Aim of the study: Evaluation of the accuracy and agreement of trans rectal ultrasound and MRI in preoperative staging of rectal carcinoma in comparison with postoperative histopathology.
Background: Accurate staging of rectal carcinoma is an important issue in preoperative planning for the management.
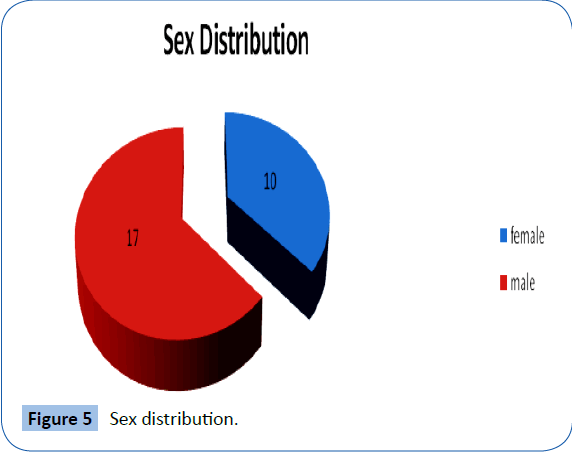
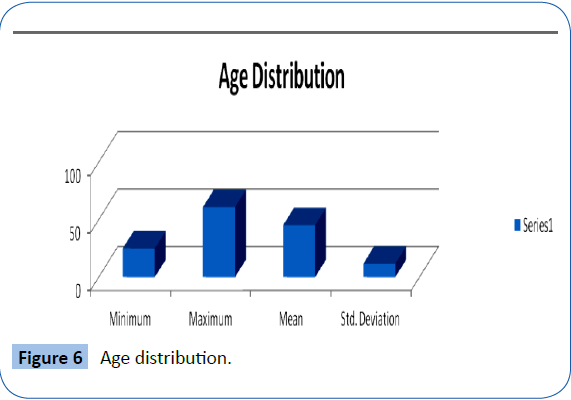
Patients and methods: Twenty seven patients, 17 males and 10 females were included in the study their ages ranging between 25 to 65 years. These patients were diagnosed by PR, colonoscopy and histopathology to have rectal carcinoma. Preoperative MRI and trans rectal ultrasound were done. Rectal wall invasion (T stag), lymph node status (N stag), relation of the tumor to the anal sphincter complex and circumferential resection margin (CRM) were assessed by MRI and trans rectal U/S. The imaging results were compared with the histopathology regarded as the gold standard of the local staging.
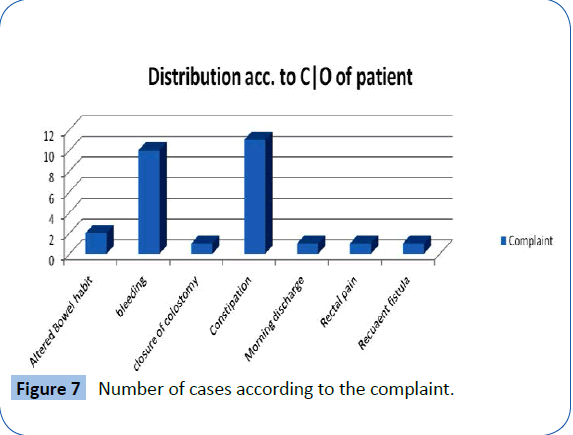
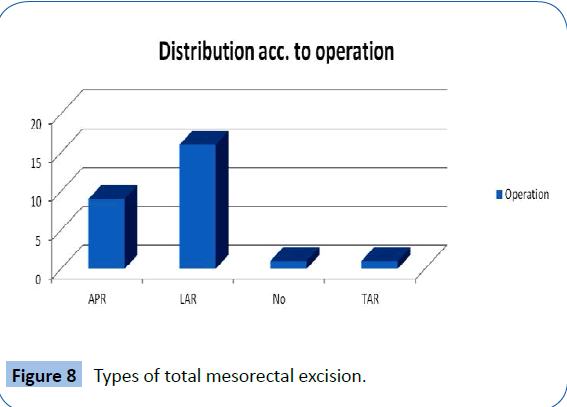
Results: Constipation was the mean complaint in 11 cases, bleeding in 10 cases. Low anterior resection was done in 16 cases; abdominoperineal resection was done in 9 cases. Neoadjuvant was taken in 13 cases for down staging. Comparison between U/S and histopathology in rectal wall invasion and lymph nodes is statistically significant (p value >0.005). Comparison between MRI and histopathology in rectal wall invasion is statistically insignificant (p value = 0.999) in contrary to the lymph node status p value is >0.005. Comparison between MRI and U/S in rectal wall invasion and lymph node status is statistically significant (p value >0.001).
Conclusion: Trans rectal U/S and MRI rectum and anal canal are complementary for proper preoperative local staging of rectal cancer.
Keywords
Rectal Carcinoma, Trans Rectal Ultrasound, Magnetic Resonance Imaging and Neoadjuvant Chemoradiotherapy
Introduction
Colorectal cancer is one of the common cancers worldwide. About 30-40% of colorectal carcinoma arises from the rectum [1]. After the wide acceptance of down staging in rectal carcinoma (neoadjuvant chemoradiotherapy) the preoperative accurate staging became an important issue [2]. Stag 1 tumors are best treated with surgery whereas stag 2 and 3 may require preoperative chemoradiotherapy [3]. Trans rectal ultrasound (TRUS) and MRI are the imaging of choice in preoperative staging [4]. Trans rectal U/S and MRI are complementary methods in accurate preoperative staging of rectal carcinoma [5]. The prognosis of rectal cancer is depending on depth of tumour invasion (T stag), CRM, number of the lymph nodes infiltrated (N stag), lymphovascular invasion, tumour grad and distant metastasism [6]. Our goal is to assess the accuracy and agreement between the Trans rectal U/S and MRI in preoperative local staging of rectal cancer.
Patients and Methods
The study was conducted on 27 patients 17 males and 10 females presented to kasr Alainy hospitals general surgery outpatient clinic from 2012 to 2015. All the patients were diagnosed to have rectal carcinoma by colonoscopy and rectal biopsy. All the patients were informed about the study and written consent were signed by all the patients included in the study. Patients with non-neoplastic masses, recurrent rectal cancer, obstructing rectal lesions and patients were not singed the consent were excluded from the study. All the patients underwent full history taking, general and local examinations including digital rectal examination. Colonoscopy and rectal biopsy were done and histopathological examination was done to prove malignancy. Routine laboratory tests (CBC, liver and kidney functions, and coagulation profile and tumour markers) were done. Preoperative local staging was done by trans rectal U/S and MRI (Figures 1-3). Trans rectal U/S was performed in both 2D and 3D images using the BK medical U/S device in the kasr Alainy colorectal unite. The technique was done on outpatient bases. One or two rectal enemas were done by the patients to evacuate the rectum before the test. The test was performed while the patients in the left lateral position with or without sedation. The probe was lubricated with water soluble gel and gently introduced in the anal canal. The BK medical U/S device has a built in 3D automatic motorized system. 2D and 3D images were taken. Assessment of the T, N stags by U/S. MRI was done with no special preparation. The patients were informed about the most important item which was the spasmolytic agent to reduce the incidence of artifact due to bowel motions. The position was the supine position. T1 and T2 weighted MRI images were taken. Site of the tumor, T, N and CRM were assessed by MRI.
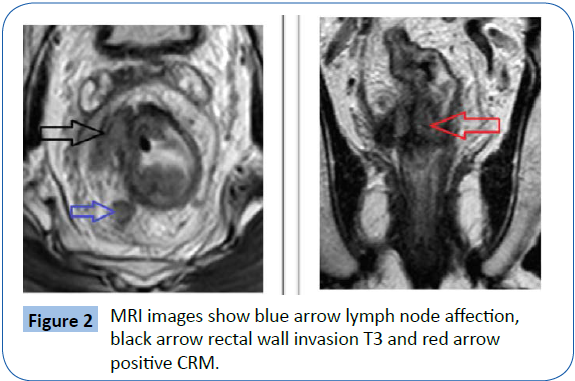
Figure 1: 2D U/S images show red arrow lymph node affection, white arrow rectal wall invasion T3 and blue arrow positive CRM.
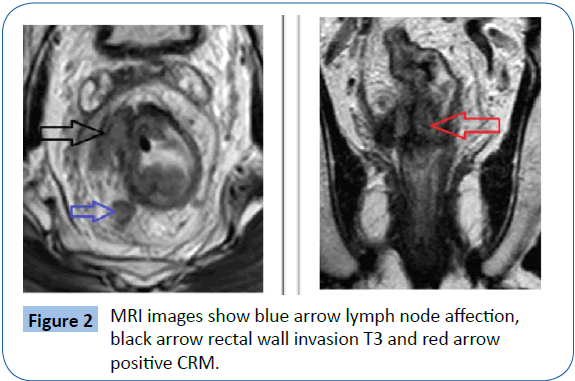
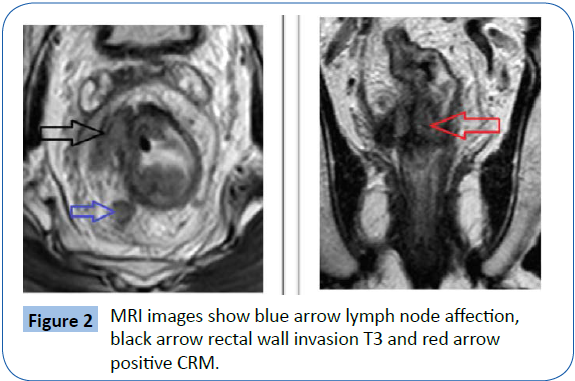
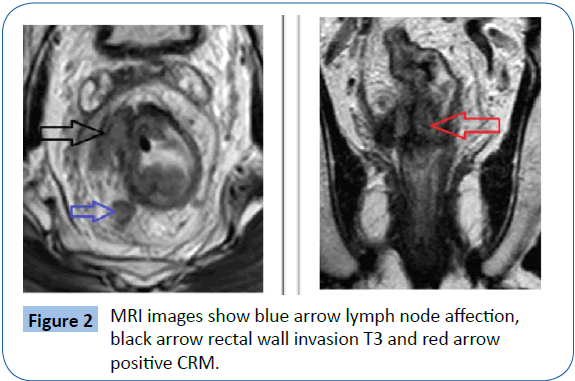
Figure 2: MRI images show blue arrow lymph node affection, black arrow rectal wall invasion T3 and red arrow positive CRM.
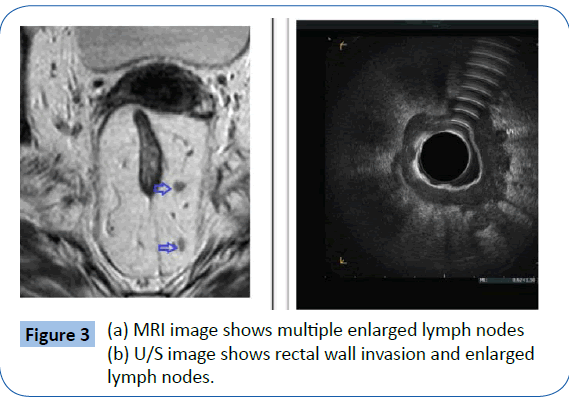
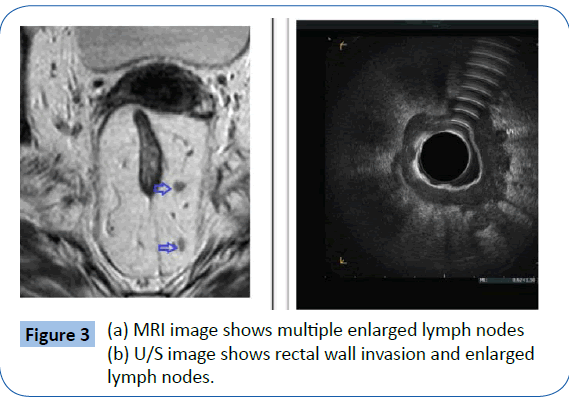
Figure 3: (a) MRI image shows multiple enlarged lymph nodes (b) U/S image shows rectal wall invasion and enlarged lymph nodes.
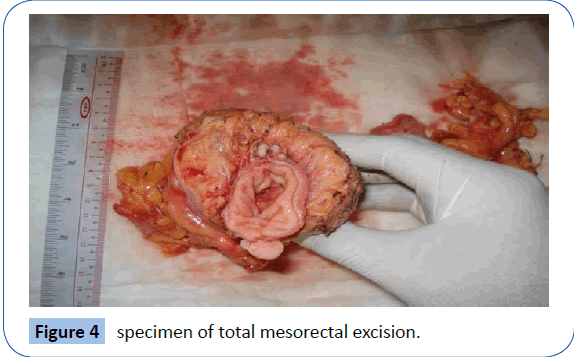
After proper preoperative staging, patients with stag 1 and 2 underwent surgery while patients with stag 3 and 4 received neoadjuvant therapy. During surgery, exploration was done first for operability (peritoneal nodules, liver metastasis and or omental affection) and irresectability. Operations done was total mesorectal excision including figure 4 low anterior resection, ultralow anterior resection with sphincter saving or abdominoperineal resection. These procedures were done open or laparoscopic or single incision laparoscopic surgery (SILS).
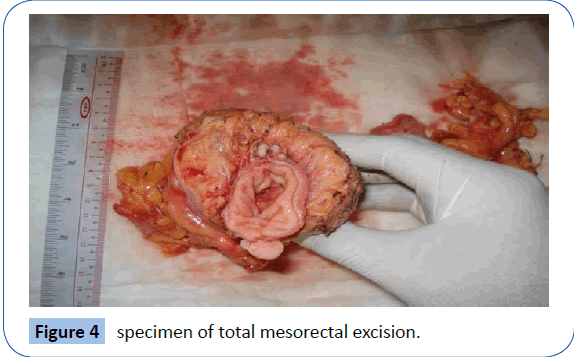
Figure 4: specimen of total mesorectal excision.
The specimen was sent for histopathological examination. Results of histopathology included the rectal wall invasion, the lymph nodes status, the circumferential resection margin and lymphovascular invasion. Data were statistically described in terms of mean ± standard deviation (± SD), and range, or frequencies (number of cases) and percentages when appropriate. Agreement between TRUS and MRI was done using kappa statistic. p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) release 15 for Microsoft Windows (2006).
Results
Demographic results (Figures 5-13)
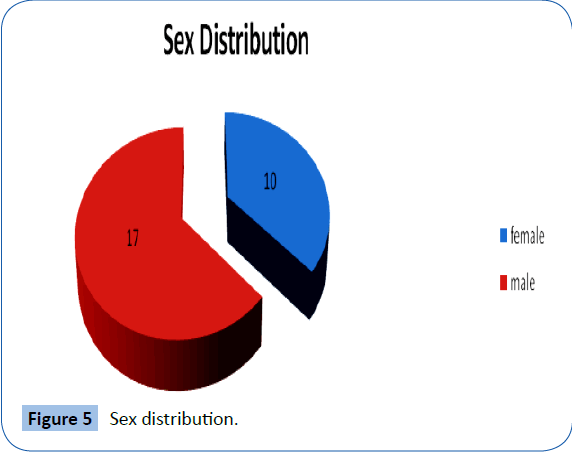
Figure 5: Sex distribution.
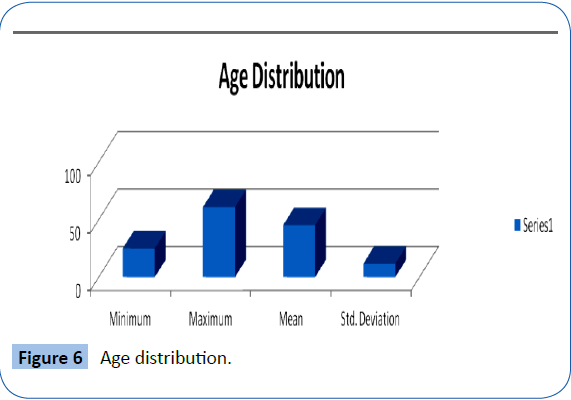
Figure 6: Age distribution.
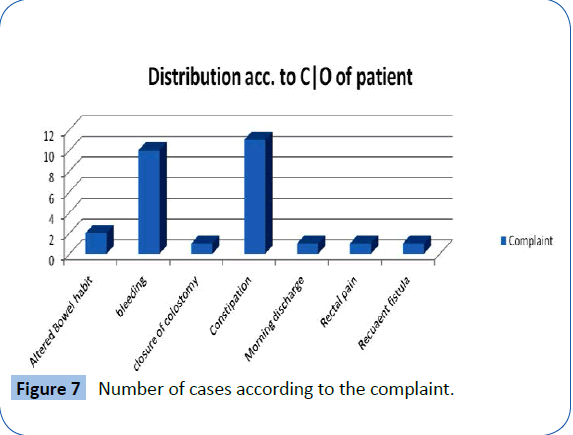
Figure 7: Number of cases according to the complaint.
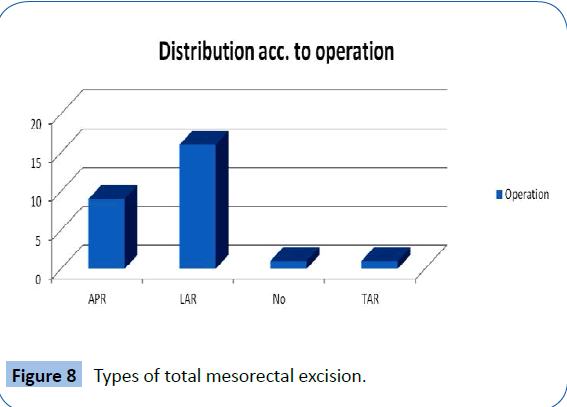
Figure 8: Types of total mesorectal excision.
Figure 9: Neoadjuvant treatment Statistical data.
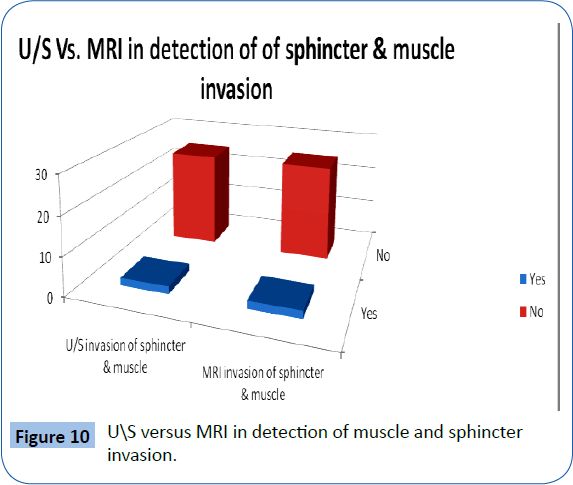
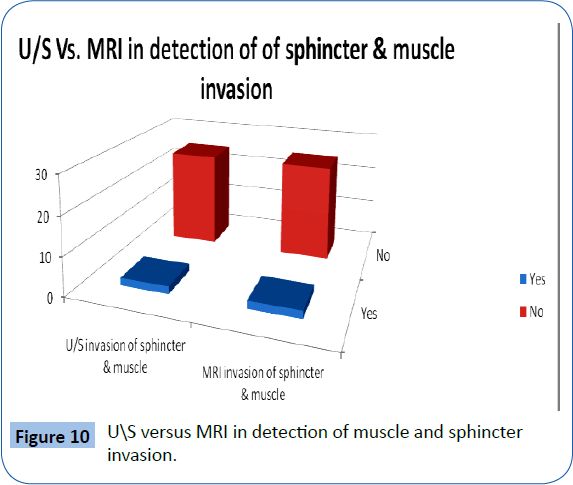
Figure 10: US versus MRI in detection of muscle and sphincter invasion.
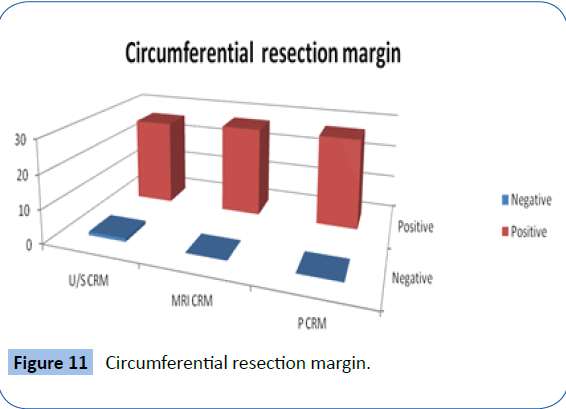
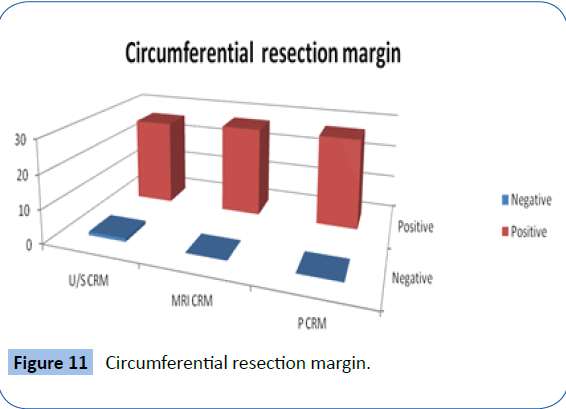
Figure 11: Circumferential resection margin.
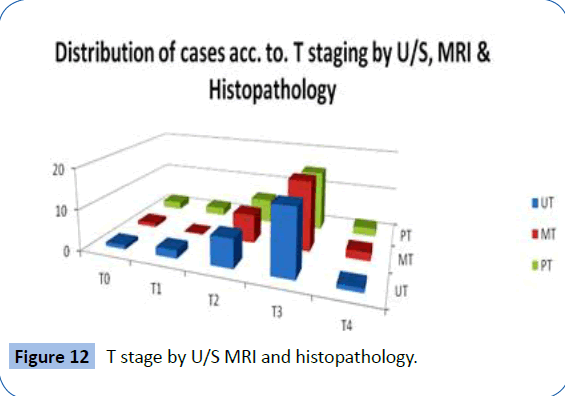
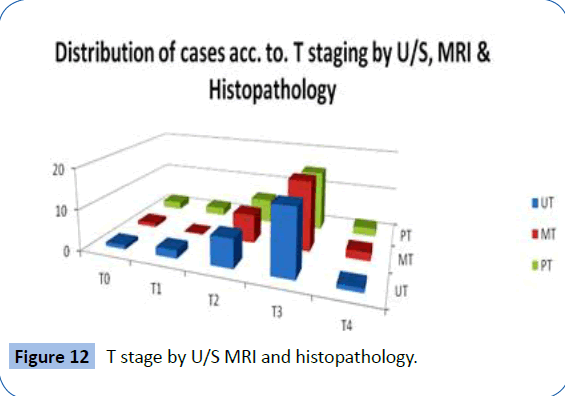
Figure 12: T stage by U/S MRI and histopathology.
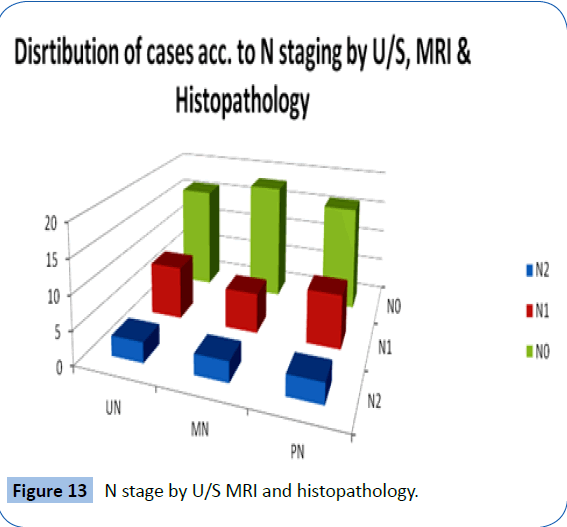
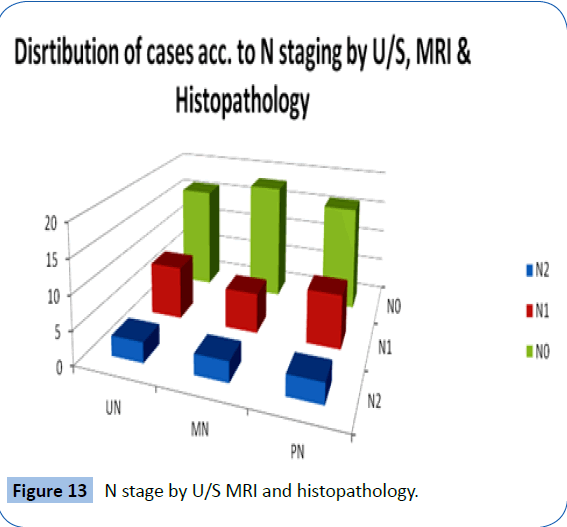
Figure 13:N stage by U/S MRI and histopathology.
Comparison between U/S and histopathology in rectal wall invasion and lymph nodes is statistically significant (p value >0.005). Comparison between MRI and histopathology in rectal wall invasion is statistically insignificant (p value = 0.999) in contrary to the lymph node status p value is >0.005. Comparison between MRI and U/S in rectal wall invasion and lymph node status is statistically significant (p value >0.001).
Discussion
Treatment of rectal cancer depends on the stage. As digital rectal examination is not accurate, preoperative imaging is mostly essential for staging [7]. The imaging modalities are CT, ERUS and MRI. CT is unreliable imaging in comparison to ERUS and MRI [8]. ERUS can delineate the anatomic layers of the rectum so it is superior in assessment of mural infiltration. However, it is operator dependent, not tolerated by the patient, and not useful in obstructing tumors or lesions of the upper rectum [9]. MRI is as useful as ERUS in assessment of T stage and is superior in assessment of nodal affection [10]. A meta-analysis carried out concluded that ERUS was the best imaging detect local invasion [11]. It was reported that ERUS is the best for rectal wall invasion while MRI for mesorectal fascia involvement and lymph nodes infiltration [12]. A study in 2012 carried out preoperative MRI has high accuracy in prediction of T stage; the agreement with histopathology was about 95% and it was as the data reported in the most of the published studies (65%-100%) [13]. Regina et al., [14] reported that MRI is the imaging of choice for primary staging of rectal cancer. Also reported ERUS is the imaging of choice to differentiate between T1 and T2 tumors if local resection is intended [14].
In our study, mesorectal fascia infiltration (CRM) by MRI is better than US as MRI is 100% accurate but US is 96.2% as US is unable to detect upper and peripheral part of mesorectum. Both MRI and US are able to detect the muscle and sphincter invasion. Ability of US in detection of rectal wall invasion was: T0 was 1 case of 2 cases about 50%, T1 was 1 case of 2 cases 50%, T2 was 5 cases of 6 cases about 83.33%, T3 was 13 cases of 15 cases about 86.6666%, T4 was 1 case of 2 cases. Ability of US in detection of lymph nodes invasion was: N0 was 15 cases of 16 cases about 93.75%, N1 was 6 cases of 8 cases. Ability of MRI in detection of rectal wall invasion was: T0 was 1 case of 2 cases about 50%, T1 was 0%, T2 was 5 cases of 6 cases about 83.33%, T3 was 14 cases of 15 cases about 93.33%. T4 was 2case of 2 cases 100%. Ability of MRI in detection of lymph nodes invasion was: N0 was 15 cases of 16 cases about 93.75%., N1 was 5 case of 8 cases about 63%, N2 was 2 cases of 3 cases about 66.66%.
Lymph node (N) staging: By MRI: proper staging was 22 cases of 27 cases about 81.5% with under staging 3 cases about 11.1% and over staging 2 cases 7.4%. By US: proper staging was 23 cases of 27 cases about 85.2% with under staging 2 case about 7.4% and over staging 2 cases 7.4%. Rectal wall invasion (T) staging: By MRI: proper staging was 22 cases of 27 cases about 81.5% with under staging 1 case about 3.7% and over staging 4 cases 14.8%. By US: proper staging was 21 cases of 27 cases about 77.8% with under staging 3 case about 11.1% and over staging 3 cases 11.1%. In conclusion, in this study comparing those two modalities we can state that phased-array MRI is slightly superior in determining the depth of transmural tumor invasion (T stage) and has same value in detecting lymph node metastases (N stage) as compared to ERUS.
Conclusion
Trans rectal U/S and MRI rectum and anal canal are complementary for proper preoperative local staging of rectal cancer.
7042
References
- Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, et al. (2005) Cancer statistics, 2005. CA Cancer J Clin 55: 10-30.
- Minsky BD1 (2001) Adjuvant radiation therapy for rectal cancer: is there finally an answer? Lancet 358: 1285-1286.
- Zampino MG,Labianca R, Beretta GD, Magni E, Gatta G, et al. (2009) Rectal cancer. Crit Rev OncolHematol 70: 160-182.
- Bellows CF, Jaffe B, Bacigalupo L, Pucciarelli S, Gagliardi G (2011) Clinical significance of magnetic resonance imaging findings in rectal cancer. World Radiol 28: 92–104.
- Halefoglu AM,Yildirim S, Avlanmis O, Sakiz D, Baykan A (2008) Endorectal ultrasonography versusphased-array magnetic resonance imaging for preoperative staging ofrectal cancer. World J Gastroenterol 14: 3504-3510.
- Wieder HA, Rosenberg R, Lordick F, Geinitz H, Beer A, et al. (2007) Rectal cancer: MR imaging before neoadjuvant chemotherapy and radiation therapy for prediction of tumor-free circumferential resection margins and long-term survival. Radiology 243: 744-751.
- Lindmark G,Gerdin B, Påhlman L, Bergström R, Glimelius B (1994) Prognostic predictors in colorectal cancer. Dis Colon Rectum 37: 1219-1227.
- Hodgman CG, MacCarty RL, Wolff BG, May GR, Berquist TH, et al. (2002) Preoperative staging of rectal carcinoma by computed tomography and 0.15T magnetic resonance imaging. Preliminary report. Dis Colon Rectum 29: 446-450.
- Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, et al. (2002) Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum 45: 10-15.
- Kwok H,Bissett IP, Hill GL (2000) Preoperative staging of rectal cancer. Int J Colorectal Dis 15: 9-20.
- Bipat S,Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, et al. (2004) Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology 232: 773-783.
- Samee A,Selvasekar CR (2011) Current trends in staging rectal cancer. World J Gastroenterol 17: 828-834.
- Giusti S, Buccianti P, Castagna M, Fruzzetti E, Fattori S, et al. (2012) Preoperative rectal cancer staging with phasedarray MR. Radiation Oncology 7:29.
- Regina GH, Tan B, Doenja MJ, Lambregts, Maas M, et.al (2013) Magnetic resonance imaging for the clinical management of rectal cancer patients. Recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. EurRadiol 23: 2522-2531.