Seyed Mokhtari SA1*, Mahmodlou R2, Ebrahimi H2 and Shabani Shojaei P1
1Student Research Committee, Urmia University of Medical Sciences, Urmia, Iran
2Department of Surgery, Imam Khomeini General Hospital, Urmia University of Medical Sciences, Urmia, Iran
Corresponding Author:
Seyed Arman Seyed Mokhtari
Student Research Committee
Urmia University of Medical Sciences
Urmia, Iran
Tel: +98-413-3852012
E-mail: armanmxt@yahoo.com
Received date: June 18, 2018; Accepted date: July 30, 2018; Published date: August 06, 2018
Citation: Seyed Mokhtari SA, Mahmodlou R, Ebrahimi H, Shabani Shojaei P (2018) Comparing Two Year Survival Rate of Esophageal Cancer Patients with and without Neoadjuvant Chemoradiotherapy Treatment. Arch Med Vol No:10 Iss No:4:5 doi: 10.21767/1989-5216.1000281
Copyright: © 2018 Seyed Mokhtari SA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords:
Esophageal cancer; Neoadjuvant therapy; Chemotherapy; Radiotherapy; Iran
Introduction
Esophageal cancer is a malignant and invasive tumor with a 5 year mortality rate of more than 90 percent. The growth rate of esophageal cancer, when compared to other types of malignancies, is significantly higher [1,2]. Esophageal cancer often arises from squamous cell hyperplasia. Monotherapy with surgery of radiotherapy do not yield hopeful results [2]. The management of advanced local esophageal cancer has evolved from monotherapy with surgery of chemotherapy to concomitant chemoradiotherapy prior to surgery (neoadjuvant chemoradiotherapy) with the aim of reducing the tumor size. Results reveal that neoadjuvant chemoradiotherapy wields better results compared to other methods [3].
In the past decades, tumor excision was considered to be the most effective method in treating non-metastatic esophageal tumors [4]. Two separate trials were performed with the aim of comparing surgical and radio therapeutic monotherapy; results reveal that surgery is more effective in cases of resect able esophageal tumors [5]. Trimodal chemoradiotherapy and surgery is considered as the most effective approach in the treatment of esophageal patients who are able to withstand the procedure. This method is the standard approach in patients with grades IB, II, III and IVA cancer [6]. Based on the various clinical trials performed, this method of treatment has been approved and confirmed by first grade clinical evidence [7]. Based on gathered evidence, 15 to 30 percent of the patients treated with neoadjuvant chemotherapy show complete pathological remission, as so the tumor itself is completely treated and no longer exists. These patients have 3 year survival rate of 50% [8].
Based on previous studies, the total survival rate and swallowing ability of patients with esophageal cancer was significantly higher in those who had undergone surgery. Also, the 3 year mortality rate was higher in patients who had had surgery when compared to subjects who had been treated with radiotherapy [9]. The main reason behind the failure of surgical methods can be pertained to the systemic attributes of esophageal cancer at the time of treatment [10,11]. Early systemic chemotherapy and also local radiotherapy, alongside surgical procedures, help limiting the spread of cancer and thus increase survival rates. The results of the many trials performed with the aim of comparing additional treatment before and after surgery, have been contradictory. In order to preserve the larynx better, Patients affected by cervical esophageal cancer are treated before or after surgery with chemoradiotherapy. Although most studies were performed on squamous cell tumors, glandular epithelium was also considered in some studies. However, since previous studies had not reached the conclusion that various tumors may react differently when treated with chemotherapy or radiotherapy, in most cases the cellular pathologic variations between these two types of tumor were not defined clearly [12].
Although surgical methods still remain the main choice of treatment in the management of esophageal cancer, the results of randomized control trials are now questioning the benefits of this method in cases of small cell carcinoma (SCC) esophageal cancer [13-15]. At hand retrospective studies both confirm and deny the superiority of surgical methods [16,17]. Studies are yet to reach a definitive conclusion concerning the positive effects of neoadjuvant chemoradiotherapy prior to surgery.
Since the treatment of esophageal cancer is highly dependent on the race and genetic predisposition of the patients and also that no previous studies were performed on esophageal cancer in the north western belt of Iran, this study was designed with the aim of determining and comparing the two year survival rate of patients who had, and had not received neoadjuvant chemoradiotherapy.
Materials and Methods
This retrospective study was approved by the ethical committee of Urmia University of medical sciences. All esophageal cancer patients who had undergone surgery at imam khomeini educational hospital, Urmia, between 2011 and 2016 were enrolled (n=280). Subjects were divided to two groups: 1) Those receiving neoadjuvant therapy (n=168) and 2) Those not receiving neoadjuvant therapy (n=112). Data related to demographic attributes were extracted from medical records. In order to determine the two year survival rate and quality of life of the subjects, phone calls were performed two years after their surgery.
Quantitative data were reported as mean ± SD, while qualitative variables were reported as percent. In order to compare the frequency of qualitative data between the two groups (treated with chemoradiotherapy/ untreated), Chi square test (and also if required, the fisher test), and in order to compare quantitative data (age), independent T-test was used. Kaplan Meier survival analysis was employed in order to determine the two year survival rate of the two groups. Data analysis was performed using SPSS software 17. P-Values less than 0.05 were assumed statistically significant.
Results
In this study, 280 esophageal cancer patients who had received chemotherapy and undergone surgery were admitted. Subjects were randomly divided into two groups. One group received neoadjuvant chemoradiotherapy prior to surgery while the other didn’t.
Gender distribution in the two groups was as follows: 1) the group who had received chemoradiotherapy, 98 (58.3%) males and 70 (41.7%) females 2) the group who had not received chemoradiotherapy; 61 (54.4%) males and 51 (45.6%) females. Comparison between the gender distribution of the subjects of either groups revealed no significant variation (P=0.36).
The mean age of the patients treated with neoadjuvant chemoradiotherapy was 70.02 ± 10.26 and that of those who had not received this treatment was 70.02 ± 11.48. Comparison of age distribution between two groups did not reveal a significant variation between (P=0.54). The most common symptom in patients was dysphagia in each group (90.4% versus 87.5%) and also the most common types of esophagus cancer in our study was SCC in each group (88% versus 91.07%). Table 1 summarizes demographic of patients, presenting symptoms and histology types of the tumors treated with and without neoadjuvant chemo-radiotherapy.
| Variables |
With neoadjuvant chemoradiotherapy |
Without neoadjuvant chemoradiotherapy |
| n=168 |
n=112 |
| Gender |
|
|
| Male |
98 (58.3%) |
61 (54.4%) |
| Female |
70 (41.7%) |
51 (45.6%) |
| Age |
70.02 ± 10.26 |
70.02 ± 11.48 |
| Presenting Symptoms |
| Dysphagia |
152 (90.4%) |
98 (87.5%) |
| Epigastric or retrosternal pain |
10 (6.06%) |
7 (6.25%) |
| Hoarseness |
4 (2.38) |
3 (3.57%) |
| Persistent cough |
2 (1.16%) |
4 (2.68%) |
| Histology types |
| SCC |
148 (88%) |
102 (91.07%) |
| Adenocarcinoma |
20 (12%) |
10 (8.93%) |
Table 1: Data presented as number, proportions (%), and mean (SD).
From 168 patients who had received neoadjuvant chemoradiotherapy, 150 (89.2%) were alive while 18 (10.8%) had passed away. From 112 patients who were not treated by neoadjuvant chemoradiotherapy, 79 (70.5%) were alive and 33 (29.5%) were deceased. A significant variation concerning survival rates between the two groups were observed (P=0.031). The average survival rate of the first group (treated with neoadjuvant chemoradiotherapy) was 27.20 ± 5.21, and of the second group (untreated) was 7.12 ± 5.86. A significant variation is observed between the survival rates of the two groups (p=0.001). Of the 33 untreated patients who had passed away, 15 (45.4%) were men and 18 (54.6%) were women. Of the deceased patients treated with neoadjuvant chemoradiotherapy (n=18), 13 (72.22%) were men and 5 (27.78%) were women. No significant variation in gender distribution was observed (p=0.68). The average age of the 13 deceased patients who had not received neoadjuvant radiotherapy was 66.86 ± 12.01, and that of those who had received this treatment was 76.56 ± 10.31. Based on the performed T-test results, no significant variation was present between the groups regarding age distribution of the deceased (P=0.12).
After one year of treatment, 164 (97.61%) subjects of the first group were still alive. Of the second group (who had not been treated with neoadjuvant chemoradiotherapy), 88 subjects (78.57%) were still alive. In the second year post operation, in the first group 162 subjects (98.78%) and of the second group 81 subjects (92.04%) where still alive. Post operation follow up the subjects revealed that the two year survival rate of the group which were treated with neoadjuvant chemoradiotherapy was 98.78% (n=162) with 1.22% (n=2) mortality. Of the 88 viable patients two years post operation, 81 patients (92.04%) were alive while 7 (7.96%) had passed away. A significant variation was observed between the two groups concerning two year survival rates (P=0.01).
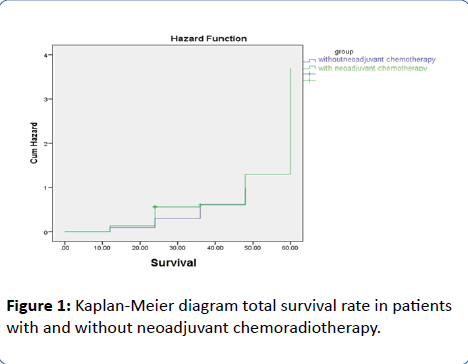
According to the Kaplan Meier survival analysis, the average survival rate of the first group (received neoadjuvant chemoradiotherapy) was 42.96 ± 2.74 months and that of the second group (untreated) was 41 ± 3.12 months. With a Pvalue= 0.03, it is revealed that a significant variation is present between the two year survival rates of the two study groups. As it is evident from the graph provided, this value is significantly higher in the group which had received neoadjuvant treatment (Figure 1).
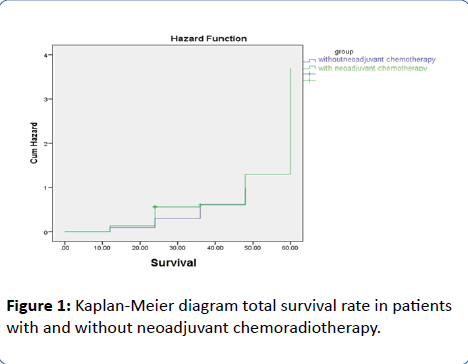
Figure 1: Kaplan-Meier diagram total survival rate in patients with and without neoadjuvant chemoradiotherapy.
Discussion
In this study, which is performed on 280 patients suffering from esophageal cancer, 168 subjects received neoadjuvant chemoradiotherapy while the remaining 112 were spared. The aim of this study was to compare the two year survival rate of esophageal cancer patients residing in the north western belt of Iran, based on receiving neoadjuvant chemoradiotherapy treatment or otherwise. Gender distribution of the first group (treated) was 98 (58.3%) men and 70 (41.7%) women. Gender distribution of the second group (untreated) was 61 (54.4%) men and 51 (45.6%) women. The mean age of the first group was 70.02 ± 10.26 and that of the second group was 70.02 ± 11.48 years. In this study, no significant variation was observed between the groups on ground of age and gender distribution. Thus, neither were considered as confounding factors.
In this study, 150 (89.2%) of the treated subjects were alive while 18 subjects (10.8%) had passed away. However, 70.5% (n=79) of the untreated subjects were alive and a significant 29.5% (n=33) were deceased (p=0.031). The average survival rate of the deceased subjects in the first group was 27.20 ± 5.21 months while the second group’s was 7.12 ± 5.86 (p=0.001). The finds of this study reveal that of 33 deceased patients of the second group, 15 (45.4%) were men and 18 (54.6%) were women. Of the 18 deceased subjects of the first group, 13 (72.22%) were men and 5 (27.78%) were women. No significant variation was observed between age distribution of the deceased of either groups (p=0.68).
In this study, the first year post op survival rate of the treated subjects was 97.61 % (n=164). Of the untreated subjects, 88 (78.571%) were alive after the first year checkpoint. In a study performed by Stahl et al. it revealed that 3 year survival rate of pre-op radiotherapy increased from 27.7% to 47.4%. In addition, it was also determined that pre-op chemoradiotherapy is superior to pre-op chemotherapy considering survival rates in in patients with locally advanced adenocarcinoma of the esophagogastric junction. The finds of the mentioned study were consistent with that of the current research, since the one year survival rate was 54.3% [18].
Second year post operational survival rates of treated patients was 98.78% (n=162) and 92.04% (n=81) in untreated patients. The mean survival rate of the treated patients was 42.96 ± 2.74 months and that of the untreated patients was 41 ± 3.12 months. With a p value of 0.03, a significant variation is observable between the survival rates of the two groups. As it is also shown in the survival graph provided, it is evident that patients treated with neoadjuvant chemoradiotherapy have a higher survival rate compared to the opposing group.
The finds of this study, concerning the two year survival rate of the patients, are consistent with that of the study performed by Malthane et al. with the aim of “determining the effect of pre-operational chemotherapy in patients with surgically treatable thoracic esophageal cancer patients”. When comparing the ratios of one year and two year survival rates of concomitant chemotherapy and surgery against surgery alone, no significant variation was observed. However, when comparing third year survival rates, a 21% rise was observed in the survival rates of patients undergone pre-op chemoradiotherapy, in the fourth year. However these finds were not statistically significant. Only when 5th year survival rates were compared, significant variations were observed. In general, it was concluded that pre-operational chemotherapy is beneficent for the 3rd, 4th and also 5th year survival rates, which was similar to the finds of the current study. In addition, the importance of pre-operational chemoradiotherapy was also highlighted, so that higher survival rates should be expected in patients who receive this treatment [19].
In a study performed by Ancona et al. it was concluded that patients with resectable esophageal cancer who had received pre-operational chemoradiotherapy, had achieved complete remission and also higher long term survival rates in contrast to opposing groups [20]. In a study carried out by Walsh et al. it was determined that pre-operative chemotherapy and subsequent resection had lesser esophageal tissue resection but higher complete resection (RO), when compared to surgical-only treatments [21]. In general, this multi-aspect study was unable to determine the benefits of pre-operational chemotherapy followed by surgery. However, the finds of this study were consistent with that of ours.
Conclusion
Considering the gathered results, our study reveals that preoperational neoadjuvant chemoradiotherapy is beneficial for the survival rates of patients suffering from esophageal cancer, therefore we recommend that prior to performing invasive treatments, such as surgery, it is beneficial to provide chemoradiotherapy for these patients. Amongst the limitations of this study, the small study population is probably the most notable difference than other similar studies. This retrospective study was performed over a short period of time, thus variables such as tumor size and staging could not be accounted for. Therefore in order to determine patients better who have higher response rate to neoadjuvant chemoradiotherapy, further studies are required to be performed. Due to the aforementioned reasons, further more extensive studies are called for in order to determine the survival rate of esophageal cancer patients better.
23058
References
- Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63: 11-30.
- Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, et al. (2011) Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: An updated meta-analysis. Lancet Oncol 12: 681-692.
- van Hagen P, Hulshof M, Van Lanschot J, Steyerberg E, Henegouwen MvB, et al. (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366: 2074-2084.
- Müller J, Erasmi H, Stelzner M, Zieren U, Pichlmaier H (1990) Surgical therapy of oesophageal carcinoma. Br J Surg 77: 845-857.
- Badwe RA, Sharma V, Bhansali MS, Dinshaw KA, Patil PK, et al. (1999) The quality of swallowing for patients with operable esophageal carcinoma. Cancer 85: 763-768.
- Tepper J, Krasna MJ, Niedzwiecki D, Hollis D, Reed CE, et al. (2008) Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26: 1086-1092.
- Blum Murphy M, Xiao L, Patel VR, Maru DM, Correa AM, et al. (2017) Pathological complete response in patients with esophageal cancer after the trimodality approach: The association with baseline variables and survival-The University of Texas MD Anderson Cancer Center experience. Cancer 123: 4106-4113.
- Hategan M, Cook N, Prewett S, Hindmarsh A, Qian W, et al. (2015) Trimodality therapy and definitive chemoradiotherapy for esophageal cancer: a single-center experience and review of the literature. Dis Esophagus 28: 612-618.
- Best LM, Mughal M, Gurusamy KS (2016) Non?surgical versus surgical treatment for oesophageal cancer. Cochrane Database Syst Rev 3: CD011498.
- Viaro AL, Roballo CA, de Campos PTR, Teixeira CO, Teixeira MAB (2015) Occult esophageal squamous cell carcinoma with metastases to the spine and central nervous system. Autops Case Rep 5: 33.
- Kim G, Suntharalingam M (2017) Carcinoma of the esophagus. Clinical Radiation Oncology: Indications, Techniques and Results.
- Aikou T (2016) Three-field lymphadenectomy for esophageal cancer. Atlas of Upper Gastrointestinal and Hepato-Pancreato-Biliary Surgery- Springer: 107-111.
- Bedenne L, Michel P, Bouché O, Milan C, Mariette C, et al. (2007) Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 25: 1160-1168.
- Chiu PW, Chan AC, Leung S, Leong H, Kwong K, et al. (2005) Multicenter prospective randomized trial comparing standard esophagectomy with chemoradiotherapy for treatment of squamous esophageal cancer: early results from the chinese university research group for esophageal cancer (CURE). J Gastrointest Surg 9: 794.
- Stahl M, Stuschke M, Lehmann N, Meyer HJ, Walz MK, et al. (2005) Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23: 2310-2317.
- McKenzie S, Mailey B, Artinyan A, Metchikian M, Shibata S, et al. (2011) Improved outcomes in the management of esophageal cancer with the addition of surgical resection to chemoradiation therapy. Ann Surg Oncol 18: 551-558.
- Monjazeb AM, Riedlinger G, Aklilu M, Geisinger KR, Mishra G, et al. (2010) Outcomes of patients with esophageal cancer staged with [18F] fluorodeoxyglucose positron emission tomography (FDG-PET): Can postchemoradiotherapy FDG-PET predict the utility of resection? J Clin Oncol 28: 4714-4721.
- Stahl M, Walz MK, Stuschke M, Lehmann N, Meyer HJ, et al. (2009) Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol 27: 851-856.
- Malthaner R, Fenlon D (2003) Preoperative chemotherapy for resectable thoracic esophageal cancer. Cochrane Database Syst Rev 4: CD001556.
- Ancona E, Ruol A, Santi S, Merigliano S, Chiarion Sileni V, et al. (2001) Only pathologic complete response to neoadjuvant chemotherapy improves significantly the long term survival of patients with resectable esophageal squamous cell carcinoma. Cancer 91: 2165-2174.
- Walsh T, Grennell M, Mansoor S, Kelly A (2002) Neoadjuvant treatment of advanced stage esophageal adenocarcinoma increases survival. Dis Esophag 15: 121-124.