Introduction
Perfect body asymmetry is largely a theoretical concept that seldom exists in living organisms [1]. Asymmetry in the craniofacial areas can be recognized as differences in the size or relationship of the two sides of the face. This may be the result of discrepancies either in the form of individual bones or a malposition of one or more bones in the craniofacial complex. The asymmetry may also be limited to the overlying soft tissues [2].
Several sorts of radiographic measurements have been applied for the quantification of craniofacial asymmetry including linear distances, angles, ratios and side-to-side differences on frontal radiographs or Posteroanterior (PA) cephalogram, orthopantomogram (OPG), 3D imaging such as computed tomography, MRI etc.
Posteroanterior cephalometry has been the most commonly used means to evaluate and measure facial asymmetry since decades. In many areas, the unavailability of 3D imaging still makes the 2D radiographs such as PA cephalogram the basis for diagnosing craniofacial asymmetry. All horizontal lines connecting bilateral cranial landmarks and vertical lines perpendicular to these horizontal lines can adequately serve as reference lines in the analysis of vertical asymmetry from PA cephalograms, if landmark identification error is acceptable [3].
Vertical measurements on panoramic radiograph, within limitations are more accurate than horizontal/ transverse and angular measurements [4]. Subject areas in the literature suggest that OPG can be applied to evaluate vertical posterior mandibular asymmetry [5]. Panoramic radiography is relatively accessible and provides a bilateral view of the mandible, and vertical measurements can be constructed [6-9]. These reports suggested that panoramic radiographs yield acceptable results, are noninvasive, have a favorable cost-benefit relationship, and expose subjects to relatively low doses of radiation [10].
Measurements on panoramic radiographs have been called into question because of considerable methodological errors [11]. Still, some researchers feel that standardized positioning of the head and the use of a bite block reduce most of these distortions [7,8]. Most authors suggest that the reproducibility of vertical and angular measurements is acceptable provided the patientâ€Âââ€Å¾Â¢s head is positioned properly in the equipment [4,12].
Thus, there is an indigence of a valid and reproducible method for assessing facial asymmetry which can be of clinical value in day to day orthodontic practice. Identifying facial asymmetry at an early age in a growing patient can help prevent more disfigurement to the face that would otherwise be attributed by growth as individual approaches adolescence. As orthopantomogram is a routine radiographic record for all orthodontic patients, ruling out asymmetry at any stage during diagnosis and treatment planning is helpful especially at an early age during the growth period. Treating asymmetry at an early age is less traumatic to the patient and easier for clinicians, with growth offering itself as a treatment-augmenting-tool at clinicianâ€Âââ€Å¾Â¢s disposal.
The aim of the current study was-
• To assess and correlate the asymmetry indices in posteroanterior cephalogram and standardized digital orthopantomogram as a tool for diagnosing posterior mandibular asymmetry, and
• To compare and correlate condylar indices using Habetâ€Âââ€Å¾Â¢s and Kjellbergâ€Âââ€Å¾Â¢s formulae.
Materials and Methods
Sample selection
Selection of subjects was based on clinical observation of the gross clinically appreciable facial asymmetry.
Inclusion criteria:
• Age: 18-40 years
• Clinically appreciable facial asymmetry
• Visible chin deviation off the facial midline (>2 mm)
Exclusion criteria
• Patients, already undergoing treatment for asymmetry, not having OPG and PA cephalogram.
• Chin deviation due to functional shift of mandible.
• Asymmetry due to Cyst, tumor, abscess etc. of hard and soft tissues of the face and jaws.
• Cleft lip and palate
• Asymmetry due to muscular hypertrophy unilaterally.
A total of 31 subjects (21 men; 10 women) were selected based on these selection criteria.
Imaging and evaluation of measurements
The procedure was explained to the patients regarding the movement of the tube around the patientâ€Âââ€Å¾Â¢s head while taking panoramic radiograph. Patient was asked to remove the eyeglasses, earrings, dentures, hairpins, etc. Patient can stand erectly in the machine with anterior teeth biting on the bite fork and dorsum of the tongue against the palate. The head was aligned with the mid sagittal plane perpendicular to the floor and the chin was adjusted so that the Frankfurt line stays parallel to the floor. Lateral head stabilizers are used to ensure that the patientâ€Âââ€Å¾Â¢s head is within the optimum focal trough. Lasers for midsagital plane, Frankfurt horizontal plane and vertical canine line were used to position the head within the machinery (Kodak 8000C, Carestream Health Inc. NY, USA). The exposure parameters for orthopantomogram (73 kV, 12 mA, 13.9 seconds) and PA cephalogram (90 kV, 10 mA, 1.00 seconds) were constant for all exposures. All the radiographs were taken by a single operator. Ethical committee of the institution approved the research proposal. Informed consent was given to all the selected subjects for the study regarding the need for PA cephalogram and a routine standardized digital panoramic radiograph.
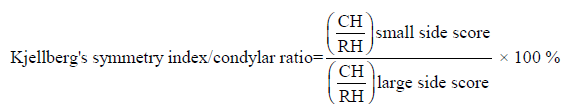
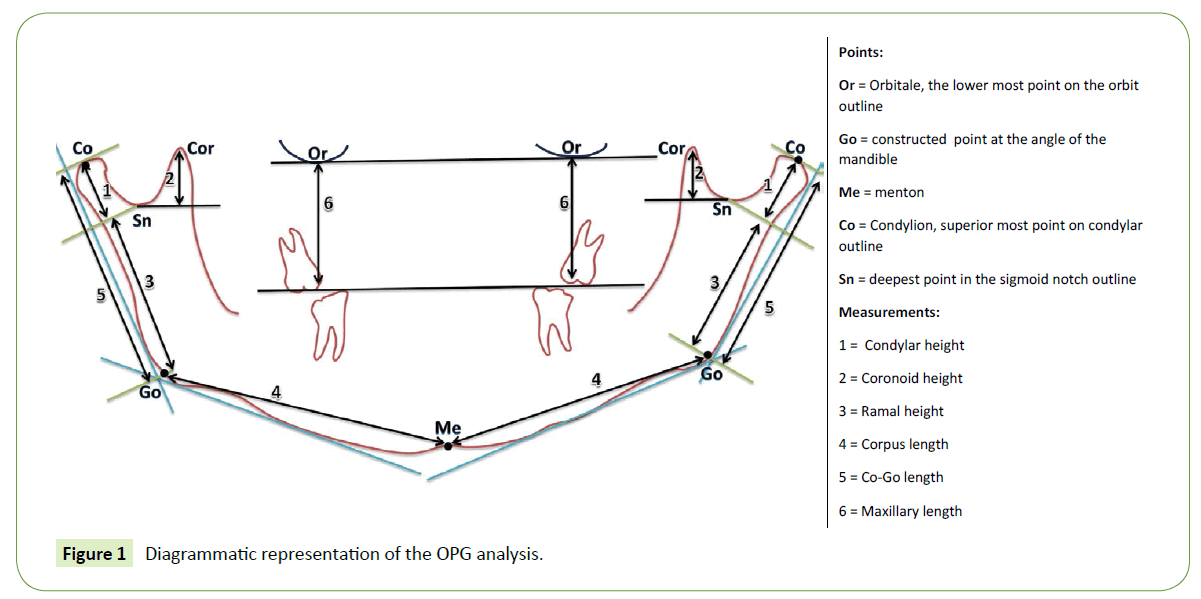
Vertical measurement of condyles, coronoid processes, ramus, Co-Go distance and maxilla were recorded on both sides in orthopantomogram and PA cephalograms shown in Figures 1 and 2. Schematic representations of measurements as described by Habetâ€Âââ€Å¾Â¢s and Kjellberg. Asymmetry index and condylar ratio were drawn for each structure by the following formula:
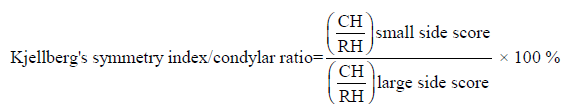
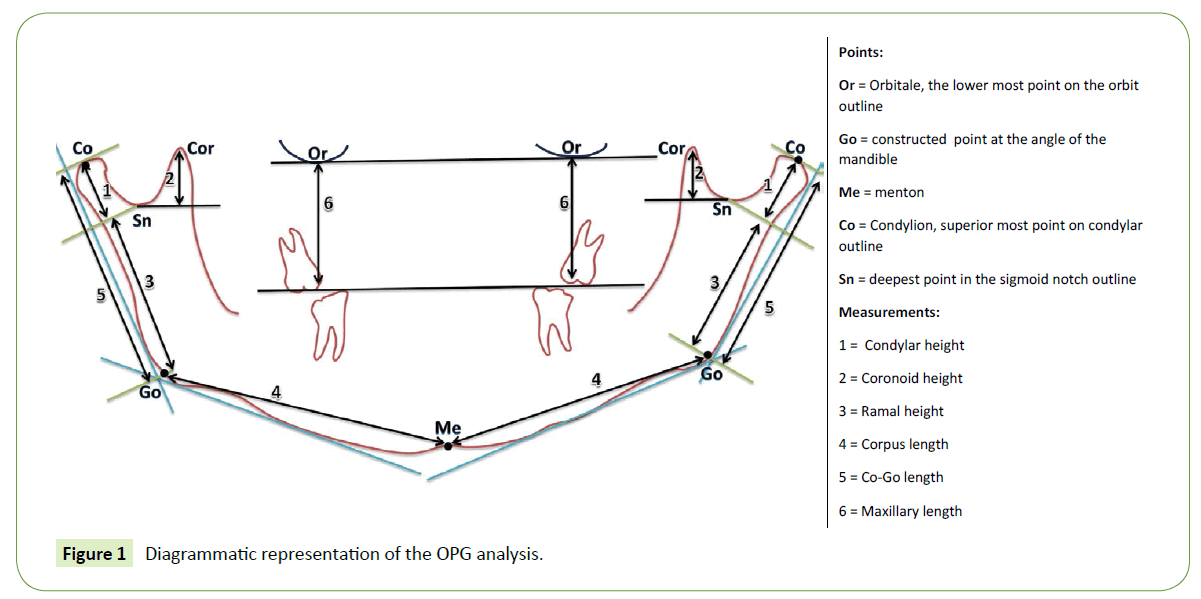
Figure 1: Diagrammatic representation of the OPG analysis.
Figure 2: Diagrammatic representation of PA cephalogram tracing.
Statistical calculations
Data analysis was carried out on a personal computer using the Statistical Package for Social Sciences (SPSS Inc., version 21.0, Chicago, Ill, USA) software for Windows. Descriptive statistics were computed together (Table 1) and separately for both males and females for age and asymmetry indices to investigate relationship between genders (Table 2). Hence, data for both genders were pooled for further analysis. Four weeks after the first measurements, all measurements for determining asymmetry indices were repeated by the same observer and another trained observer separately, on five randomly selected OPG and five PA cephalograms and paired t-test was used to determine statistically significant differences for intra-observer and inter-observer errors (Tables 3 and 4). Test for significant differences between the asymmetry indices from both OPG and PA cephalogram were analysed and conducted using independent t-test (Table 5). Correlation between respective indices from OPGs and PA cephalograms was derived and evaluated for significance (Table 6). Level of significance for all tests was set at <0.05.
| Sr. No. |
Asymmetry Index |
N |
Mean |
Standard error |
Min. |
Max. |
p-value |
| 1 |
Condyle (Habet’s) |
OPG |
31 |
23.59 |
5.92 |
0.00 |
100.00 |
0.697 NS |
| PA cephalogram |
31 |
20.67 |
4.54 |
1.89 |
100.00 |
| 2 |
Condyle (Kjellberg) |
OPG |
31 |
74.20 |
5.92 |
0.00 |
99.80 |
0.422 NS |
| PA cephalogram |
31 |
67.80 |
5.23 |
0.00 |
97.94 |
| 3 |
Ramus |
OPG |
31 |
4.96 |
1.04 |
0.00 |
32.03 |
0.146 NS |
| PA cephalogram |
31 |
7.04 |
0.95 |
0.00 |
19.50 |
| 4 |
Corpus |
OPG |
31 |
5.18 |
0.81 |
0.00 |
17.30 |
0.186 NS |
| PA cephalogram |
31 |
6.94 |
1.04 |
0.93 |
22.02 |
| 5 |
Maxilla |
OPG |
31 |
4.72 |
1.02 |
0.00 |
22.35 |
0.896 NS |
| PA cephalogram |
31 |
4.53 |
0.96 |
0.00 |
21.57 |
| 6 |
Co-Go |
OPG |
31 |
7.19 |
1.50 |
0.00 |
30.59 |
0.965 NS |
| PA cephalogram |
31 |
7.28 |
1.37 |
0.00 |
28.14 |
NS- Non-significant
Table 1: Comparison of different facial asymmetry indices derived from OPG and PA cephalogram.
| Parameters tested |
Mean Values |
p-value |
Sig. |
| Males (n=21) |
Females (n=10) |
| Age (years) |
21.29 |
19.53 |
0.165 |
NS |
| Condyle Index |
OPG |
27.6 |
15.17 |
0.334 |
NS |
| (Habet’s formula) |
PA cephalogram |
23.34 |
15.07 |
0.404 |
NS |
| Condylar ratio |
OPG |
71.09 |
80.71 |
0.457 |
NS |
| (Kjellberg’s formula) |
PA cephalogram |
65.02 |
73.63 |
0.451 |
NS |
| Ramus Index |
OPG |
5.64 |
3.53 |
0.353 |
NS |
| (Habet’s formula) |
PA cephalogram |
6.86 |
4.57 |
0.788 |
NS |
| Corpus Index |
OPG |
5.55 |
4.39 |
0.509 |
NS |
| (Habet’s formula) |
PA cephalogram |
7.8 |
5.12 |
0.231 |
NS |
| Maxilla Index |
OPG |
4.98 |
4.16 |
0.717 |
NS |
| (Habet’s formula) |
PA cephalogram |
4.56 |
4.48 |
0.969 |
NS |
| Co-Go Index |
OPG |
8.49 |
4.46 |
0.214 |
NS |
| (Habet’s formula) |
PA cephalogram |
7.97 |
5.85 |
0.48 |
NS |
NS = non-significant (p>0.05)
Table 2: Comparison of mean values of age and asymmetry indices between male and female subjects.
| Sr. No. |
Asymmetry Index |
n |
Correlation coefficient |
Significance     (2-tailed) |
| 1 |
Condyle (Habet’s formula) |
OPG |
31 |
0.894 |
0.000** |
| PA cephalogram |
31 |
| 2 |
Condyle ratio (Kjellberg’s formula) |
OPG |
31 |
0.709 |
0.000** |
| PA cephalogram |
31 |
| 3 |
Ramus
(Habet’s formula) |
OPG |
31 |
0.418 |
0.019* |
| PA cephalogram |
31 |
| 4 |
Corpus
(Habet’s formula) |
OPG |
31 |
0.242 |
0.189 |
| PA cephalogram |
31 |
| 5 |
Maxilla
(Habet’s formula) |
OPG |
31 |
0.757 |
0.000** |
| PA cephalogram |
31 |
| 6 |
Co-Go distance
(Habet’s formula) |
OPG |
31 |
0.857 |
0.000** |
| PA cephalogram |
31 |
*- p< 0.05 (statistically significant correlation) **- p< 0.0001 (highly statistically significant correlation)
Table 3: Pearson correlation coefficient of asymmetry indices derived from OPG and PA cephalogram and their significance levels.
| Sr. No. |
Asymmetry Index |
n |
Correlation coefficient |
Significance     (2-tailed) |
| 1 |
Condyle (Habet’s formula) |
OPG |
31 |
0.894 |
0.000** |
| PA cephalogram |
31 |
| 2 |
Condyle ratio (Kjellberg’s formula) |
OPG |
31 |
0.709 |
0.000** |
| PA cephalogram |
31 |
| 3 |
Co-Go distance
(Habet’s formula) |
OPG |
31 |
0.857 |
0.000** |
| |
|
|
|
|
Table 4: Pearson correlation coefficient of asymmetry indices derived from OPG and PA cephalogram and their significance levels.
| Sr. No. |
Asymmetry Index |
Radiograph |
Correlation coefficient |
Sig. |
T |
Sig. (2-tailed) |
| 1 |
Condyle (Habet’s) |
OPG |
0.986 |
0.002 |
1.224 |
0.288 |
| PA cephalogram |
0.994 |
0.006 |
-1.399 |
0.256 |
| 2 |
Condyle (Kjellberg) |
OPG |
0.999 |
0.000 |
-1.114 |
0.328 |
| PA cephalogram |
0.999 |
0.000 |
2.643 |
0.057 |
| 3 |
Co-Go distance
(Habet’s) |
OPG |
0.998 |
0.000 |
1.011 |
0.369 |
| PA cephalogram |
0.992 |
0.001 |
-0.738 |
0.514 |
| |
Overall |
OPG |
0.972 |
0.000 |
-2.047 |
0.050 |
| PA cephalogram |
0.971 |
0.000 |
1.149 |
0.262 |
Table 5: Intra-observer error with paired t-test results and correlation coefficients.
| Sr. No. |
Asymmetry Index |
Radiograph |
Correlation coefficient |
Sig. |
t |
Sig. (2-tailed) |
| 1 |
Condyle (Habet’s) |
OPG |
0.921 |
0.026 |
0.740 |
0.501 |
| PA cephalogram |
0.989 |
0.011 |
1.932 |
0.149 |
| 2 |
Condyle (Kjellberg) |
OPG |
0.998 |
0.000 |
-0.372 |
0.729 |
| PA cephalogram |
0.999 |
0.000 |
5.887 |
0.004 |
| 3 |
Co-Go distance
(Habet’s) |
OPG |
0.993 |
0.001 |
0.132 |
0.901 |
| PA cephalogram |
0.963 |
0.037 |
-1.337 |
0.274 |
| |
Overall |
OPG |
0.923 |
0.000 |
-1.498 |
0.145 |
| PA cephalogram |
0.940 |
0.000 |
-0.970 |
0.342 |
Table 6: Inter-observer errors with paired t-test results and correlation coefficients.
Results
The condyle asymmetry index was the highest amongst all the observed variables (23.59 ± 5.92 for OPG and 20.67 ± 4.54 for PA cephalogram). No statistically significant differences in asymmetry indices were found between OPG and PA cephalogram (Table 1). Mean age for male and female subjects was 21.29 ± 4.35 and 19.53 ± 2.96 years respectively. There was no statistically significant difference between the genders regarding the age or indices. (p>0.05) (Table 2). To further explore the statistical relationship of similarities between the asymmetry indices OPG and PA cephalogram, correlation coefficients and significance of the correlation were computed. There was positive correlation between all indices measured from the PA cephalogram and OPG (Table 3). Asymmetry indices for the condyle and Co-Go distance and condylar ratio (Kjellberg) derived from OPG were found to be statistically highly significantly correlated with those derived from PA cephalogram (p< 0.01). Intra-observer and interobserver errors were within 0.809 to 0.997. The magnification and distortion factors are shown in Table 4 for right and left sides, which showed no asymmetric enlargement or asymmetric shortening of bilateral wire markers. Habetâ€Âââ€Å¾Â¢s and Kjellbergâ€Âââ€Å¾Â¢s indices correlated significantly negatively with each other (Table 5).
Discussion
The present study was undertaken to evaluate, compare and correlate the asymmetry indices derived from linear measurements of mandibular posterior region on PA cephalogram and orthopantomogram .
The patients were selected based on the gross facial asymmetry and clinically appreciable chin deviation on clinical examination, who required PA cephalogram for the evaluation of facial asymmetry. The reason why we selected the subjects with >2 mm was because, according to a criterion used previously [13,14], chin deviation of more than 2 mm was considered asymmetric.
Since orthopantomogram is more routinely prescribed radiograph in orthodontic practice, the shape of mandibular ramus and condyle etc. on both sides can be grossly compared at a primary level [15]. On the other hand, cephalometric PA projection is a valuable tool for estimating asymmetry between right and left structures, since they are located at equal distances from the film and X-ray source [16].
In most cases, the presence and degree of facial asymmetry can be diagnosed by PA cephalogram [17-19]. Since this projection has been the conventional radiograph for evaluating the facial asymmetry for decades, it is interesting to compare the asymmetry derived from PA cephalogram and orthopantomogram. The purpose of the present study was to evaluate and compare the asymmetry indices derived from various linear measurements from panoramic radiograph and PA cephalogram in patients exhibiting gross facial asymmetry. The aim of the study was to see if orthopantomogram can be routinely used to assess the facial asymmetry as a screening aid for orthodontic patients. This would be particularly beneficial to the growing orthodontic patients, in whom developing asymmetry can be intercepted and prevented from further worsening and also in cases of subclinical asymmetry which may be masked by soft tissues or otherwise.
Linear measurements from both the radiographs contain distortion and magnification in different regions of the imaged areas, more so in case of panoramic radiographs. Hence, it would have been unreasonable to compare the linear measurements from both the radiographs. Some authors [20,21] have suggested the use of ratio over the linear dimensions especially in radiographs where chances of inherent errors like distortion, magnification either due to projection geometry or due to patient positioning, shadows the accuracy in determining the right left differences or asymmetry. With respect to panoramic radiographs, Van Eslande [20] stated that by using the ratio, condylar height asymmetries can be identified. According to Kjellberg [21], the ratio is not affected by positioning error, distortion, or magnification in panoramic images. Hence, asymmetry index was used to quantify asymmetry in the present study.
Vertical measurements on orthopantomogram are relatively more reliable [22-24] and may be used if patient positioning is accurate [4,25] Mawani et al. [26] reported greater magnification in horizontal dimension than in vertical dimension in assessing the condylar shape on digital panoramic images of dry skulls. According to Larheim et al. [4], horizontal measurements have been reported to be unreliable because of the variation in magnification factor.
According to Graber, the magnification of orthopantomogram is uniform and should not materially affect the diagnostic decision [27]. The magnification errors were reduced by accurate and reproducible patient positioning. Besides all these precautions, all the radiographs were taken by a single operator to reduce the inconsistency in patient positioning. Magnification factor was further checked by evaluating the distortion factor in vertical and horizontal plane by using stainless steel wire on a dry skull. The distortion factors are shown in Table 7. For both right and left sides which showed no asymmetric enlargement or asymmetric shortening of the bilateral wire markers. The magnification factor was derived from dividing the radiographic length of the wire marker by the actual length of the wire marker. The distortion factor was lower (Table 7) than the distortion factor mentioned by the manufacturer (1.27 for OPG and 1.14 for PA cephalogram) for both orthopantomogram and PA cephalogram. This is in accordance with the previous studies [5,28]. Although there was some distortion affecting the absolute linear dimensions, the asymmetry indices being a ratio did not get influenced because there was no asymmetric distortion of the wire makers placed bilaterally in our investigation. Thus, correction factors to account for projective errors in panoramic images or PA cephalograms were not required. This was further checked on the patients being radiographed by stainless steel markers of the same length attached on the side of the face on ramus and body regions. Two radiographs exhibiting asymmetric distortion were excluded from the study.
| Distortion factor |
| Right side |
Left side |
| Vertical wire marker |
Horizontal wire marker |
Vertical wire marker |
Horizontal wire marker |
| PA |
OPG |
PA |
OPG |
PA |
OPG |
PA |
OPG |
| 1.04 |
1.16 |
0.20 |
1.02 |
1.04 |
1.16 |
0.20 |
1.02 |
Table 7: Magnification /distortion factors for wire markers on dry skull.
The patientsâ€Âââ€Å¾Â¢ names were masked on the radiographs and were coded. Thus, operatorâ€Âââ€Å¾Â¢s bias was reduced by blinding the investigator who traced the radiographs and evaluated asymmetry.
Our indices were relatively higher than other similar studied [29-34] with respect to condyle or Co-Go distance. This may be attributed to the sample characteristics. Our sample being constituted of gross facial asymmetry was expected to give higher values of asymmetry indices.
Table 3 shows no statistically significant difference between orthopantomogram and PA cephalogram for all the indices measured.
There was a statistically significant (positive) correlation between the asymmetry indices of condyle (Habetâ€Âââ€Å¾Â¢s and Kjellbergâ€Âââ€Å¾Â¢s), ramus, Co-Go, and maxilla, measured from the PA cephalogram and orthopantomogram. These asymmetry indices were derived from vertical linear measurements, hence were more accurate on orthopantomogram as has been shown by various studies [5-8], while asymmetry indices of mandibular corpus was not found to be significantly correlated between orthopantomogram and PA cephalogram. That might be because of the fact that horizontal parameters are not that accurate on orthopantomogram when asymmetry indices are calculated and compared.
Correlation between linear measurements from digital orthopantomogram and direct anatomic measurements was investigated by Turp et al. [35]. Low correlation was found for condylar height, ramus and Co-Go distance in their study. In contrast, we investigated the asymmetry indices derived from the same linear measurements from digital orthopantomogram and PA cephalogram and found high correlation between two radiographs for all three measurements.
To the best of our knowledge, there is no study in the literature till date that attempted to evaluate the asymmetry indices in the PA cephalogram and compare them with the panoramic radiograph. However, attempt has been made to compare the PA cephalogram to CBCT images of dry asymmetric skulls by Damstra et al. [36]. We found highly significant correlation between Co-Go and maxilla between orthopantomogram and PA cephalogram. Damstra et al. [36] also found highly significant correlation for linear measurement of Co-Go and maxilla (Or-U6) between CBCT and PA cephalogram.
Condylar ratio (Kjellbergâ€Âââ€Å¾Â¢s) and asymmetry index (Habetâ€Âââ€Å¾Â¢s) in the present study showed highly significant correlation between PA cephalogram and orthopantomogram, whereas Kambylafkas [17] found poor correlation of condylar height index between digital orthopantomogram and laminograph. However, the correlation was highly significant with respect to the total ramal height, similar to present study (Table 8).
| Condyle asymmetry |
Habets’ method (%) |
Kjellberg’s method (%) |
p-value (t-test) |
Correlation |
Significance |
| OPG |
23.59 |
74.20 |
0.000* |
-0.986 |
0.000* |
| PA cephalogram |
20.67 |
67.80 |
0.000* |
-0.907 |
0.000* |
*- p< 0.0001 (statistically highly significant)
Table 8: Comparison of Habetâ€Âââ€Å¾Â¢s and Kjellbergâ€Âââ€Å¾Â¢s method for assessing condylar asymmetry.
In another study, the condylar asymmetry index was also found to have low correlation when digital orthopantomogram and direct anatomic measurements were compared [37], however high correlation was found for the Co-Go distance/total ramal height asymmetry index in this study, which is in accordance with our study.
Further studies are needed to verify the accuracy and reliability of conventional panoramic radiographs by comparing them with the three-dimensional data which is the current gold standard for the accurate diagnosis. If found accurate, in specific regions, practitioners can be confident that they can use the conventional panoramic image to assess that specific area and that they are not disillusioned by the image distortion or magnification. Early detection of skeletal asymmetry in the growing patients gives an opportunity for interceptive therapy that can improve the long term treatment outcomes. Moreover, 2D images are more easily shared among the practitioners with greater ease than the 3D data which require special software to be viewed and patient is spared from more radiation exposure of tomography.
Conclusions
• Condyle, ramus, Co-Go distance, and maxilla asymmetryindices and condylar ratio derived from vertical measurements correlated highly significantly between OPG and PA cephalogram.
• Habetâ€Âââ€Å¾Â¢s asymmetry index and Kjellbergâ€Âââ€Å¾Â¢s condylar ratio correlated significantly negatively with each other.
• Thus, asymmetry indices can be calculated from OPG in vertical dimension for mandibular posterior regions. However, clinician should be aware of the distortion of a radiographic machine before evaluation of measurements.
17734
References
- Bishara SE, Burkey PS, Kharouf JG (1994) Dental and facial asymmetries: a review. Angle Orthod 64: 89-98.
- Sutton PR (1968) Lateral facial asymmetry-methods of assessment. Angle Orthodontist 38: 82-92.
- Trpkova B, Major P, Nebbe B, Prasad N (2003) Craniofacial Asymmetry and temporomandibular joint internal derangement in female adolescents: A posteroanteriorcephalometric study. Am JOrthodDentofacialOrthop123: 512-520.
- Larheim TA, Svanaes DB (1986) Reproducibility of rotational panoramic radiography: mandibular linear dimensions and angles. Am J OrthodDentofacialOrthop 90: 45-51.
- Kambylafkas P, Kyrkanides S, Tallents RH (2006) Mandibular asymmetry in adult patients with unilateral degenerative joint disease. Angle Orthod76: 388-393.
- Wabeke KB, Spruijt RJ, Habets LL (1995) Spatial and morphologic aspects of temporomandibular joints with sounds. J Oral Rehabil22: 21-27.
- Habets LL, BezuurJN, van OoijCP, Hansson TL (1987)Theorthopantomogram, an aid in diagnosis of temporomandibular joint problems. I. The factor of vertical magnification. J Oral Rehabil14: 475-480.
- Habets LL, BezuurJN, Naeiji M, Hansson TL (1988) The Orthopantomogram an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J Oral Rehabil15: 465-471.
- BezuurJN, Habets LL, Hansson TL (1989) The recognition of craniomandibular disorders, Rehabil., condylar symmetry in relation to myogenous and arthrogenous origin of pain. J Oral Rehabil16: 257-260.
- Yanez-VicoRM, Iglesias-Linares A, Torres-Lagares D (2010) Diagnosis of the craniofacialasymmetry. Literature review. Med Oral Patol Oral Cir Bucal 15: e494-e498.
- Larheim TA, Johannessen S, Tveito L (1988) Abnormalities of the temporomandibular joint in adults with rheumatic disease. A comparison of panoramic, transcranial and transpharyngeal radiography with tomography. DentomaxillofacRadiol17: 109-113.
- Larheim TA, Svanaes DB, Johannessen S (1984) Reproducibility of radiographs with the Orthopantomograph 5: Tooth length assessment. Oral Surg Oral Med Oral Pathol58:736-741.
- SevertTR, ProffitWR (1997)The prevalence of facial asymmetry in the dentofacial deformities population at the university of north Carolina. Int J AdutOrthodonOrthognathSurg7: 31-34.
- Haraguchi S, Takada K, Yasuda Y (2002) Facial asymmetry in subjects with skeletal class III deformity. Angle Orthod72: 28-35.
- Cheong YW, Lo LJ (2011) Facial asymmetry: etiology, evaluation and management. Chang Gung Med J 34:341-351.
- GrummonsDC, Kappeyne van de Coppello MA (1987) A frontal asymmetry analysis. J ClinOrthod21:448-465.
- Hwang HS, Lee KH, Park JY, Kang BC, Park JW, et al. (2004) Development of posteroanteriorcephalometric analysis for the diagnosis of facial asymmetry. J Korean Dent Assoc42:219-231.
- Letzer GM, KronmanJH (1967) A posteroanteriorcephalometric evaluation of craniofacial asymmetry. Angle Orthod37:205-211.
- Van Eslande DC, Russell SJ, Flores-Mir C (2008) Mandibular asymmetry diagnosis with panoramic imaging.Am J OrthodDentofacialOrthop 134: 183-192.
- Kjellberg H, Ekestubbe A, Kiliaridis S, Thilander B (1994) Condylar height on panoramic radiographs. A methodologic study with a clinical application. ActaOdontolScand 52:43-50.
- Tronje G, WelanderU, McDavidWD, Morris CR (1981) Image distortion in rotational panoramic radiography. IV. Object morphology, outer contours. ActaRadiolDiagn (Stockholm) 22:689-696.
- Ericsson S, Lundberg M (1967) Alterations in the temporomandibular joint at various stages of rheumatoid arthritis. ActaRheumatolScand13:257-274.
- LasterWS, Ludlow JB, Bailey LJ, Garl H, Hershey H (2005) Accuracy of measurements of mandibular anatomy and prediction of asymmetry in panoramic radiographic images. DentomaxillofacRadiol34:343-349.
- Tronje G, Eliasson S, Julin P, Welander U (1981) Image distortion in rotational panoramic radiography. II. Vertical distances. ActaRadiolDiagn (Stockh) 22:449-455.
- Mawani F (2003)The anatomic accuracy of lateral temporomandibular joint images from axially corrected multidirectional tomography and three panoramic radiography units: a comparative dry skull study [masterÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¾ÃÂâs thesis]. Edmonton AB: university of Alberta.
- Graber TM (1967)Panoramic radiography in orthodontic diagnosis. Am J Orthod53: 799-821.
- Pirttiniemi P, Kantomaa T, Lahtela P (1990) Relationship between craniofacial and condyle path asymmetry in unilateral cross-bite patients. Eur J Orthod12: 408-413.
- Kurt G, Uysal T, Sisman Y, Ramoglu SI (2008) Mandibular asymmetry in class II subdivision malocclusion. Angle Orthod 78:32-37.
- Saglam AM (2003)Theconsylar asymmetry measurements in different skeletal patterns. J Oral Rehabil30:738-742.
- Kiki A, Kilic N, Oktay H (2007) Condylar asymmetry in bilateral posterior crossbite patients. Angle Orthod 77:77-81.
- BiavatiFS, Ugolini A, Laffi N, Canevello C, Biavati AS (2014) Early diagnostic evalulation of mandibular asymmetry using orthopantomogram. Indian J Dent Res 25:154-159.
- Halicioglu K, Celikoglu M, Buyuk SK, Sekerci AE, Candirli C (2014) Effects of early unilateral mandibular first molar extraction on condylar and ramal vertical asymmetry. Eur J Dent 8:178-183.
- Saglam AA, Sangli G (2004) Condylar asymmetry measurements in temporomandibular disorders. J Contemp Dent Pract 5:59-65.
- TurpJC, Vach W, Strub JR, Harbich K, Alt KW (1995) The recognition of mandibular asymmetries in the panoramic tomogram. An example of the need for judging the value of a diagnostic procedure. SchweizMonatsschrZahnmed105:755-759.
- Damstra J, Fourie Z,Ren Y (2013) evaluation and comparison of postero-anterior cephalograms and cone-beam computed tomography images for the detection of mandibular asymmetry. EurJ Orthod35: 45-50.
- Boratto R, Gambardella U, Micheletti P, Pagliani L, Preda L (2002) Condylar-Mandibular asymmetry, A reality. Bull Group IntRechSciStomatolOdontol 44:52-56.