Background: Cryptococcal meningitis (CM) is associated with a high mortality rate among people living with HIV (PLHIV). CM often presents with subtle features delaying the diagnosis. The diagnosis of CM can be challenging, especially with limited access to the newer diagnostic techniques. This study compared the utility of various tests in the diagnosis of CM in a resource constrained setting.
Methods : In this prospective study conducted in a tertiary care public facility in New Delhi, India, PLHIV with chronic meningitis were screened for CM. A comparison of clinical assessment, Cerebrospinal fluid (CSF) analysis [cytology, biochemistry (sugar/protein), and microbiology (India ink staining/Latex Agglutination Test (LAT)], CSF and blood cultures and radiology (MRI brain) in 25 subjects of CM was done.
Results: The mean age of subjects was 37 ± 11.25 years and 88% were men. The mean BMI of subjects was 21.28 ± 3.65 kg/m2, 36% were undernourished. The mean CD4 count was 87 ± 66 cells/mm3 and 68% had CD4 count < 100 cells/ mm3. Headache (92%), vomiting (68%), fever (44%), altered consciousness (36%), and seizures (20%) were common symptoms. Median duration of headache (24 days) and fever (20 days) corroborated late presentation of patients. Cryptococcal antigen detection by Latex agglutination (LAT) in the CSF was the positive in 100%. The India ink staining of CSF was positive in only 60% of subjects. CSF culture isolated Cryptococcus in 64% cases. On MRI of the brain, only 28% had a normal scan and leptomeningeal enhancement was the commonest abnormality seen (28%).
Conclusions: CM can present with subtle findings- about 1/3rd patients do not have classical features of meningitis. Patients tend to present late; the paucity of CSF abnormalities further delays the diagnosis. India ink staining is useful in diagnosis in only 2/3rd of cases. Even though LAT is more expensive it should be the preferred diagnostic modality. Early clinical suspicion and antigen detection tests are recommended for the early and timely diagnosis of CM.
Keywords
Cryptococcal meningitis; Cerebrospinal fluid; Latex agglutination
Introduction
Cryptococcal meningitis (CM) is the most common central nervous system fungal opportunistic infection among people living with HIV (PLHIV). The annual incidence of CM is about one million cases a year and accounts for nearly 500000 deaths in sub Saharan Africa alone [1]. CM is associated with high case fatality and the 2-week mortality ranges from 35% to 65% in various studies even under optimum treatment conditions [2, 3]. The mortality rates are higher in the resource limited settings like Africa and India where the diagnosis is often delayed due to a combination of reasons: a lack of classical clinical features delaying clinical suspicion and inaccessibility of newer diagnostic techniques. The limited availability of Amphotericin B based treatment further contributes to increased mortality. The life expectancy of those who survive the initial episode of CM is very low due to secondary complications. With the availability of antigen based tests, the diagnosis of CM has become very easy and quick in the developed countries. The costs of these tests remain an important issue to be addressed in resource limited settings. The present study assessed the clinical spectrum of CM and compared the newer tests with the conventional tests for the diagnosis of CM.
Methods
This observational, descriptive study was conducted in the Department of Medicine and ART centre at the Maulana Azad Medical College and associated Lok Nayak hospital, New Delhi, India, a public health tertiary care facility, from October 2011 to April 2013. The study was approved by the Institutional Ethics Committee and subjects were recruited after prior informed consent. All PLHIV with history and/or clinical examination suggestive of chronic meningitis were evaluated for CM. Subjects with diabetes mellitus, malignancy, any end- organ failure or subjects taking cytotoxic agents and/or steroids were excluded. After a detailed clinical assessment including a neurological evaluation, all subjects underwent a lumbar puncture after a noncontrast CT scan of the head. Cerebrospinal fluid (CSF) collected was sent for cytological, biochemical and microbiological analysis.
The subjects were defined as a case of CM if they were symptomatic and fulfilled any one of the three criteria on CSF analysis:
1. Microscopic examination of CSF by India ink and Gram stain demonstrating Cryptococcus.
2. A Positive Latex agglutination test (LAT) for detection of capsular antigen in CSF. LAT was performed after collecting CSF supernatant by centrifugation at 1500 rpm for 15 minutes. The supernatant was heated in boiling water for 5 minutes. One drop of the supernatant was placed on the disposable card and 30 μL of CSF was added and the card was rotated at 100 rpm in a rotator. The card was read after 2 minutes and was considered positive if visible clumping was seen.
3. Isolation of Cryptococcus by culture of CSF in Sabouraud Dextrose Agar (SDA) at 22 and 37°C.
25 subjects fulfilling the case definition were enrolled in the study. They were further assessed with laboratory tests and MRI brain imaging. Treatment was given according to standard national protocol with Amphotericin B based induction phase (0.7 - 1.0 mg/kg) of 2 weeks, followed by consolidation and maintenance phases. The clinical features, findings of CSF analysis and laboratory parameters were analysed in the patients. A comparative assessment of the various microbiological tests for the diagnosis of CM was done. All subjects were followed up for 10 week to assess mortality. The descriptive data is presented as mean with standard deviation for continuous variables and as proportions for categorical variables.
Results
The mean age of subjects with CM was 37 ± 11.25 years (range- 21-58 years), 88% subjects were men, 12% were women and the majority of subjects were unskilled workers -36% subjects. The primary mode of HIV acquisition based on their self-reported history was heterosexual (64%), IV drug use (8%) and in 20% subjects, both IV drug use and heterosexual promiscuity and high risk behaviour. Suspected infected blood transfusion was reported by 8% subjects.
The mean BMI of the subjects was 21.28 ± 3.65 kg/m2 (range 16-28 kg/m2), and 36% (9/25) had a BMI < 18.5 kg/m2 (classified as under nutrition). The mean CD4 count of the subjects was 87 ± 66.89 cells/mm3 (range 10-216). Among the subjects, 44% had CD4 count < 50 cells/mm3, 24% had counts between 51-100 cells/ mm3 and 32% had CD4 counts > 100 cells/mm3.
Headache was most common presenting symptom of CM. It was found in 92% (23/25) of the subjects and most of them had severe headache. Vomiting (68%), fever (44%), and altered consciousness (36%) were the other prominent symptoms in the subjects. Seizures (20%), aphasia, focal neurological deficits and bilateral hearing loss (4% each) were also found. The mean duration of the symptoms is summarized in Table 1. Neck rigidity was the most common finding on neurological examination seen in 88% (22/25) subjects. The other neurological signs observed are summarised in Table 2.
| Symptom |
Duration (mean ± S.D.) |
Median duration |
Range |
| Headache |
49.34 ± 33.0 days |
24 days |
10–120 days |
| Fever |
19.8 ± 11.8 days |
10.0 days |
05 – 45 days |
| Vomiting |
6.4 ± 3.1 days |
4.0 days |
02 -12 days |
| Altered consciousness |
3.66 ± 2.44 days |
2 days |
02 – 10 days |
Table 1: Duration of symptoms of CM in the study subjects.
| Neurological examination findings |
n |
Percentage (%) |
| Disorientation |
9 |
36 |
| Altered consciousness |
6 |
24 |
| Neck rigidity |
22 |
88 |
| Positive Kernig’s sign |
17 |
68 |
| Hypertonia |
1 |
4 |
| Extensor plantar response |
6 |
24 |
| Focal neurological deficits |
5 |
20 |
| left sided hemiparesis |
2 |
8 |
| left 6th cranial nerve palsy |
1 |
4 |
| bilateral 6th cranial nerve palsy |
1 |
4 |
| left 7th nerve palsy |
1 |
4 |
| wernicke’s aphasia |
1 |
4 |
| broca’s aphasia |
1 |
4 |
Table 2: Neurological signs in PLHIV with CM.
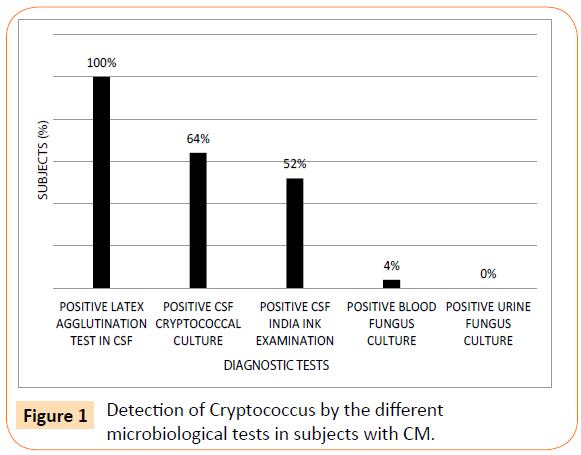
All subjects underwent a lumbar puncture and CSF was collected for cytological, biochemical and microbiological analysis. The CSF was evaluated for isolation / identification of Cryptococcus by India ink examination, LAT and culture on Sabaraoud’s Dextrose agar (SDA). Additionally, blood and urine were cultured for Cryptococcus in all subjects. The rates of detection of Cryptococcus by the various tests are depicted in Figure 1. The CSF latex agglutination test was most sensitive test to detect Cryptococcus species and was positive in 100% (25/25) of subjects. Culture of CSF demonstrated Cryptococcus in 64% (16/25) of cases. However, the India ink examination was positive in only 60% (15/25) of subjects.
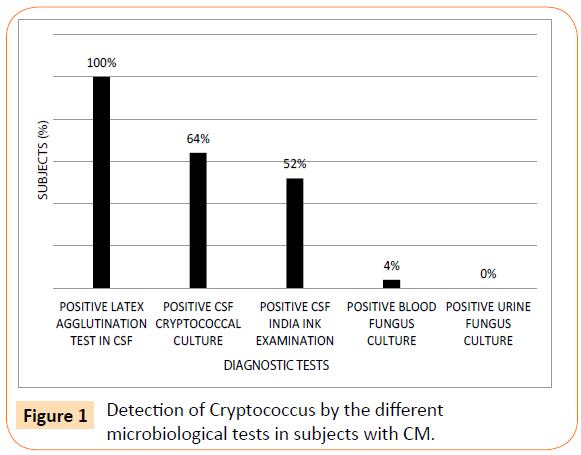
Figure 1: Detection of Cryptococcus by the different microbiological tests in subjects with CM.
All study subjects underwent Magnetic Resonance Imaging (MRI) of the brain during hospital stay. A normal MRI scan was seen in 28% (7/25) of subjects. In all the others, there was a demonstrable abnormality on the MRI. The most common MRI finding was leptomeningeal enhancement, found in 24% (6/25) of subjects. Cryptococcomas were observed in 20% subjects. The other MRI brain findings included prominent Virchow Robin spaces (16%), hydrocephalus (16%), infarcts (12%) and encephalomyelitis (4%). Though MRI findings were common, none were specific for CM and were similar to findings seen in other chronic meningitis like Tubercular meningitis.
In our study, many of the subjects had another opportunistic infection (OI) concurrent to CM. Pulmonary tuberculosis was most the common OI, present in the 32% of the subjects. Extrapulmonary tuberculosis in 12%, oral candidiasis in 8%, CNS toxoplasmosis in 4% and progressive multifocal leucoencephalopathy (PMLE) in 4% were the other OI observed.
CM was associated with high mortality: 56% (14/25) subjects died during in-hospital stay. Three more patients died during the 10 week period following discharge from the hospital.
Discussion
The mean CD4 count of the study subjects with CM was 87 ± 66 cells/mm3 and 68% subjects had CD4 count < 100 cells/mm3. Other previous studies have also demonstrated that low CD4 counts are associated with higher incidence of CM among PLHIV. The mean / median CD4 counts in previous studies have varied from 27 to 143 [4,5]. On further analysis of the study subjects, it was observed that the mean CD4 counts in the ART naive patients was 29 cells/ mm3 reflective of the advanced degree of immunosuppression in these patients. This also is indicative of the late presentation and diagnosis of HIV infection in the developing countries like India. The mean BMI of the study subjects was 21.28 ± 3.65 kg/m2 and 36% of them were undernourished i.e. had a BMI < 18.5 kg/m2. The subjects on ART had higher weight and BMI compared to the pre- ART subjects (23 kg/m2 versus 20 kg/m2) though this was not statistically significant.
Headache was the most prominent clinical manifestation among the study subjects (92%) and the median duration of headache was 24 days. In 8/25 patients, headache was present for more than 1 month. Fever of low grade was seen in 64% subjects with mean duration 19.8 ± 11.8 days. The classical signs of chronic meningitis were seen in only 2/3rd of the patients. Similar findings have been reported from other studies in Africa [6]. This emphasizes the need for a high index of suspicion of CM among PLHIV and an early lumbar puncture with CSF analysis are recommended.
MRI of the brain was performed in all subjects. Seventy six percent of the study subjects had an abnormal MRI brain at presentation. Leptomeningeal enhancement was most the common finding (24%), followed by Cryptococcomas in 20% and prominent Virchow Robin spaces in 16% of the subjects. In a study by Miszliel et al. on MRI findings in 25 subjects of CM, prominent Virchow Robin spaces were seen in 40% of the subjects [7]. On a repeat MRI in these patients, 9 had converted into Cryptococcomas. Mathews et al. in his study in patients with CM demonstrated that all patients had an abnormal MRI brain scan [8]. Though none of the findings are diagnostic or specific of CM, MRI of the brain provides good corroborative evidence. This is important to keep in mind since Tubercular meningitis is a close differential diagnosis to CM and its endemicity and prevalence are also high in the same regions.
For the diagnosis of CM, CSF analysis was a key diagnostic procedure. In many African countries, the availability of lumbar punctures and CSF analysis is a major limiting factor to the diagnosis of CM. We routinely perform lumbar punctures at our centre and it is an integral test in the approach to the diagnosis of patients with suspected meningitis. Though measurement of CSF opening pressures was not done in the study, it has been reported that increased CSF opening pressure is associated with increased mortality. Edward et al. analysed 82 subjects with CM with respect to the CSF opening pressure and elegantly deduced that the patients with higher CSF opening pressures had more altered mental status, more focal deficits, more requirement for ventricular shunts and increased mortality [9]. Interestingly, Bicanic et al. in their study demonstrated that patients with higher baseline fungal burden had higher baseline opening pressure [3]. They hypothesized that a high fungal burden appeared necessary but not sufficient for development of high intracranial pressure.
On microbiological analysis of CSF, India ink staining identified Cryptococcus in 60% of the study subjects. The reported India ink positivity in previous studies has been reported between 60 to 92%. Prolonged storage of the CSF sample, improper specimen transport and expertise of lab, has all been implicated but the exact cause is unknown. The India ink staining of CSF is widely used, especially in resource limited settings, as it is relatively inexpensive, easily available and requires little technical expertise of the lab. CSF culture was positive in 64% of the subjects and all isolates were Cryptococcus neoformans var. neoformans. A higher culture positive rate is indicative of a higher fungal burden in our study subjects. The latex agglutination test (LAT) for detection of Cryptococcus antigen was the most sensitive test to diagnose CM, being positive in the 100% of the study subjects. This corroborates with findings of other studies. Capoor et al. from India showed that the CSF latex agglutination test was 100% sensitive in detecting CM [10]. A similar very high sensitivity of Cryptococcal antigen detection has been reported in other studies [11].
The India ink staining of CSF for the diagnosis of Cryptococcus has low sensitivity. Though it is cheap and accessible in resource limited settings, its low rate of detection of Cryptococcus is a major drawback. If India ink screening had been used as the sole diagnostic test for CM, the diagnosis of CM would have been missed in 10/25 of the subjects. Fungal culture for the Cryptococcus is the gold standard but requires the expertise of lab, needs 3-5 days for a result, and is not available at the peripheral centres. This highlights the efficacy and utility of Cryptococcal antigen detection tests in CSF for the diagnosis of CM. The present study used the LAT for the detection of Cryptococcal antigen. The test is simple to use and does not require much technical expertise. Though slightly more expensive then the India ink staining, the advantages of the test in terms of sensitivity far outweigh the costs. The India ink test missed nearly 1/3 of cases of CM in the present study. Further, the treatment costs of one case of CM are approximately USD 2400 compared to the cost of 1 LAT test of approximately 3 USD. With the availability of lateral flow assay technique, the detection of cryptococcal antigen has become simpler and cheaper, and Cryptococcal antigen can now be performed as a point of care test. Also, in centres where it is feasible, quantitative measurement of Cryptococcal antigen in CSF offers additional prognostic value in patients with CM.
The detection of Cryptococcal antigen in the CSF has emerged as the diagnostic test of choice in CM. It is a very sensitive and specific test. False-positive Results may rarely occur with infections with Trichosporon, Stomatococcus and Capnocytophagus species. Other rare causes include disinfectants and soap [12]. False negative CrAg Results have been described in patients with very low fungal burden and due the phenomena of prozones and immune complex formation [13]. The National AIDS control programme in India relies on and recommends India ink staining as the preferred test for the diagnosis of CM. In view of the numerous advantages and much higher sensitivity, the programme should now consider recommending antigen detection in CFS routinely for the diagnosis of CM. This is even more so required in countries like India where Tuberculosis is endemic. The clinical presentation of CM is identical to tubercular meningitis, and a strong index of suspicion for the diagnosis of CM is essential. In fact among our study subjects, 12% were already receiving anti tuberculosis treatment for suspected tubercular meningitis and presented with worsening of clinical symptoms. These Results in a delay in diagnosis and relying on a less sensitive test such as India ink staining will further compromise the chances of a correct diagnosis of CM, contributing to increased mortality.
To conclude, CM is a serious opportunistic infection among PLHIV. It usually presents as a subacute to chronic meningitis but in about a third of patients, neurological examination may be unremarkable. A CSF analysis is crucial for the diagnosis of CM. Cryptococcal antigen detection is the most sensitive test for the diagnosis of CM and should be adopted as the diagnostic method of choice by India’s national programme.
Conflict of Interest
The authors declare that there is no conflict of interest. S. Anuradha, Mahaveer Singh, Ravinder Kaur and K. Rajeshwari were involved in the study design and protocol. S. Anuradha, Mahaveer Singh and Ravinder Kaur were involved in data collection. All were involved in data analysis, S. Anuradha, Mahaveer Singh and K. Rajeshwari in writing and the manuscript was approved by all
6498
References
- Park BJ,Wannemuehler KA, Marston BJ, Govender N, Pappas PG, et al. (2009) Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 23: 525-530.
- Lessells RJ,Mutevedzi PC, Heller T, Newell ML (2011) Poor long-term outcomes for cryptococcal meningitis in rural South Africa. S Afr Med J 101: 251-252.
- Bicanic T,Meintjes G, Wood R, Hayes M, Rebe K, et al. (2007) Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis 45: 76-80.
- Bicanic T, Harrison T (2010) Cryptococcus: Spectrum of Disease andTreatment. Pathogenic Yeasts. Springer 8:145-165.
- Pappas PG, Bustamante B, Ticona E, Hamill RJ, Johnson PC, et al. (2004) Recombinant interferon- gamma 1b as adjunctive therapy for AIDS-related acute cryptococcal meningitis. J Infect Dis 189: 2185-2191.
- Heyderman RS,Gangaidzo IT, Hakim JG, Mielke J, Taziwa A, et al. (1998) Cryptococcal meningitis in human immunodeficiency virus-infected patients in Harare, Zimbabwe. Clin Infect Dis 26: 284-289.
- Miszkiel KA, Hall-Craggs MA, Miller RF, Kendall BE, Wilkinson ID, et al. (1996) The spectrum of MRI findings in CNS cryptococcosis in AIDS. ClinRadiol 51: 842-850.
- Mathews VP,Alo PL, Glass JD, Kumar AJ, McArthur JC (1992) AIDS-related CNS cryptococcosis: radiologic-pathologic correlation. AJNR Am J Neuroradiol 13: 1477-1486.
- Edwards VE, Sutherland JM, Tyrer JH (1970) Cryptococcosis of the central nervous system. Epidemiological, clinical, and therapeutic features. J NeurolNeurosurg Psychiatry 33: 415-425.
- Capoor MR, Nair D, Deb M, Gupta B, Aggarwal P (2007) Clinical and mycological profile of cryptococcosis in a tertiary care hospital. Indian J Med Microbiol 25: 401-404.
- Shah HS, Patel DA, Vegad MM (2011) Evaluation of conventional and serological methods for rapid diagnosis of cryptococcal meningitis in HIV seropositive patients at tertiary care hospital. Nat J Comm Med 2: 354-357.
- Wilson DA,Sholtis M, Parshall S, Hall GS, Procop GW (2011) False-positive cryptococcal antigen test associated with use of BBL Port-a-Cul transport vials. J ClinMicrobiol 49: 702-703.
- Tanner DC, Weinstein MP, Fedorciw B, Joho KL, Thorpe JJ, et al. (1994) Comparison of commercial kits for detection of cryptococca l antigen. J ClinMicrobiol 32: 1680-1684.