Stefan Mausbach1*, Alexandra Gerasimova1, Ze’ev Itsekson1, Noit Brown1, Yvonne Schwammenthal1,2, Oleg Merzlyak1, Mati Bakon3 and David Orion1,2
1Department of Neurology, Sheba Medical Center, Tel HaShomer, Israel
2Sackler Faculty of Medicine, Tel Aviv, Israel
3Department of Neuroradiology, Sheba Medical Center, Tel HaShomer, Israel
*Corresponding Author:
Dr. Stefan Mausbach
Department of Neurology
Sheba Medical Center
Tel HaShomer, Israel
Tel: 491715234190
E-mail: S.Mausbach@gmail.com
Received Date: February 13, 2019; Accepted Date: March 18, 2019; Published Date: March 24, 2019
Citation: Mausbach S, Gerasimova A, Itsekson Z, Brown N, Schwammenthal Y, et al. (2019) Comparison of Direct Endovascular Treatment Versus Thrombolysis and Rescue-endovascular Treatment for Patients with M1/M2 Occlusion: A Real-life Retrospective Study. J Neurol Neurosci Vol.10 No.02:295. DOI: 10.36648/2171-6625.10.2.295
Keywords
Stroke; Endovascular treatment; Stent retriever; Thrombolysis
Introduction
Ischemic stroke is a disease with rising prevalence. Two-thirds of patients suffer from a cardiovascular incidence from the age of 65 onwards [1]. On the background of aging, specifically in the western world, there is increasing need for effective treatment for ischemic stroke.
Today, there are two main therapeutic approaches. One is thrombolysis by intravenous administration of recombinant tissue Plasminogen Activator (tPA) as systemic therapy, the other is by an endovascular approach. While systemic treatment is limited to a restricted time window, endovascular therapy offers a more extensive window as well as better treatment options for large vessel occlusions where systemic therapy may be limited.
In certain instances, it appears that thrombolytic therapy has limited success. Studies published in 2011 [2] and 2014 [3] showed that thrombolytic therapy has no benefit in large vessels with a clot larger than 8 mm.
Since the approval of the Solitaire FR catheter, stent retriever has become the worldwide standard for endo-vascular treatment. Other catheters, such as Trevo, show similar recanalization rates [4].
In light of these studies, it is important to mention, that endovascular therapy for intracranial artery occlusion is still a second line treatment, according to the latest guidelines of the American Heart Association [5]. The first treatment line for ischemic stroke is still intravenous thrombolysis. Endovascular therapy is an established rescue treatment in those cases where thrombolytic therapy fails or if contraindications to systemic thrombolysis exist.
The aim of this study was to analyze, if there would be a better outcome for direct endovascular treatment in comparison to prior treatment by systemic thrombolysis with no, or insufficient improvement and secondary rescue endovascular treatment in a real-life cohort.
Patients and Methods
The study protocol was approved by the Committee on Human Research at the Sheba Medical Center. In this retrospective cohort mono-center study, patients were identified from the Database of the Department of Neurology at the Sheba Medical Center. Eligible Patients from January 2014 until December 2017 were included.
Inclusion criteria
Patients aged 18-90 years that were diagnosed with an ischemic stroke and occlusion of the middle cerebral artery territory by imaging between January 2014 and December 2017 and received endovascular treatment at Sheba Medical Center, according to the Stroke and Endovascular Unit of Neurology. Included were only patients with a prior mRS of 0-1.
Exclusion criteria
Patients not fulfilling the age criteria, improvement after systemic thrombolysis, no indication for mechanical thrombectomy, mRS ≥ 2, pregnancy, side effects after systemic thrombolysis (bleeding, allergic reaction), basilar occlusion.
Study
Patients eligible for the study were analysed for medical history and current treatment including blood thinners like platelet antiaggregant, Vitamin-K-Antagonists, NOAC and Heparin. The initial NIHSS and prior mRS were acquired. The treatment was followed by thrombolysis and endovascular treatment in comparison to direct endovascular treatment. Data from CTPerfusion scans was collected and analysed. mRS ≤ 2 was defined as favorable outcome in comparison to mRS ≥ 4 seen as nonfavorable outcome. Consent from all patients to process their data was received.
Questionnaire
NIHSS and mRS after 7 days were acquired as well as after 10-14 weeks including the EQ5D questionnaire by examination in the ward, follow-up in the outward patient department or telephonic questionnaire.
Statistical analysis
All data collected in this study was analysed using SPSS version 21.0. Deceased patients during the study were followed up over the national register with day of death. Data was observed using arithmetic mean, medians and standard deviations. The interquartile range was used as a measure of distribution. A comparison between the two groups was performed using cross-tables for independent samples and continuous variables.
Results
55 patients receiving tPA and EVT and 52 patients receiving direct EVT were included in the study (Table 1). A total of 5 where lost for follow up (2 not interested, 3 left the country).
| Baseline characteristics of the study population |
| Characteristics |
tPA + EVT (N=52) |
EVT (N=55) |
| Age |
Median |
71 |
73.5 |
| Interquartile range |
34-88 |
28-90 |
| Male sex |
no. (%) |
27 (51.9) |
25 (45.5) |
| Cardiovascular Risk factors |
| Art. Hypertension no. (%) |
37 (71.15) |
35 (63.36) |
| Dyslipidemia no. (%) |
30 (57.69) |
28 (50.91) |
| DM no. (%) |
9 (17.31) |
14 (25.45) |
| |
AF/PAF no. (%) |
24 (46.15) |
32 (58.18) |
| |
CHF no. (%) |
10 (19.23) |
16 (29.09) |
| |
Stroke in the Past no. (%) |
8 (15.38) |
10 (18.18) |
| |
Median HBA1c (%) |
5.8 |
5.3 |
| Baseline NIHSS |
| median |
16.5 |
15 |
| Dense Artery sign native CT |
median in mm (no of patients) |
162 mm (37) |
218 mm (43) |
| Extracranial occlusion |
no (%) |
8 (15.3) |
9 (16.4) |
| Time intubated |
| median in days |
1.55 |
1.4 |
Table 1: Analysis of study groups regarding age, cardiovascular risk factors, stroke in the past, initial NIHSS and rate of extracranial occlusion in addition to proximal MCA-occlusion.
The initial outcome of each procedure was determined by modified Ranking Scale that was evaluated after 7 days (or dismissal) as well as after 10-14 weeks. mRS ≤ 2 is seen as favorable outcome as this still holds the potential of regaining ability to carry out all previous activities. mRS ≥ 4 is seen as non-favorable outcome as it renders the patient with need for help with own bodily needs and assisted walking, is bed bound or deceased.
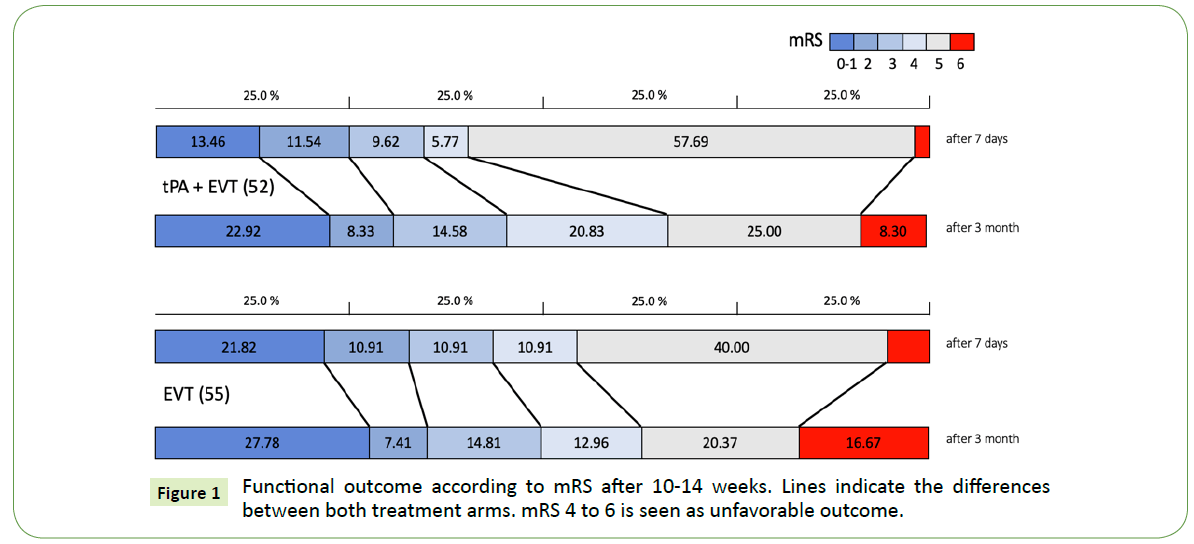
There is a first difference after 7 days regarding the two treatment groups (Figure 1). After tPA + EVT, 25% of all patients reached a favorable outcome while nearly 33% with direct EVT reached this outcome. Nearly 66% of patients receiving both treatments show an unfavorable outcome in contrast to 56% in the EVT group. Important to notice is the higher number of patients with mRS 6 in this group in the first follow up after 7 days.
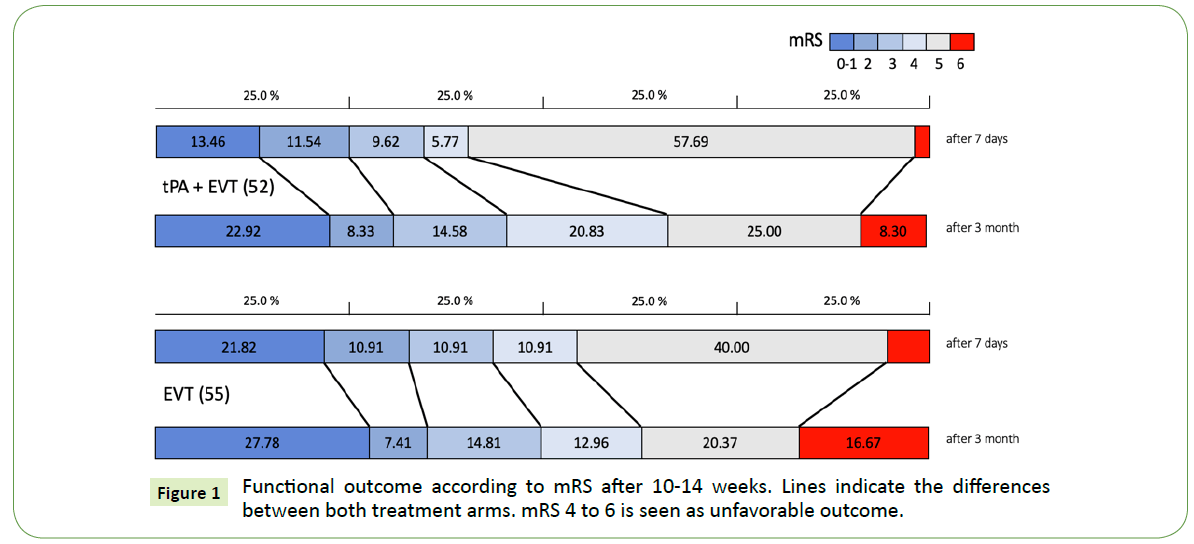
Figure 1: Functional outcome according to mRS after 10-14 weeks. Lines indicate the differences between both treatment arms. mRS 4 to 6 is seen as unfavorable outcome.
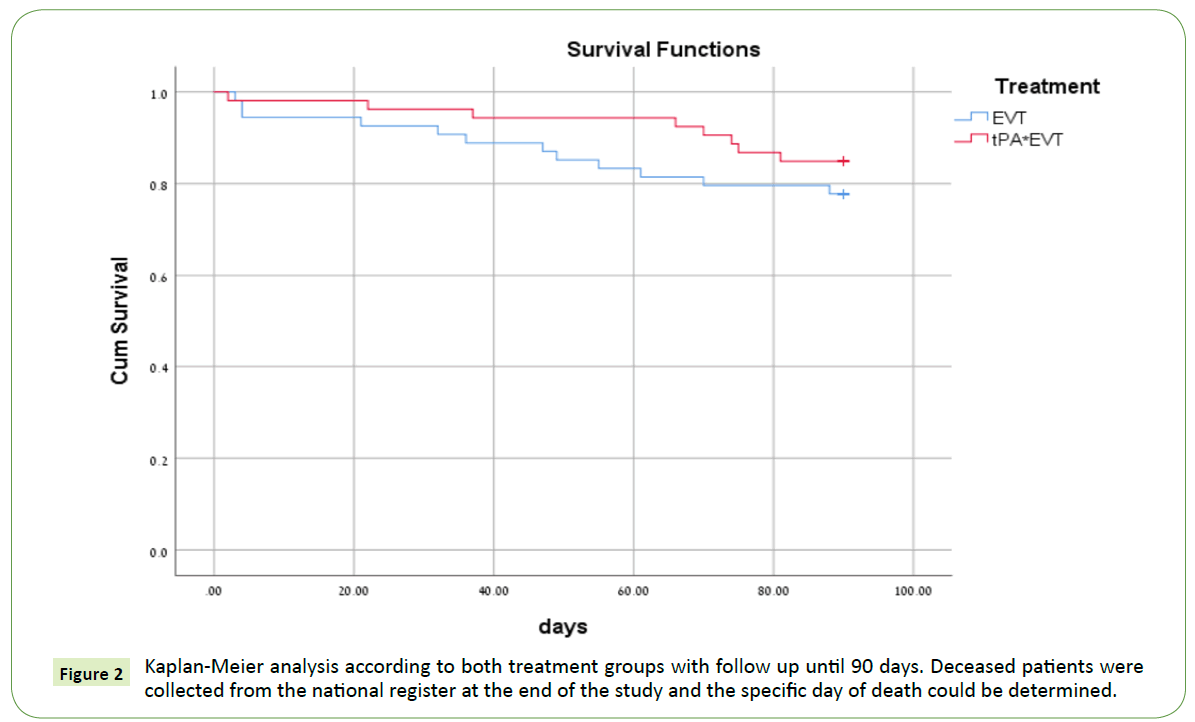
After 3 months, an increase in mortality in both groups can be seen with a higher rate in the EVT group (Figure 2). Specifically, tPA+EVT shows improvement after 3 months in the groups of mRS 4 and 5 with progress under time and physiotherapy to a better functional outcome and an increase in total of 6% of favorable outcome. The EVT group shows an increased mortality and only a slight increase in the percentage of favorable outcome (3%). It should be pointed out that after 3 months, the best possible outcome with mRS 0-1 is highest in the EVT group. Regarding the favorable outcome set to mRS ≤ 2, there is no statistical difference between both study arms. The EVT group reaches 35% in comparison to 31% in the other group.
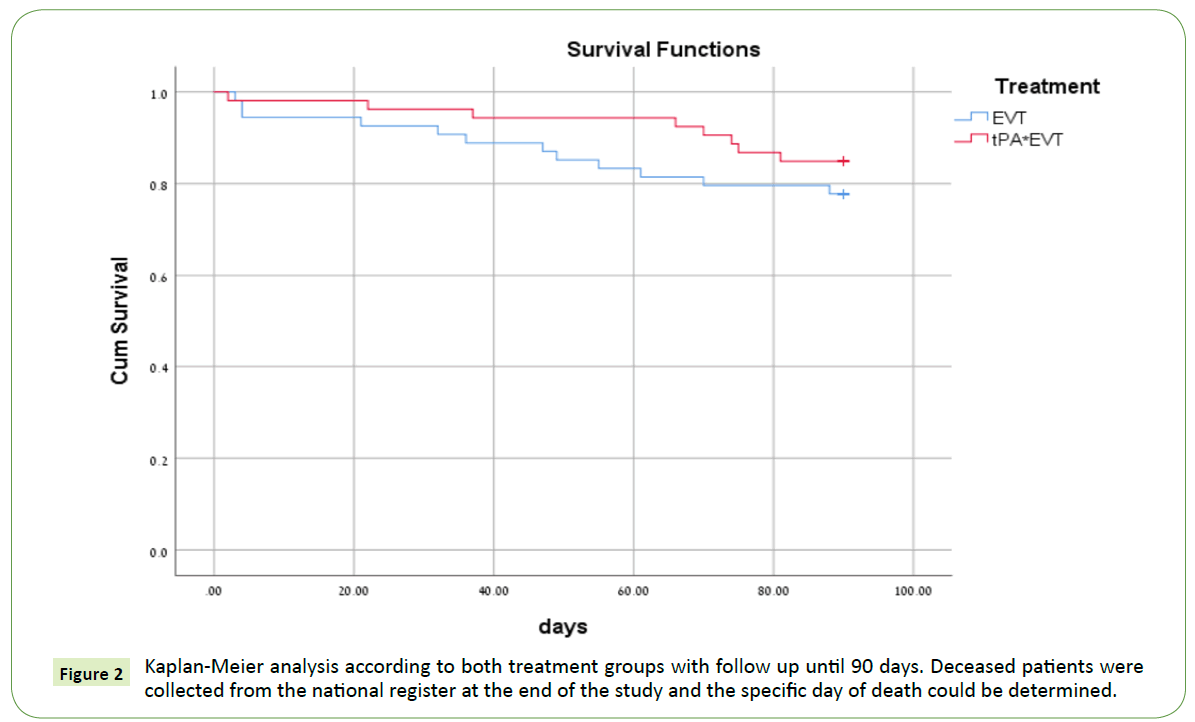
Figure 2: Kaplan-Meier analysis according to both treatment groups with follow up until 90 days. Deceased patients were collected from the national register at the end of the study and the specific day of death could be determined.
The Kaplan-Meier analysis (Figure 2) shows an initial higher rate of death in the first week after treatment in the direct endovascular group. A second decline starts 45 days after EVT treatment and 65 days after prior tPA treatment (Figure 2). In total 20 patients passed away during the study time of 98 days, 3 passed away during the first 7 days after direct EVT, 1 patient after prior tPA treatment.
10 to 14 weeks after the stroke event, patients underwent 2 telephone consultation to the standard EQ5D scale, an instrument of evaluating quality of life and general health status. Patients were questioned regarding their mobility, self-care, general care, pain and depression/anxiety level. The answer options ranged from no influence on life (1), medium influence on life (2) and strong influence on life (3). In the individual analyzes of the different mRS groups, it points out that the EVT group with mRS 0-1 has the best ratings (Table 2). From mRS 2 on there is a decline while the subjective ratings stay stable in the tPA+EVT group and only start to decline from mRS3.
| EQ5D Questionnaire after 10-14 weeks |
| mRS |
0-1 |
2 |
3 |
4 |
5 |
| Treatment arm |
tPA + EVT |
EVT |
tPA + EVT |
EVT |
tPA + EVT |
EVT |
tPA + EVT |
EVT |
tPA + EVT |
EVT |
| No. Patients |
14 |
11 |
5 |
3 |
6 |
7 |
9 |
7 |
8 |
9 |
| Mobility |
Mean-No. |
1.36 |
1.21 |
1.20 |
2.33 |
1.67 |
2.00 |
2.22 |
2.57 |
3.00 |
2.56 |
| Self-Care |
Mean-No. |
1.09 |
1.14 |
1.20 |
2.33 |
1.50 |
2.86 |
2.56 |
3.00 |
3.00 |
3.00 |
| General Ability |
Mean-No. |
1.36 |
1.21 |
1.60 |
2.33 |
1.67 |
2.86 |
2.33 |
2.71 |
3.00 |
2.56 |
| Pain |
Mean-No. |
1.82 |
1.29 |
1.60 |
1.66 |
1.33 |
1.86 |
1.89 |
2.76 |
1.50 |
1.78 |
| Depression/ Anxiety |
Mean-No. |
1.72 |
1.36 |
1.40 |
2.00 |
1.50 |
1.86 |
2.00 |
1.78 |
2.00 |
1.80 |
Table 2: Analysis after 10-14 weeks for both treatment groups regarding EQ5D (measurement for general health introduced by European Quality Group in 1990 with a questionnaire of 5 questions). Results are shown in mean value.
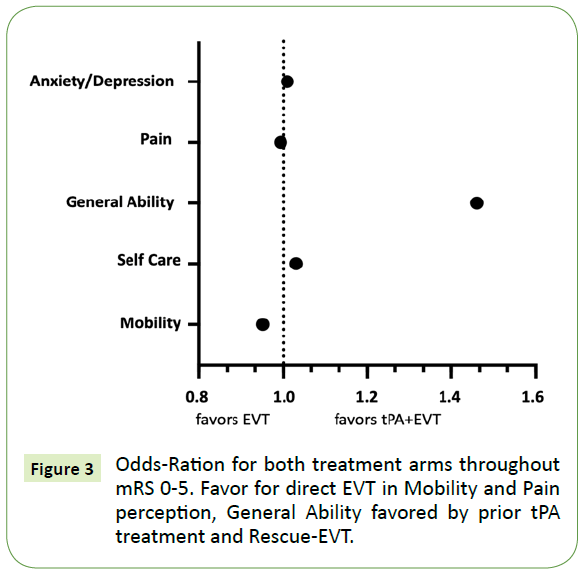
Regarding the odds-ratio including all patient outcomes, there is a favor for EVT for mobility and slightly for pain susceptibility, Anxiety and Depression as well as self-care is slightly favored for prior thrombolysis. Outstanding is the result for general ability which clearly favors tPA with additional endovascular treatment (Figure 3).
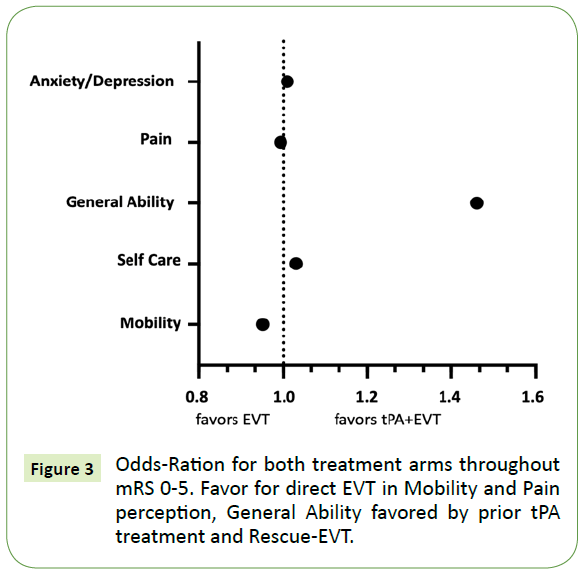
Figure 3: Odds-Ration for both treatment arms throughout mRS 0-5. Favor for direct EVT in Mobility and Pain perception, General Ability favored by prior tPA treatment and Rescue-EVT.
For further investigation of predefined outcome regarding imaging, patient data were further analyzed for size of penumbra and core infarction (Table 3). Via volume rendering, both could be exactly measured. There is no correlation of penumbra size to outcome. There is slight trend of core infarct size and outcome, yet the position of the core infarction is more predefining then the size.
| CT Perfusion results |
| mRS |
0 |
1 |
2 |
3 |
4 |
5 |
6 |
| Penumbra |
12.92 |
10.92 |
14.21 |
15.06 |
13.72 |
14.95 |
13.81 |
| Core Infarct |
1.08 |
1.39 |
2.26 |
2.49 |
2.64 |
2.06 |
2.44 |
Table 3: Correlation of Penumbra to Core Infarct on CT-Perfusion scans before mechanical thrombectomy. Not statistical relevance can be seen regarding the penumbra and the outcome. There is a slight correlation between size of the core infarction and a higher mRS.
Discussion
The treatment by tPA is still the most established treatment for eligible patients. The studies with intra-arterial thrombolysis [6] and early mechanical thrombectomy devices like Merci [7] showed no benefit over tPA. The studies from 2014 and 2015 regarding Stent-Retriever, showed improved outcomes in case of revascularization rate and outcome for large vessel occlusions. The current guidelines by AHA/ASA recommend tPA for patients eligible for the first 4.5 hours after symptom onset. Even if endovascular treatment is considered, tPA is recommended to be given.
Patients received therapy by thrombolysis during the first 4.5 hours after symptom onset if eligible. After lack of improvement, or only minor improvement during the first 45 minutes of thrombolysis treatment, a CTA of head and neck and a CTP were performed. With fitting criteria regarding penumbra and core infarct, patients underwent mechanical thrombectomy during the first 6 h after symptom onset.
Patients not eligible for thrombolysis treatment following the guidelines by ASA/AHA underwent direct thrombectomy during the first 6 hours of symptoms. The initial analysis regarding mRS show a better outcome after direct EVT treatment. Nearly 33% regain the ability to return to normal life including return to work after dismissal from hospital. In comparison, 25% got the same outcome after prior tPA treatment.
Two-thirds of the tPA+EVT group show an unfavorable outcome which is defined by mRS ≥ 4 with a very high number of mRS 5 with nearly 58%. After direct EVT treatment, 56% showed an unfavorable outcome with 40% of mRS 5, showing in conclusion that more people are rendered with significant loss of life quality after prior thrombolysis.
After 10-14 weeks, there is improvement in both groups. Specifically, in the tPA+EVT group, with improvement specifically for the more severely disabled patients. There is a high shift from mRS 5 to better outcomes and only a slight increase of deceased patients. All in all, 31% reach a favorable outcome. Direct EVT treatment as well shows a shift to better outcome. 35% show a mRS ≤ 2 in the follow up. But the shift from mRS 5 points to both directions. The total amount is reduced to 20% with equal improvement and worsening. 16,8% deceased in comparison to 8% after prior tPA treatment.
The comparison by mRS shows an initial better outcome of direct EVT treatment which favors this method of stroke intervention. 34% return to a good to very good outcome, there are less patients with unfavorable outcome and there is further improvement in the following 10-14 weeks. Important to notice is the higher rate of death. One reason is unsuccessful revascularization, but also higher rates of intracranial bleedings and massive intracerebral bleedings either due to mechanical injury by catheter or effects by prior anticoagulation or need for loading doses for stent implantations worsen the outcome. Patients underwent endovascular treatment also with elevated INR by Vitamin K Antagonists or liver disease or treatment by new oral anticoagulations. These agents are still active during the treatment and state a higher bleeding risk. Patients receiving tPA have by definition no bleeding diathesis due to contraindications for treatment. After failure of improvement by tPA, the patient underwent the procedure including CTA and CTP for further diagnostics. On average, the patient underwent 1h after tPA the additional endovascular treatment. tPA has a clearance of 550- 680ml/minute from plasma. This results in a half-life ≤ 5 minutes and a terminal elimination after around 40 minutes. Only a reduced bleeding risk by lowering of fibrinogen endures.
The tPA studies [3] showed an initial improvement of 15% with further improvement over the next 3 months to a total average of 30%. The same can be seen in this study after 10 to 14 weeks. tPA treatment in addition to endovascular treatment shows improvement by 6% of favorable outcome and lowering by 11% of unfavorable outcome.
In comparison to the ESCAPE study [8], there is a slightly different outcome in this study. In ESCAPE, 29% showed a favorable outcome after 90 days with tPA treatment in comparison to 54% that received additional endovascular treatment. The mean NIHSS is very similar in both groups with 16.5 in the ESCAPE study and 15.7 in this study. A major difference is the randomization of patients. Patients in ESCAPE ranged from age 60 to 81, in this study from 28 to 89 with respect to higher numbers of patients above 80 years of age (25%). MR. CLEAN [9] included patients from the age of 54 to 76. The intervention group shows a beneficial outcome for 33% of patients in the follow-up after 90 days, equal to the outcome in this study with respect to lower average patient age. SWIFT PRIME [10] included 196 patients for both groups with an average age of 65.6. In this study, the average age is 69.5 years and by that close to the average age of ESCAPE with 70.5 years (excluding younger than 60 and older than 81) and by average 5 years higher than MR. CLEAN and SWIFT PRIME. The outcome regarding mRS in SWIFT PRIME shows for thrombolytic treatment a favorable outcome of 36% after 90 day, which is a better outcome than in this study after tPA treatment. These numbers are higher than in the tPA studies [3]. 60% reach a favorable outcome after additional endovascular treatment. This is nearly 25% more than in this study. The outcome in this study is equal to the results from the Netherlands by MR. CLEAN. In a more optimal cohort like SWIFT PRIME the results differ dramatically for tPA as well as tPA+EVT. The real-life data in this study includes a wider range of patients with more elderly patients and younger patients with lesser collateral blood supply. After analyzing patients regarding the objective mRS score, there was an additional questionnaire for all patients after 10-14 weeks. Out of 107 patients, 102 were available for follow up. Patients receiving direct treatment by EVT with revascularization and only minor or no stroke on the follow up CT showed the best outcome in all categories. Patients with the same favorable outcome (mRS 0-2) after prior tPA treatment show a similar result but have slightly higher rates for pain and depression/anxiety. Nearly all patients receiving both treatments were above the age of 60, while in the EVT group, a third of the patients were aged 30-50. This reflects the different judgement in the EQ5D. Specifically the score for “general ability” was in favor for thrombolysis prior to endovascular treatment. The reason might be found in the different aging of the group where a pensioner might see his abilities in context to his age, while the on average younger patients in the direct EVT group often still need to work and are rendered unable to provide for their families following the stroke. Another aspect is the higher rate of anxiety and depression in this age group which might cause a worse estimation of the subjective status. This could lead to lower motivation for physiotherapy and progress after the stroke event. Anxiety is a common problem in stroke patients, also after effective treatment. Up to 30% are affected [11]. This study did not put contrast on the treatment for anxiety and depression. Light needs to be put on in further studies.
Conclusion
Regarding this study, there are currently no recommendations to switch treatment for patients with proximal MCA occlusion. Patients can improve directly under thrombolysis therapy and by failure still undergo rescue endovascular treatment with a similar outcome to direct EVT after 10-14 weeks. Regarding analysis for quality of life, direct EVT is favorable. Patients eligible for thrombolysis should receive tPA. After insufficient improvement, there is nearly equal benefit with rescue endovascular treatment. This real-life study supports the latest guidelines by the AHA regarding the best medical treatment outcome.
Funding
The authors received no financial compensation for the study. There was no sponsoring involved.
24253
References
- Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, et al. (2011) Guidelines for the primary prevention of stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 42: 517-584.
- Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, et al. (2011) The importance of size: Successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 42: 1775-1777.
- Sit SP, Bose A, Hirsch JA, Lev MH, Grb FS (2014) Stroke: Implications for IA Therapy. Stroke 44: 3553-3556.
- Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, et al. (2012) Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): A randomised trial. The Lancet 380: 1231-1240.
- Powers WJ, Rabinstein A, Ackerson T, Adeoye OM, Tirschwell DL (2018) 2018 Guidelines for the early management of patients with acute ischemic stroke. Stroke 49: e46-e99.
- Women P, Cancer EB (2006) A randomized trial of intraarterial treatment for acute ischemic stroke. OA Library 2747-2757.
- Katz JM, Gobin YP (2006) Merci retriever in acute stroke treatment. Expert Review of Medical Devices 3: 273-280.
- Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, et al. (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. New England Journal of Medicine 1019-1030.
- Berkhemer OA, Fransen PSS, Beumer D, Van den Berg LA, Lingsma HF, et al. (2014) A randomized trial of intraarterial treatment for acute ischemic stroke. New England Journal of Medicine 372.
- Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, et al. (2012) Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): A randomized, parallel-group, non-inferiority trial. The Lancet 380: 1241-1249.
- Sun Y, Liang Y, Jiao Y, Lin J, Qu H, et al. (2017) Comparative efficacy and acceptability of antidepressant treatment in post-stroke depression: A multiple-treatments meta-analysis. BMJ Open 7: e016499.