Keywords
Low dose tamsulosin; Lower ureteric stones; Medical expulsive therapy
Introduction
Urolithiasis is an ancient disease with global distribution and has perplexed human beings and physicians for many centuries. Pakistan is situated in the middle of Afro-Asian stone belt, a high region of stone incidence [1]. Treatments for ureteric stones traditionally include watchful waiting, extracorporeal shock wave lithotripsy, ureteroscopy and open ureterolithotomy.
Minimally invasive techniques, such as shock wave lithotripsy and endourology, are now being used more frequently. Even minimally invasive surgery, however, is not free of complications and the cost is high [2]. Stone size and location are the main factors that can influence their passage; a stone smaller than 4 mm is usually passed after conservative treatment [2]. The human ureter contains a high number of α-adrenergic receptors, especially α1d -receptors at the lower part of the ureter [3,4].
Tamsulosin is a combined α1a- and α1d-selective adrenergic antagonist that is an alternative to other medications, such as calcium channel blockers, corticosteroids, and analgesic and anti-inflammatory drugs, for the treatment of distal ureteric stones [5-7]. The standard dose of tamsulosin for the treatment of distal uretic stones is 0.4 mg/day; many reports from Asian countries have confirmed that low-dose tamsulosin (0.2 mg/day) is effective in the treatment of benign prostatic hyperplasia (BPH) [5-7]. There are few published clinical studies dealing with lowdose tamsulosin for medical expulsive therapy for ureteral stones [8,9]. In a randomized controlled trial (RCT) the ureteral stones expulsion rate was 4%, 40% and 68% in control, low dose (0.2mg) and standard dose (0.4 mg) tamsulosin groups respectively [10]. In another RCT the stone expulsion rate was signi?cantly higher in low dose tamsulosin group than in control group (77% vs. 50%, P=0.002). No signi?cant differences were noted in the stone expulsion time and analgesic use between the groups [11]. There was a validity issue in the above mentioned studies as the sample sizes were and hence the results cannot be generalized [10,11]. Furthermore no local data is available on this topic locally and there is dearth of literature internationally as well. Therefore the present study is designed with proper calculation of sample size to assess the effectiveness of low dose tamsulosin, so that if founds to be effective then the same could be used in future with confidence in patients with lower ureteric stones.
The objective of the current study was to determine the effectiveness of low dose tamsulosin as a medical expulsive therapy in patients with lower ureteric stones.
Materials and Methods
Setting
Department of Urology, Liaquat University of Medical and Health Sciences Jamshoro.
Study design
Randomized controlled trial
Duration of study
6 months
Sample size
The sample size calculation was done on WHO calculator using reference 10 and considering one sided hypothesis
• Stone expulsion in low dose tamsulosin group was 40%
• Stone expulsion in control group was 4%
• Power of the test 99%
• Level of significance 5%
Sample size 76 patients that is 38/groups, however considering lost to follow up and stratification we will take a total of 100 patients having 50 patients in each groups.
Sample technique
Non-probability consecutive.
Sample selection
Inclusion criteria:
• Patients with stone size 4-10 mm determined on ultrasound
• Presence of stone in the lower 1/3rd of the ureter diagnosed as per operational definition
• either gender
• Age range 30-60 years
Exclusion criteria:
• urinary tract infection
• multiple stones
• pregnancy
• severe hydronephrosis
• hypotension
• ureteral stricture
• current use of calcium antagonists or alpha adrenergic blockers
Data collection procedure
Permission from the ethical review committee and informed consent from the patients was taken after explaining the purpose, procedure, risk and benefit of the study. to make two groups random allocation was done by a third person not involved in the study by asking patients to pick one sealed, opaque envelop bearing a card in it of group A and B. Group A patients was offered low dose tamsulosin (0.2 mg) one tablet daily in the morning for a maximum of 4 weeks and group B served as control. All patients were prescribed 50 mg diclofenac suppository on demand for pain relief. Patients were further advised to take minimum 2 liters of water daily. The patients were followed up on weekly basis along with X-ray KUB and ultrasonography. The final outcome was measured at the end of 4th week of treatment. Patients were instructed to note the time and the date of expulsion of stone. Absence of echoic shadows on lower 1/3rd of ureteric line on ultrasound was taken as effectiveness (expulsion of stone). The status of stone expulsion in terms of effectiveness and the demographics like age, gender, size of stone and time taken for stone expulsion was noted and entered in the questionnaire attached as annexure.
Data Analysis
Statistical Package for Social Sciences (SPSS) version 17was used for data entry and analysis. Frequency and percentages was calculated for gender and effectiveness (stone expulsion). Mean+SD was calculated for age, size of stone, duration of expulsion and BMI. The two groups were compared for effectiveness (stone expulsion), applying Chi square test and significance level was set at 0.05. Confounders and effect modifiers was controlled through stratification of age, gender, size of the stone and BMI, post stratification, chi-square test was applied.
Results
Baseline characteristics
Mean age of the patients in control group was 45.52 ± 6.70 years whereas mean age of the patients in low dose Tamsulosin was 46.72 ± 6.73 years (Table 1).
| Age of the patients (in years) |
Control |
Tamsulosin |
Mean difference |
95% c.i |
| mean ± sd |
mean ± sd |
| 45.52 ±6.70 |
46.72 ±6.73 |
-1.2 |
-3.8 to 1.46 |
sd= standard deviation
Table 1: Age of the patients n=100.
Mean BMI of the patients in control group was 30.16 ± 1.81 kg/ m2 whereas mean BMI of the patients in low dose Tamsulin was 29.56 ± 1.40 Kg/m2 (Table 2).
| Bmi (in kg/m2) |
Control |
Tamsulosin |
Mean difference |
95% c.i |
| mean ± sd |
mean ± sd |
| 30.16 ±1.81 |
29.56 ±1.40 |
0.60 |
-0.04 to 1.24 |
Table 2: Body mass index of the patients n=100.
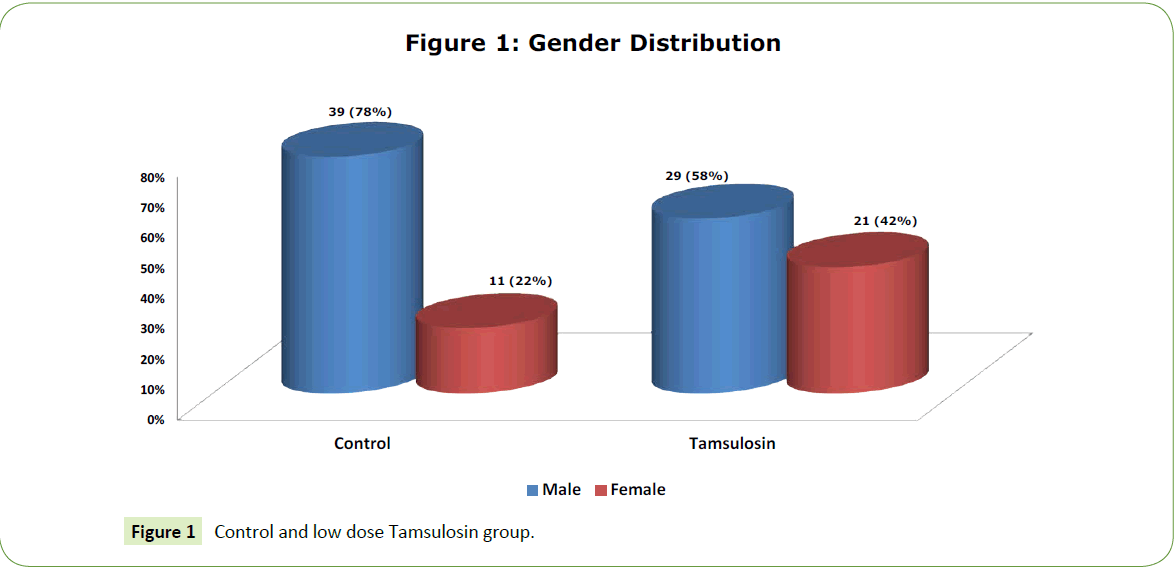
There were more male in both control and low dose Tamsulosin group, i.e. 39 (78%) and 21 (42%) respectively (Figure 1).
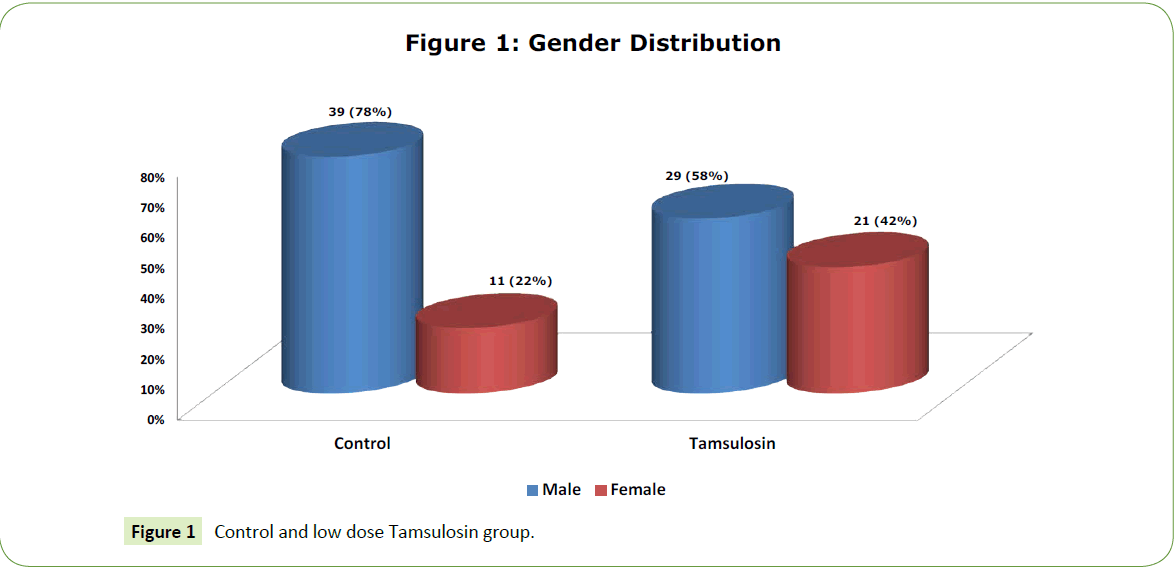
Figure 1: Gender Distribution
Mean stone size of the patients in control group was 6.16 ± 1.20 mm whereas mean stone size of the patient in low dose Tamsulin was 6.52 ± 1.19 mm (Table 3).
| Size of the stone (in mm) |
Control |
Tamsulosin |
Mean difference |
95% c.i |
| mean ±sd |
mean ±sd |
| 6.16 ±1.20 |
6.52 ±1.19 |
-3.6 |
-0.83 to 0.11 |
Table 3: Stone size of the patients n=100.
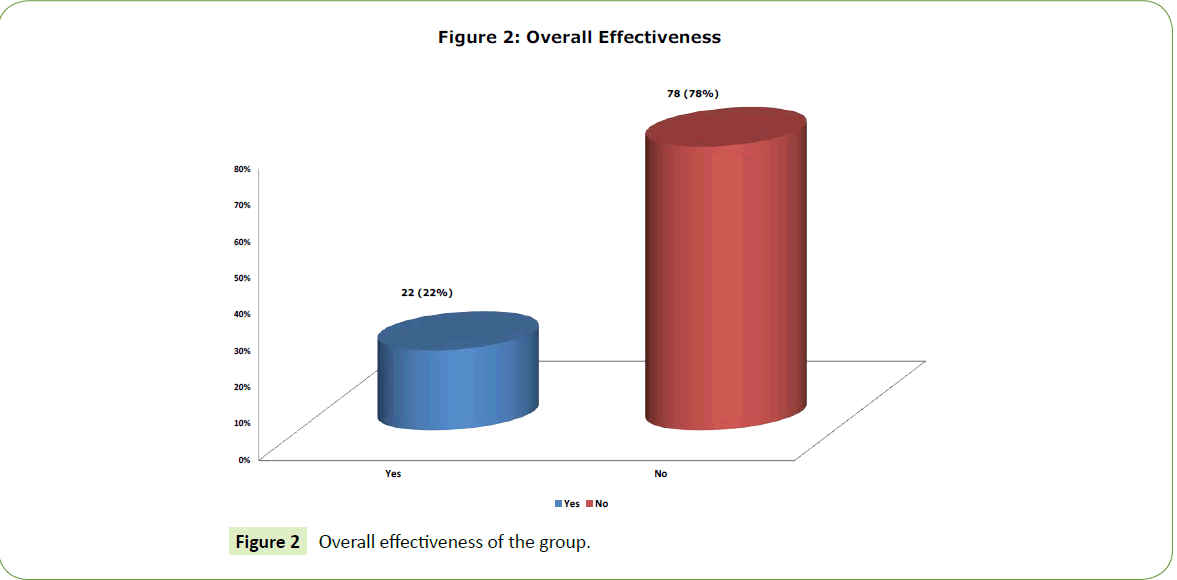
Outcome and expulsion
Mean duration of expulsion in control group was 30.66 ± 3.78 days whereas mean duration of explosion in low dose Tamsulosin was 28.47 ± 0.61 days. (Table 4) Overall effectiveness was found in 22 (22%) of the patients. (Figure 2) In control group effectiveness was found 3 (6%) patients whereas in low dose Tamsulosin group effectiveness was found in 19 (38%). Chi-square test was applied and statistically sufficient evidence of significant relationship was observed as p-value was found to be less than level of significance (p-value <0.001), as shown in Table 5. Stratification was done with respect to age, size of stone, BMI and gender. Chi-square test was applied and statistically sufficient evidence of significant relationship was observed except in stone >6 mm (p-value 0.201), as shown in Tables 6-13.
| Duration of expulsion (in days) |
n |
Control |
Tamsulosin |
Mean difference |
95% c.i |
| 3 |
mean ± sd |
mean ± sd |
| 19 |
30.66 ±3.78 |
28.47 ±0.61 |
2.19 |
0.46 to 3.91 |
Table 4: Duration of expulsion of stone among groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulosin |
| yes |
3 (6) |
19 (38) |
22 (22) |
| no |
47 (94) |
31 (62) |
78 (78) |
| total |
50 (100) |
50 (100) |
100 (100) |
Table 5: Comparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulosin |
| yes |
3 (7.5) |
14 (37.8) |
17 (22.1) |
| no |
37 (92.5) |
23 (62.2) |
60 (77.9) |
| total |
40 (100) |
37 (100) |
77 (100) |
Table 6 :≤45 years age groupcomparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulosin |
| yes |
0 (0) |
5 (38.5) |
5 (21.7) |
| no |
10 (100) |
8 (61.5) |
18 (78) |
| total |
10 (100) |
13 (100) |
23 (100) |
Table 7: >45 years age groupcomparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulosin |
| yes |
2 (5.1) |
14 (42.4) |
16 (22.2) |
| no |
37 (94.9) |
19 (57.6) |
56 (77.8) |
| total |
39 (100) |
33 (100) |
72 (100) |
Table 8: ≤6 cm stone sizecomparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulin |
| yes |
1 (9.1) |
5 (29.4) |
6 (21.4) |
| no |
10 (90.9) |
12 (70.6) |
22 (78.6) |
| total |
11 (100) |
17 (100) |
28 (100) |
Table 9: >6 gm stone sizecomparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulin |
| yes |
2 (5.7) |
12 (27.9) |
14 (17.9) |
| no |
33 (94.3) |
31 (72.1) |
64(78) |
| total |
35 (100) |
43 (100) |
78 (100) |
Table 10: ≤30 kg/m2bmi&comparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulin |
| yes |
1 (6.7) |
7 (100) |
8 (36.4) |
| no |
14 (93.3) |
0 (0) |
14 (63.6) |
| total |
15 (100) |
7 (100) |
22 (100) |
Table 11: >30 kg/m2 bmi &comparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulin |
| yes |
2 (5.1) |
11 (37.9) |
13 (19.1) |
| no |
37 (94.9) |
18 (62.1) |
55 (80.9) |
| total |
39 (100) |
29 (100) |
68 (100) |
Table 12: Male gender &comparison of effectiveness in both groups n=100.
| Effectiveness |
Group |
Total |
| Control |
Tamsulin |
| yes |
1 (9.1) |
8 (38.1) |
9 (28.1) |
| no |
10 (90.9) |
13 (61.9) |
23 (71.9) |
| total |
11 (100) |
21 (100) |
32 (100) |
Table 13: Female gender &comparison of effectiveness in both groups n=100.
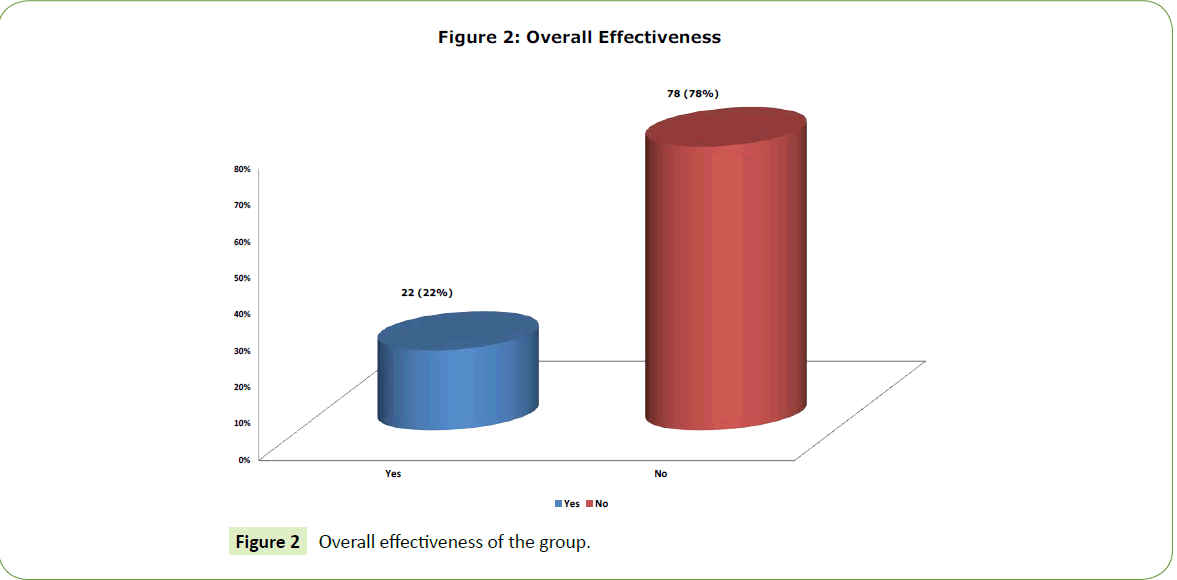
Figure 2: Overall effectiveness of the group.
Discussion
There are few published clinical studies dealing with low-dose tamsulosin for medical expulsive therapy for ureteral stones [8,9]. In a randomized controlled trial (RCT) the ureteral stones expulsion rate was 4%, 40% and 68% in control, low dose (0.2 mg) and standard dose (0.4 mg) tamsulosin groups respectively [10]. In another RCT The stone expulsion rate was signi?cantly higher in low dose tamsulosin group than in control group (77% vs. 50%, P=0.002). No signi?cant differences were noted in the stone expulsion time and analgesic use between the groups [11]. Improved detection of stones, increasing lifespan, and dietary changes may be related to the increased prevalence of stone disease [12,13]. A meta-analysis by the American Urological Association (AUA) Guidelines Panel determined that ureteral stones with a diameter of less than 5 mm will pass in up to 98% of cases [14]. For stones with diameters greater than 7 mm, the overall chance of spontaneous passage is low [15,16]. Overall passage rate is 25% for proximal, 45% for middle and 75% for distal ureteric stones [17]. In this study, Overall effectiveness was found in 22 (22%) of the patients. In control group effectiveness was found 3 (6%) patients whereas in low dose Tamsulin group effectiveness was found in 47 (94%). Chi-square test was applied and statistically sufficient evidence of significant relationship was observed as p-value was found to be less than level of significance (p-value <0.01). Time to spontaneous passage also depends on stone size, with stones up to 2 mm in size taking 8 days to pass and stones 4-6 mm taking 22 days to pass [18]. Most authors recommend that stone passage should not exceed 4-6 weeks due to the risk of renal damage [15,19]. Resim et al. did not identify a significant difference in distal stone passage rates between the tamsulosin and control groups. Similar expulsion rates were seen when patients with 6 mm stones were evaluated separately from those with stones larger than 6 mm [20]. In that trial, the average time to stone passage was not reported, the similar passage rates may be related to the longer treatment duration of 42 days, approaching the time when stone passage would spontaneously occur. A similar 28 day trial, conducted by Dellabella et al., analyzed not only expulsion rates, but also hospitalization and ureteroscopy rates in comparing the efficacy of tamsulosin with that of the antispasmodic agent phloroglucinol [21]. Both groups also received deflazacort 30 mg daily for up to 10 days and TMP/ SMX (80/400 mg) twice daily for 8 days. Mean stone size was significantly larger in the treatment group receiving tamsulosin than in the group receiving phloroglucinol, but the stone passage rate was significantly higher in patients treated with tamsulosin than in the phloroglucinol group. Tamsulosin therapy also significantly decreased the average time to passage of the stone. When adjusting for various patient factors, only treatment with tamsulosin predicted stone passage. Hospitalization rate was significantly lower with tamsulosin than with phloroglucinol (0% and 33%, respectively), and the ureteroscopy rate was similarly reduced (0% and 30%). Since phloroglucinol has significant antispasmodic effects, there was no true control group in this trial. Terazosin, another selective α-1 adrenergic antagonist, has also recently been shown to facilitate stone passage. Tekin et al., in a prospective randomized trial of 75 patients with distal ureteral stones ≤ 15 mm in width, found that patients treated with 5 mg terazosin daily for 4 weeks had a more statistically significant increase in stone passage rate than those patients receiving no treatment (77% vs. 46%). Treatment with terazosin was particularly effective for stones <8 mm, as a statistically significant increase in passage rate was noticed for this subgroup (95% vs. 56%). Drug-related side effects were minimal and no patient dropped out of the study [22]. After the expulsive efficacy of both nifedipine and tamsulosin had been reported, Porpiglia et al. compared the efficacy of nifedipine, tamsulosin, and control. The nifedipine and tamsulosin groups each received deflazacort 30 mg daily for 10 days and misoprostol 200 μg daily, and the control group received only symptomatic therapy [23]. The stone passage rates in the nifedipine and tamsulosin groups were similar (85 vs. 80%, respectively), but the differences between each of these groups and the control group (43%) were significant. Average time to stone passage was not significantly different between the nifedipine and tamsulosin groups, but the time to passage of the tamsulosin group was significantly shorter than that of the control group (12 days). Similarly, Dellabella et al. compared the expulsive efficacy of tamsulosin, nifedipine, and phloroglucinolall given with deflazacort 30 mg daily. Patients also received TMP/SMX 160/800 mg daily [24]. Despite the stones being significantly larger in the tamsulosin group, that group had a significantly higher stone passage rate than either the group receiving sustained-release nifedipine or the group receiving phloroglucinol. Median times to passage were significantly shorter with tamsulosin than with nifedipine and phloroglucinol (3 vs. 5 vs. 5 days, respectively). Rates of hospitalization were significantly less for tamsulosin than for nifedipine and phloroglucinol (1.4%, 20%, and 34.3%, respectively). A similar reduction in ureteroscopy rate with tamsulosin (1.4%) relative to nifedipine (20%) and phloroglucinol (31.4%) was noted. Treatment with tamsulosin also resulted in a significant reduction in median work days lost (2 days) compared with nifedipine (3 days) and phloroglucinol (5 days), and the median work days lost with nifedipine was significantly less than with phloroglucinol. The comparative efficacy of the α1-adrenoreceptor antagonists tamsulosin, terazosin, and doxazosin was evaluated in a controlled trial by Yilmaz et al. [25]. The control group had a significantly lower stone passage rate (53.57%) than did the treatment groups. Average time to stone passage was also significantly longer in the control group compared with the treatment groups. None of the patients in this trial received corticosteroids or antispasmodic agents, which permits more accurate assessment of the absolute efficacy of these specific agents. The authors concluded that all of these drugs appeared to be effective ureteral expulsive agents and that corticosteroid therapy may not be necessary. This theory that corticosteroids were not necessary for the expulsion of ureteral stones was further tested in a comparison of tamsulosin plus deflazacort with tamsulosin monotherapy [26]. Expulsion rates of the tamsulosin and tamsulosin/deflazacort groups at study end were similarly high. The median time to stone expulsion was shorter in the group receiving both tamsulosin and deflazacort (5 vs. 3 days). The rates of emergency department visits, hospitalizations, and lost work days were similar between the 2 groups. The authors concluded that the addition of deflazacort resulted in expulsion rates similar to those of tamsulosin alone, but that time to expulsion may be lessened. Several trials have shown the beneficial effect of expulsive treatment of ureteral stones with either nifedipine or tamsulosin. In 28 day trials, the rate of ureteral stone passage was 35-70% in the control groups compared with 77.1-80% in patients treated with nifedipine and 79.3-100% in patients treated with tamsulosin. Average time to stone passage in the control groups was 4.6-20 days, but only 5-9.3 days and 2.7-7.9 days in those receiving nifedipine and tamsulosin, respectively. The other α 1-adrenoreceptor antagonists, based on one trial, appear to have expulsion rates similar to those of tamsulosin [27].
Conclusion
In our study the effectiveness of low dose tamsulosin as a medical expulsive therapy in patients with lower ureteric stones was higher as compared to control.
19138
References
- Rizvi SA,Naqvi AA, Hussain Z, Hussain M, Zafar MN, et al. (2003) Management of pediatric urolithiasis in Pakistan: Experience with 1,440 children. J Urol169: 634-637.
- DellabellaM, Milanese G, Muzzonigro G (2003) Efficacy of tamsulosin in the medical management of juxtavesical ureteral stones. J Urol170:2202–2205.
- TroxelSA, Jones AW, Magliola L, Benson JS (2006) Physiologic effect of nifedipine and tamsulosin on contractility of distal ureter. J Endourol20:565–568.
- Sigala S, Dellabella M, Milanese G, Fornari S, Faccoli S, et al. (2005) Evidence for the presence of α adrenoceptor subtypes in the human ureter. Neurourol Urodyn 24: 142-148.
- Park CH, Chang HS, Oh BR (2004) Efficacy of low-dose tamsulosin on lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a nonblindmulticenter Korean study. Clin Drug Invest 24: 41-47.
- Li NG, Chen S, Yang XH (2003) Efficacy of low-dose tamsulosin in Chinese patients with symptomatic benign prostatic hyperplasia. Clin Drug Invest 23: 781-787.
- Lee E (2003) Comparison of tamsulosin and finasteride for lower urinary tract symptoms associated with benign prostatic hyperplasia in Korean patients. J Int Med Res 30: 584-590.
- Lojanapiwat B, Kochakarn W, Suparatchatpan N, Lertwuttichaikul K (2008) Effectiveness of low-dose and Lertwuttichaikul K. Effectiveness of low-dose and stones: a randomized controlled study. J Int Med Res 36: 529-536.
- Lojanapiwat B, Kochakarn W, Suparatchatpan N, Lertwuttichaikul K (2008) Effectiveness of low-dose and standard-dose Tamsulosin in the treatment of distal ureteric stones: A randomized controlled study. J Int Med Res 36:529-536.
- Kaneko T, Matsushima H, Morimoto H, Tsuzaka Y, Homma Y (2010) Ef?cacy of low dose tamsulosin in medical expulsive therapy for ureteral stones in Japanese male patients: A randomized controlled study. Int J Urol17:462-465.
- Stamatelou KK, Francis ME, Jones CA, Nyberg LM Jr, Curhan GC (2003) Time trends in reported prevalence of kidney stones in the United States,1976-1994. Kidney Int63:1817-1823.
- www.auanet.org/timssnet/products/guidelines/ main_reports/UreStnMain8_16.pdf.
- Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, et al. (2001) Guidelines on urolithiasis. EurUrol40:362-371.
- Hochreiter WW,Danuser H, Perrig M, Studer UE (2003) Extracorporeal shock wave lithotripsy for distal ureteral calculi:what a powerful machine can achieve. J Urol169: 878.
- Lotan Y, Gettman MT, Roehrborn CG, Caddeu JA, Pearle MS (2002) Management of ureteral calculi: a cost comparison and decision making analysis. J Urol167:1621-1629.
- Segura JW, Preminger GM, Assimos DG (1997) Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. The American Urological Association. J Urol158:1915-1921.
- Miller OF, Kane CJ (1999) Time to stone passage for observed ureteral calculi: a guide to patient education. J Urol162: 688-690.
- Ibrahim AI, Shetty SD, Awad RM, Patel KP (1991) Prognostic factors in the conservative management of ureteric stones. BJU 67:358-361.
- Tekin A, Alkan E, Beysel M (2004) Alpha-1 receptor blocking therapy for lower ureteral stones: a randomized prospective trial. J Urol 171: 1152.
- Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM (2004)Nifedipine versus tamsulosin for the management of lower ureteral stones. J Urol172:568-571.
- Dellabella M, Milanese G, Muzzonigro G (2005) Randomized trial of the efficacy of tamsulosin, nifedipine, and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J Urol174:167-172.
- Yilmaz E, Batislam E, Basar MM, Tuglu D, Ferhat M, et al. (2005) The comparison and efficacy of 3 different alpha-1-adrenergic blockers for distal ureteral stones. J Urol173:2010-2011.
- Dellabella M, Milanese G, Muzzonigro G (2005) Medical expulsive therapy for distal ureterolithiasis: randomized prospective study on role of corticosteroids used in combination with tamsulosin-simplified treatment regimen and health-related quality of life. Urology 66:712-715.
- Dellabella M, Milanese G, Muzzonigro G (2003) Efficacy of tamsulosin in the medical management of juxtavesical ureteral stones. J Urol170: 2202 – 2205.
- Troxel SA, Jones AW, Magliola L (2006) Physiologic effect of nifedipine and tamsulosin on contractility of distal ureter. J Endourol 20: 565-568.