Weh Kiat Gan*
Department of Haematology, Salford Royal Hospital, Salford Royal NHS Foundation Trust, Salford, Lancashire, UK
Corresponding Author:
Weh Kiat Gan
Department of Haematology, Salford Royal Hospital, Salford Royal NHS Foundation Trust, Salford, Lancashire M3 7BY, UK
Tel: +447719748479
E-mail: wehkiat@doctors.org.uk
Received: December 11, 2017; Accepted: December 28, 2017; Published: December 31, 2017
Citation: Gan WK (2017) Diagnostic Challenge of Heparin-Induced Skin Necrosis. Ann Clin Lab Res Vol.5: No.4:213. doi: 10.21767/2386-5180.1000213
Letter to Editor
Heparin has been widely used in both medical and surgical practices as effective prophylaxis and treatment for thromboembolic disorders. Heparin-induced skin necrosis (HISN) is a rare but potentially devastating complication of heparin therapy. Nevertheless, HISN can be a diagnostic challenge to clinicians in various ways.
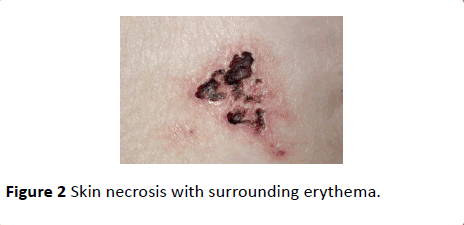
HISN classically presents with oedema and erythema, followed by blistering lesion (Figure 1) and formation of necrotic center at later stage (Figure 2). HISN typically occurs at injection sites but distant sites HISN have been infrequently reported [1]. Differentiating HISN from other necrotic drug eruptions is essential and can be challenging at early stage especially in patients with polypharmacy and absence of signs at injection sites. Heparin-induced skin necrosis usually occurs with marked swelling under the skin and visible blistering as a result of both dermal and epidermal involvement in contrast to fragile superficial bullae and haemorrhagic erosions in Stevens-Johnson syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), which characteristically limited to epidermal necrosis.

Figure 1: Violaceous blisters at injection sites.
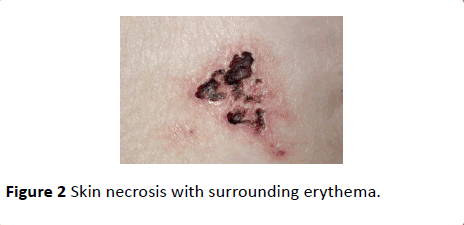
Figure 2: Skin necrosis with surrounding erythema.
Several mechanisms have been proposed leading to the occurrence of HISN including intravascular thrombosis as a result of Heparin-induced Thrombocytopaenia (HIT), cutaneous vasculitis caused by type III hypersensitivity syndrome (Arthus Phenomenon) and disruption of local vascular supply due to poor injection technique.
HISN has been classically associated with positive HIT antibodies and thrombocytopaenia. However, cases of heparin induced skin necrosis without presence of heparin platelet factor-4 antibody and HIT have been increasingly reported. [1] Skin biopsy would aid the diagnosis in these instances by demonstrating epidermal and dermal involvements with areas of necrotic tissues, infarctions, clots or evidence of vasculitis. Damage to dermal vascular supply due to poor injection technique has been proposed to be causing HISN.
Cautious monitoring of platelet counts should be executed in patients receiving heparin therapy, as most cases of HISN associated with HIT do not present with overt thrombocytopaenia (platelet count <150 × 109/L). A fall in platelet count of more than 50% from baseline would be indicative of HIT.
Onset of HISN can be variable and cases of HISN developing between 1 to 30 days post heparin therapy have been reported [1]. HIT can develop alongside, typically between 5 to 14 days following heparin therapy and within hours in previously sensitized patients [2,3]. The risk of thrombotic sequelae-systemic thromboembolism, skin necrosis can persist for up to three months due to circulating HIT antibodies developed post heparin exposure [4].
In summary, HISN is a rare adverse reaction of heparin therapy and early detection is essential as prompt cessation of heparin therapy and substitution with appropriate anticoagulant can prevent disease progression and avoid serious thrombotic complications.
Conflict of Interest
The author declares no conflict of interest.
21576
References
- Handschin AE, Trentz O, Kock HJ, Wanner GA (2005) Low molecular weight heparin-induced skin necrosis- a systemic review. Langenbecks Arch Surg 390: 249-254.
- Ahmed I, Majeed A, Powell R (2007) Heparin induced thrombocytopenia: diagnosis and management update. Postgrad Med 83: 575-582.
- Gan WK (2017) Delayed-onset heparin-induced skin necrosis: a rare complication of perioperative heparin therapy. BMJ Case Rep: 2017
- Zinkovsky DA, Antonopoulos MS (2008) Heparin-induced thrombocytopenia: overview and treatment. P T. 33: 642–651.