Dalvir Gill1*, Kamalpreet Mann2, Sharanpreet Kaur1, Vanessa Goyes Ruiz1, Ryan Dean1 and Samana Zaidi1
1Department of Internal Medicine, SUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY, USA
2The University of Medicine and Health Sciences, Basseterre, St. Kitts
Corresponding Author:
Dalvir Gill
Department of Internal Medicine
SUNY Upstate Medical University
750 East Adams Street, Syracuse
NY, USA
Tel: 3158028394
E-mail: gillda@upstate.edu
Received date: January 23, 2017; Accepted date: February 23, 2017; Published date: February 28, 2017
Citation: Gill D, Mann K, Kaur S, Ruiz VG, Dean R, et al. Sjogren’s Syndrome in a Patient with Maculopapular Cutaneous Mastocytosis. Arch Med.2017, 9:1
Copyright: © 2017 Gill D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Staphylococcus aureus; Vancomycin; Linezolid
Case Report
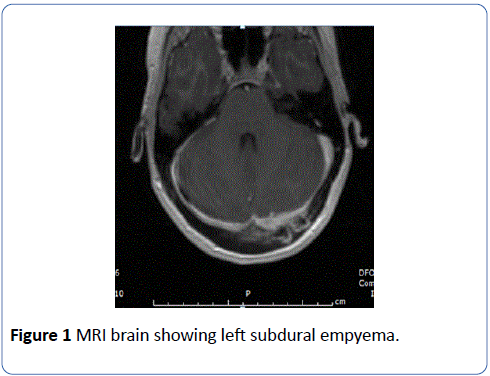
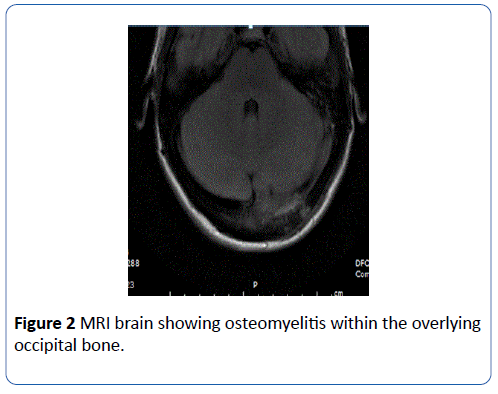
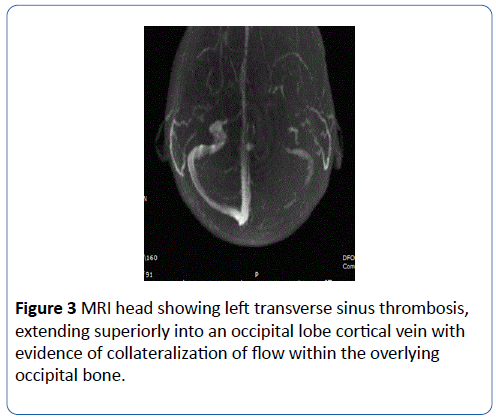
A 27-year-old female with past medical history significant for IVDU presented to emergency department with neck pain, and occipital headache for 1 week. She admitted to recent heroin use. Her vitals were significant for, blood pressure of 102/67 mm Hg, pulse of 116 beats per minute, temperature 36.9°C (oral), respiratory rate of 19 breaths per minute, oxygen saturation of 96% on room air. Physical exam was remarkable for left shoulder hematoma and track marks bilaterally on arms. WBC count was with normal range. Blood cultures grew MRSA, susceptible to vancomycin. Transesophageal echocardiogram showed 6.9 mm tricuspid valve vegetation. MRI brain showed left subdural empyema (Figure 1) and associated osteomyelitis within the overlying occipital bone (Figure 2). MRI head showed left transverse sinus thrombosis extending superiorly into an occipital lobe cortical vein with evidence of collateralization of flow within the overlying occipital bone (Figure 3). Neurosurgery did not recommend any surgical intervention. Follow up head MRI showed decrease in the size of the subdural empyema. Patient completed 6-week course of vancomycin and her symptoms improved.
Figure 1: MRI brain showing left subdural empyema.
Figure 2: MRI brain showing osteomyelitis within the overlying occipital bone.
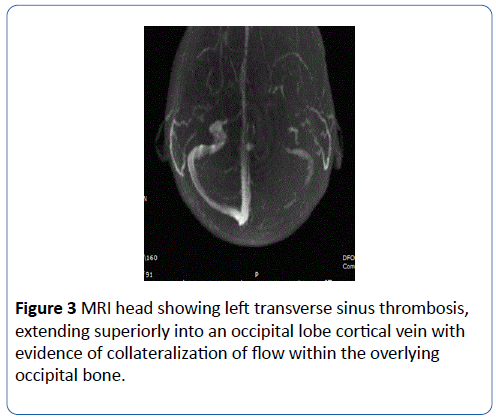
Figure 3: MRI head showing left transverse sinus thrombosis, extending superiorly into an occipital lobe cortical vein with evidence of collateralization of flow within the overlying occipital bone.
The patient in our case report developed bacteremia from MRSA due to significant IVDU and it had disseminated into the central nervous system. Treating CNS disease due to MRSA is challenging because of few therapeutic options, and difficulty in attaining therapeutic concentration of the drug in cerebrospinal fluid (CSF). Vancomycin is the main treatment, however in some patients vancomycin therapy fails because of its poor CSF penetration [1]. There are some cases where linezolid has been successful, due to its greater CSF penetration [2,3]. Even though there are many CNS disease occurring from MRSA, it is rare to find CNS disease development from community acquired MRSA. Hence, clinicians should have a high index of suspicion for subdural empyema in IVDUs who present with headaches and neck pain. Recognition and treatment of subdural empyema as a complication of bacteremia in IVDU is very important due to its complication rate. As evident in this case, thrombosis of the venous sinus can lead to venous occlusion and sometimes even brain infarction. Surgical and/or medical treatment should not be delayed.
18422
References
- Kessler AT, Kourtis AP (2007) Treatment of meningitis caused by methicillin-resistant Staphylococcus aureus with linezolid. Infection 35:271-274.
- Saito N, Aoki K, Sakurai T (2010) Linezolid treatment for intracranial abscesses caused by methicillin-resistant Staphylococcus aureus – two case reports. Neurol Med Chir 50:515-517.
- Naesens R, Ronsyn M, Druwé P (2009) Central nervous system invasion by community-acquired methicillin-resistant Staphylococcus aureus. J Med Microbiol58:1247-1251.