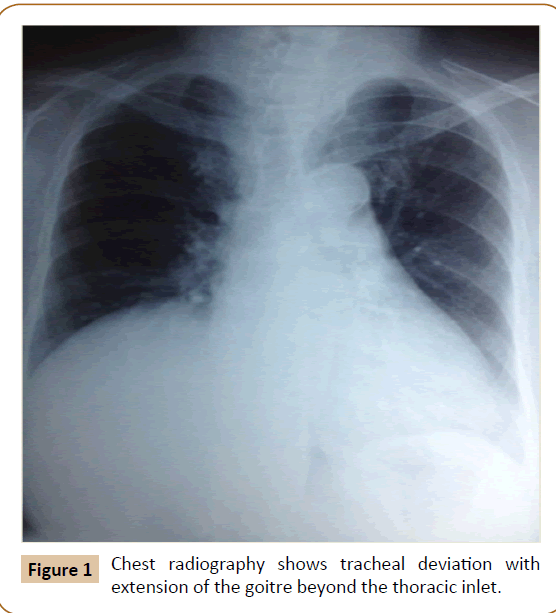
Figure 1: Chest radiography shows tracheal deviation with extension of the goitre beyond the thoracic inlet.
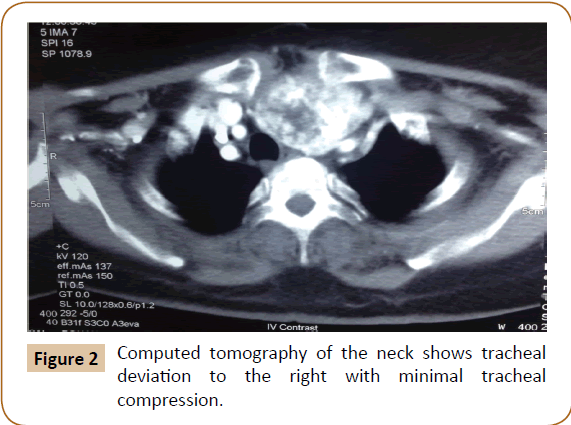
Figure 2: Computed tomography of the neck shows tracheal deviation to the right with minimal tracheal compression.
The case was discussed in a multidisciplinary meeting, and it was decided that the thyroidectomy would be performed together with CABG under the same general anaesthesia. The operation took place in an operation room equipped with cardiopulmonary bypass facility. Total thyroidectomy was performed first through the cervical collar incision. Intraoperative nerve monitoring was used for identification of the laryngeal nerves. Parathyroid glands were identified and preserved. Retrosternal portion of the thyroid gland was successfully removed through the cervical wound. The cervical wound was then packed and a temporary pressure dressing was applied. Heparinization was then commenced. Median sternotomy and triple coronary arterial bypass grafting were performed. After closure of the sternotomy wound, reversal of heparinization with protamine sulphate was undertaken and the cervical wound was again explored in order to secure the haemostasis. There was no bleeding noted from the thyroid bed, but some inconspicuous blood found coming from the chest through a communication between the cervical and the chest wounds. A single drain was inserted to the thyroid bed and the usual two drains to the thoracic cavity. Postoperatively, drainage from the cervical wound was minimal. Thyroxine supplementation was started on the first postoperative day. Both the cervical and thoracic drains were removed in less than a week. No postoperative laryngeal nerve injury or parathyroid insufficiency noted in this patient.
Discussion
Indication for thyroidectomy
To the best of our knowledge, less than 50 cases of combined thyroidectomy and CABG have been reported in the literature. These were mostly reports of an individual case [1-12] and a few small case series [13-15]. In majority of cases, thyroidectomy was performed due to Retrosternal extension or tracheal compression was the main reason why thyroidectomy was performed together with CABG. Two cases reported that airway compromise was not the indication for thyroidectomy. In one case, Grave’s disease the most common reason for thyroidectomy was presence of retrosternal extension or tracheal compression. Other reasons were Grave’s disease and anticipation of amiodarone prescription after cardiac operation.
Excision of the thyroid gland was deemed necessary in our patient as it had been progressively enlarging and compressing on to the trachea. Swallowing and breathing difficulties as well as compression on the major vessels were the expected sequalae. Sudden increase in the size of the goitre could happen unpredictably as a result of internal bleeding or tissue oedema which in turn might lead to an acute upper airway obstruction and endangered patient’s life. Furthermore, she had been diagnosed with subclinical hyperthyroidism, which itself in a long run carried significant risk of morbidities such as compromised cardiovascular functions, decreased bone density, and eventual progression into full blown hyperthyroidism [16].
Should thyroidectomy and CABG performed concurrently?
The literature review reveals that the combined operations were feasible with no serious untoward events related to the procedure or anaesthesia. The reason given on why these two operations were performed concurrently was because both the organs are closely related anatomically so that exposure of one organ would facilitate dissection of the neighbouring organ. Combined operation also means that the two operations were accomplished in a same sitting, thus avoiding a second intervention and unnecessary emotional stress to the patient.
As a convention, In the presence of significant coronary artery disease, the function of the heart should be optimized first before any major non-cardiac surgery can be safely performed. The latter is typically performed once the cardiac function has stabilised which may take a few months, or earlier, depending on the urgency of the latter. Nevertheless, thyroid and heart surgery could be done concurrently when there is a strong need to do so. Our patient had severe tracheal deviation from markedly enlarged thyroid gland. This could lead to serious difficulty in weaning of ventilation and extubation during the postoperative period if the thyroid gland was not removed together with CABG.
Acute airway obstruction due to rapidly enlarging goitre could occur following cardiac operation with cardiopulmonary bypass [17,18]. Cardiopulmonary bypass compromises the upper airway by initiating series of inflammatory responses which ultimately lead to systemic tissue oedema including acute enlargement of the thyroid gland [19,20].
The presence of retrosternal extension in our patient was another reason why the surgeries were performed concurrently. Most of retrosternal goitres can be removed through the cervical incision especially when the thyroid gland is soft and compressible. Nevertheless, the need for sternotomy should not be underestimated. Re-sternotomy would be challenging not only because of scarring but also poses risk of damage to the coronary bypass grafts.
Which operation should be performed first?
Most of the combined operations reported in the literature were in the sequence of thyroidectomy followed by cardiac procedure. Two authors described an initial cardiac procedure through median sternotomy followed by thyroidectomy either through a separate cervical incision [11] or through cervical collar incision in continuity with the sternotomy wound [12]. The postoperative course was uneventful in all reported cases irrespective of the sequence of operations.
As a general principle in surgical practice, whenever a surgical patient have concomitant coronary artery disease, bypass grafting should be performed first in order to minimise risk of perioperative myocardial infarction from the stress of major surgery and its general anaesthesia. However, in a planned combined surgery, such consideration may not be so imperative; as cardiopulmonary bypass could be achieved immediately should it be needed.
Another major consideration is the use of heparinization during cardiac surgery and the bleeding it can cause. Although the heparinization can readily be reversed by protamine sulphate, some residual effect and oozing from raw tissues should be expected. In thyroid operation, preservation of the vital structures i.e. laryngeal nerves and parathyroid glands is the essence of the operation. The crucial element to achieve this is to ensure that the operative field is kept clean and dry at all times, and this could be compromised by the heparinization. This had become the main reason why we performed thyroid surgery first before the CABG.
Furthermore in our patient, since the risk of sternotomy was real although very slim, the same sternotomy wound could be the access for both removal of retrosternal portion of goitre and the subsequent CABG. This preventing from reopening of the sternotomy wound should the cardiac surgery is performed first, thus avoiding damage to the bypass grafts [10].
In conclusion, when combining thyroidectomy and cardiac bypass surgery, performing thyroid dissection before heparinization thus the CABG, could be a wiser decision as it has a better chance in avoiding complications related to the thyroidectomy.
22962
References
- Cetin E, Ozyuksel A, Dalbasi E (2014) Single stage substernal thyroidectomy and off-pump coronary artery bypass grafting: is it worth using cardiopulmonary bypass unless absolutely necessary? BMJ Case Rep 2014: bcr2013201496
- Sjoeholm A, Saxena P, Bunton RW (2012) Combined thyroidectomy and cardiac surgery. J Card Surg 27: 342-344.
- Wexler S, Yamane K, Fisher KW, Diehl JT, Hirose H (2011) Single-stage operation for giant substernal goiter with severe coronary artery disease. Ann Thorac Cardiovasc Surg 17: 524-527.
- Ducos C, Blaise H, Brichon PY, Chavanon O, Chaffanjon PC (2011) Indications for combined thyroidectomy and cardiac surgery. J Visc Surg 148: 321-322.
- Testini M, Poli E, Lardo D, Lissidini G, Gurrado A, et al. (2010) Combined cardiac surgery and total thyroidectomy: Our experience and review of the literature. Thorac Cardiovasc Surg 58: 450-454.
- Mehra AP, Shah KS, Jain PC, Bhansali SK, Sunawala JD, et al. (2009) Combined off-pump coronary artery bypass grafting and thyroidectomy. Ann Thorac Surg 88: 661-663.
- Koçak H, Becit N, Erkut B, Kaygin M (2007) Combined coronary arterial bypass graft and thyroidectomy in a patient with giant goiter: How reliable is it? Thorac Cardiovasc Surg 55: 56-58.
- Tang GH, Feindel CM, Gullane PJ, Butany J (2006) Combined cardiac surgery and excision of a retrosternal thyroid mass: A case report. J Card Surg 21: 281-283.
- Litmathe J, Kurt M, Grabitz K, Knoefel WT, Gams E (2005) Simultaneous coronary artery bypass grafting, replacement of the innominate artery and subtotal thyroidectomy in a 61 year-old patient: A case-report. Chin Med J 118: 699-701.
- Mehta Y, Sujatha P, Juneja R, Singh H, Sachdeva S, et al. (2005) OPCAB and thyroidectomy in a patient with a severely compromised airway. J Cardiothorac Vasc Anesth 19: 79-82.
- Matsuyama K, Ueda Y, Ogino H, Sugita T, Nishizawa J, et al. (1999) Combined cardiac surgery and total thyroidectomy: A case report. Jpn Circ J 63: 1004-1006.
- Daniel SV, Lansdown MR (2012) Combining thyroidectomy with cardiac surgery: Implications for the endocrine surgeon. World J Endoc Surg 4: 43-46.
- Litmathe J, Kurt M, Boeken U, Roehrborn A, Feindt P, et al. (2005) Combined cardiothoracic surgery and interventions of the para/thyroid gland. A rare clinical cooperation. Z Kardiol 94: 28-32.
- Abboud B, Sleilaty G, Asmar B, Jebara V (2003) Interventions in heart and thyroid surgery: Can they be safely combined? Eur J Cardiothorac Surg 24: 712-715.
- Wolfhard U, Krause U, Walz MK, Lederbogen S (1994) Combined interventions in heart and thyroid surgery: An example of interdisciplinary cooperation. Chirurg 65: 1107-1110.
- Donangelo I, Braunstein GD (2011) Update on subclinical hyperthyroidism. Am Fam Physician 83: 933-938.
- Cagli K, Ulas MM, Hizarci M, Sener E (2005) Substernal goiter: An unusual cause of respiratory failure after coronary artery bypass grafting. Tex Heart Inst J 32: 224-227.
- Sajja LR, Mannam GC, Sompalli S, Simhadri CS, Hasan A (2006) Multinodular goiter compressing the trachea following open heart surgery. Asian Cardiovasc Thorac Ann 14: 416-417.
- Edmunds LH Jr (1998) Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg 66: S12-S16.
- Asimakopoulos G, Smith PL, Ratnatunga CP, Taylor KM (1999) Lung injury and acute respiratory distress syndrome after cardiopulmonary bypass. Ann Thorac Surg 68: 1107-1115.