Introduction
Osteitis fibrosa cystica (brown tumor) is rare a clinical consequence of untreated severe primary or secondary hyperparathyroidism (HPT) [1]. Reported in about 3% of patients with primary HPT and 1.5% of those with secondary HPT disease [2].
Clinically, hyperparathyroidism (HPT) presents as stones, bones and groans. The stones refer to recurrent kidney stones. Bones refers to the bone lesions that occur in severe or prolonged cases. Groans are meant to describe the gastrointestinal symptoms of nausea, vomiting, peptic ulcers and pancreatitis. However, Up to one third of patients may be asymptomatic [3,4].
Hyperparathyroidism is frequently caused by a solitary adenoma in 80% of patients, multiple adenomas in 5%, parathyroid hyperplasia in 15%, and carcinoma in less than 1-5% [2,4].
Hypercalcemia is often discovered incidentally during routine laboratory testing hypophosphatemia and increased alkaline phosphatase level in blood may also be seen [3,4].
In daily practice, hip and thigh pain are commonly attributed to arthritis or soft tissue inflammation, however an unusual pain pattern should alert the clinician to search for underlying causes such as metabolic bone disease.
We herein present a case of primary HPT secondary to single adenoma and concurrent brown tumor that presented with persistent thigh pain ultimately femur fracture.
Case report
This is a case of a 35 year-old Indian lady who recently immigrated to Canada. She had an intermittent right-sided thigh pain, which gradually increase in severity over the course of four months. She had frequent visits to walk in clinic and emergency room in which pain was treated with analgesics. While attempting to get out bed, she sustained a mid-shaft fracture of the right femur.
She has previously been very active; she has not had any other fracture. There was no history of peptic ulcer, renal stone, increased thirst, urinary frequency, constipation, and weight loss. There was no exposure to radiation or industrial toxin. She takes only one dairy serving per day. She does not take calcium or vitamin D; she does not drink alcohol or smoke cigarettes. She never had a tumor diagnosed.
On physical examination, her head and neck were normal; no cervical adenopathy and no enlargement of the thyroid or nodularity palpable in the thyroid bed.
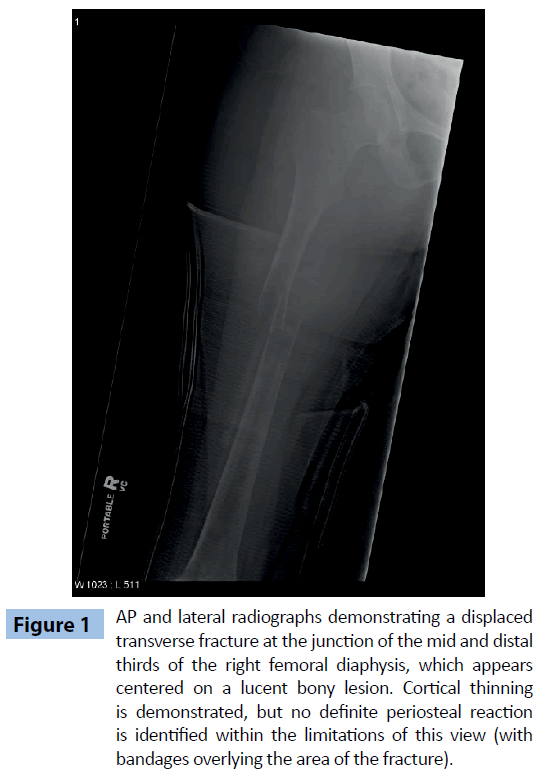
Her radiograph showed cortical thinning within the mid diaphysis of the femur (Figure 1).
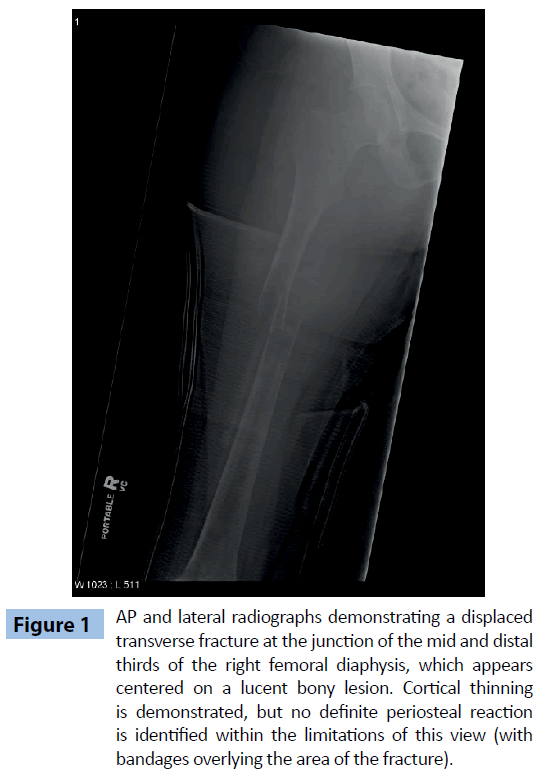
Figure 1: AP and lateral radiographs demonstrating a displaced transverse fracture at the junction of the mid and distal thirds of the right femoral diaphysis, which appears centered on a lucent bony lesion. Cortical thinning is demonstrated, but no definite periosteal reaction is identified within the limitations of this view (with bandages overlying the area of the fracture).
Curettings from the right femur medullary canal revealed giant cells with no evidence of fibrous dysplasia or malignancy.
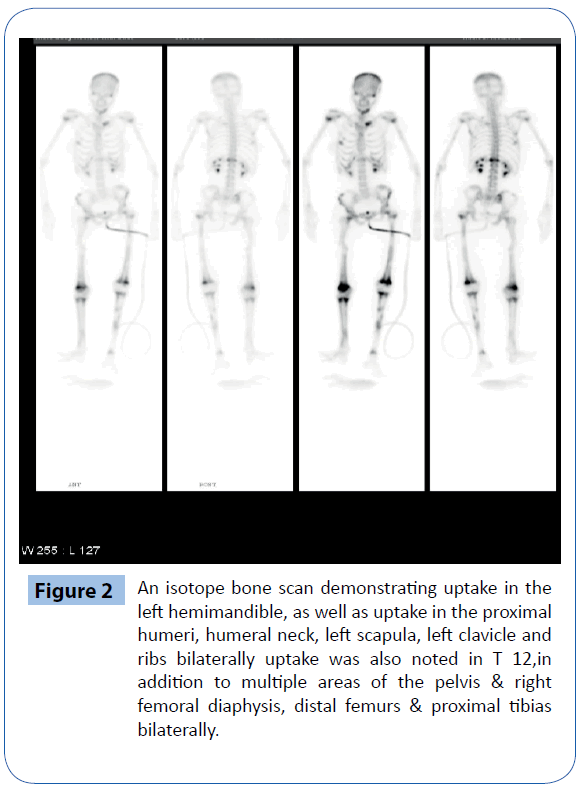
An isotope bone scan showed left hemimandible uptake, as well as uptake in the proximal humeri, humeral neck, left scapula, left clavicle and ribs bilaterally uptake was also noted in T 12,in addition to multiple areas of the pelvis and right femoral diaphysis, distal femurs and proximal tibias bilaterally (Figure 2).
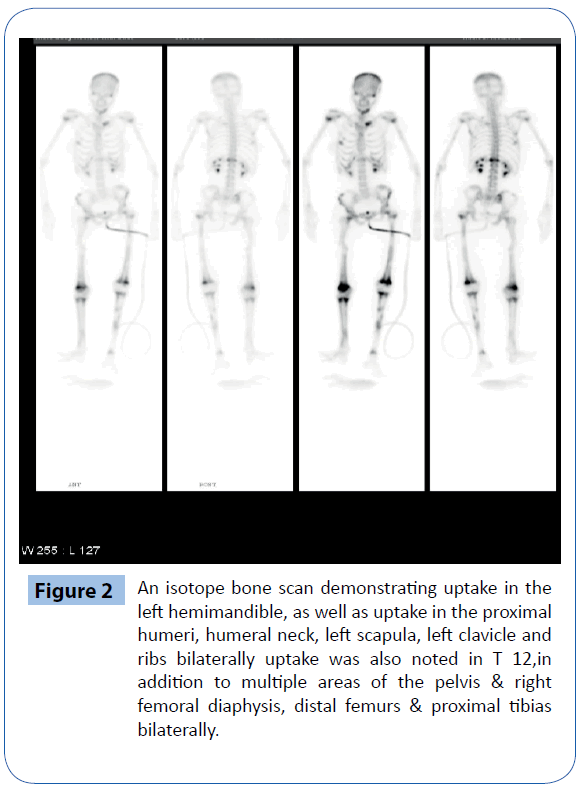
Figure 2: An isotope bone scan demonstrating uptake in the left hemimandible, as well as uptake in the proximal humeri, humeral neck, left scapula, left clavicle and ribs bilaterally uptake was also noted in T 12,in addition to multiple areas of the pelvis & right femoral diaphysis, distal femurs & proximal tibias bilaterally.
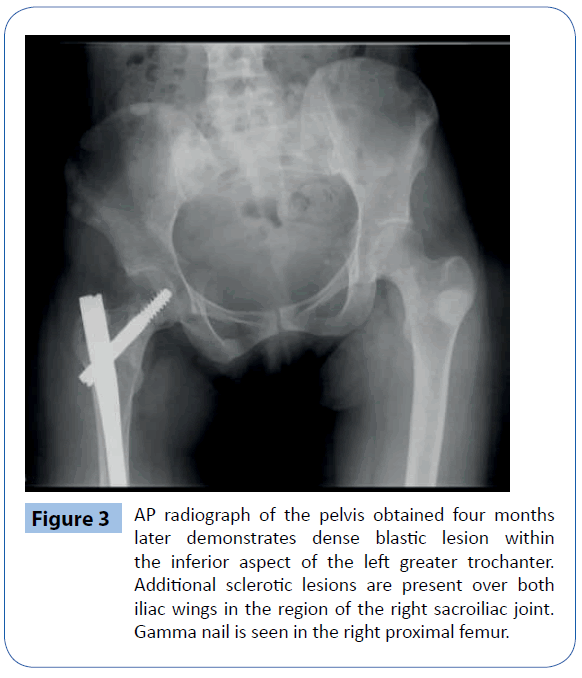
Radiographs obtained four months later demonstrates dense blastic lesion within the inferior aspect of the left greater trochanter. Additional sclerotic lesions are present over both iliac wings in the region of the right sacroiliac joint. Gamma nail remains is seen in the right proximal femur (Figure 3).
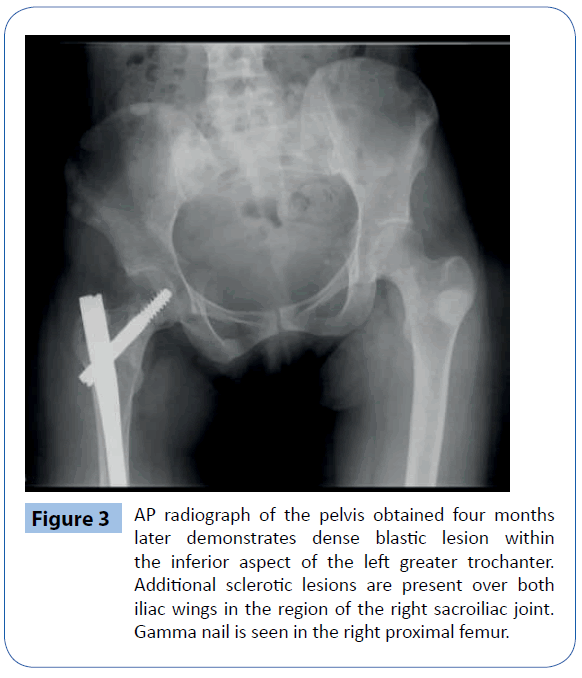
Figure 3: AP radiograph of the pelvis obtained four months later demonstrates dense blastic lesion within the inferior aspect of the left greater trochanter. Additional sclerotic lesions are present over both iliac wings in the region of the right sacroiliac joint. Gamma nail is seen in the right proximal femur.
Parathyroid scan showed an increased activity at the inferior pole of the left lobe, with delayed washout. There are no other reproducible abnormalities to suggest parathyroid abnormality elsewhere.
The serum level of calcium was markedly elevated at 3.79 mmol/L (normal range 2.10-2.55mmol/L), phosphorus level was low at 0.72 mmol/L (normal 0.80-1.40 mmol/L). Parathyroid hormone was elevated at 160 Pmol/L (normal<6.4). Serum alkaline phosphate was high at 258 U/L (normal 48-138 U/L). Co-existing Vitamin D deficiency was noted at 23 nmol/L (reference range 75-150 nmol/L).
Neck exploration revealed 1.2 x 1.2 cm left inferior parathyroid adenoma, which has been resected and histopathology confirmed parathyroid adenoma. Patient tolerated the surgery very well. Subsequently, her PTH post operatively returned to normal at 0.9 Pmol/L as well as the ionized calcium at 1.07 mmol/L (reference range: 1.03-1.23 mmol/L).
At four months follow-up, L2-4 bone mineral density was 0.688 g/cm2, which was 3.5 standard deviations below age matched. Total hip bone density was 0.627 g/cm2, which was 2.5 standard deviations below age matched and distal third of radius was 0.377 g/cm2, which was 3.5 standard deviations below age matched. Follow up bone mineral density 1 year later showed that total hip BMD is 0.851 g/cm2, which is 0.7 standard deviations below age matched, reflecting a significant increased by 35.8% from previous.
Discussion
In 1891, Von Recklinghousen described the classic bone disease termed osteitis fibrosa cystic. In 1925, the Viennese surgeon Mandl performed the first parathyroid exploration and adenoma resection. Mandl noted improvement of the patient’s severe skeletal abnormalities post operatively, thereby linking HPT with bone disease. Albright later in 1930s described the clinical entity of classic primary HPT on the basis of 17 cases from his clinical practice [5].
The term “Brown Tumor” is a misnomer, because it is not a true neoplasm. It is represents a localized accumulation of osteoclast, fibrous tissue and blood. High hemosiderin content gives the lesion characteristic brown color so it’s called Brown tumor [3].
Brown tumor of the bone typically involves the jaws, clavicle, ribs, pelvic bone and infrequently the long bone such as the femur. There have been occasional reports of involvement of the femur [6-18] and one report in pediatric patient [19].
Diagnostic confusion arises mainly when the clinician encounters multiple lytic lesions involving different areas of the skeleton, as was the case in our patient. Metastatic bone tumor is a rational consideration whenever multiple osteolytic lesions are found. However, serum calcium, phosphate and PTH level should be checked before the whole set of tumor survey is initiated, Although hypercalcemia with high intact PTH level and imaging evidence of parathyroid adenoma all indicated that brown tumor is highly possible, the definite diagnosis is histopathology of bone biopsy, which will reveal a dense fibroblastic stroma, area of cystic degeneration, osteoid, microfractures, hemorrhage, macrophages with hemosiderin, and multinucleated osteoclastic gaint cells.
Brown tumor has similar radiologic features seen in other cystic bony lesions such as giant cell tumor, fibrous dysplasia and aneurismal bone cyst. Differentiating between a brown tumor and other giant cell tumor may be very difficult, even with histology. However, after treatment of hyperparathyroidism, brown tumors may heal with calcification, sclerosis and subsequently lesion disappearance [20].
Vitamin D insufficiency is common in patients with primary HPT and may be associated with more severe and progressive disease. Epidemiological studies suggest that vitamin D deficient patients with HPT have higher level of PTH and markers of bone turnover, larger parathyroid adenomas, and more frequent fractures than vitamin D replenished patients [21]. Vitamin D repletion reduces levels of PTH and bone turnover in HPT [22].
7710
References
- Yilmazlar S, Arslan E, Aksoy K, Tolunay S (2004) Sellar-parasellar brown tumor: case report and review of literature. Skull Base 14: 163-168.
- Grégoire C, Soussan M, Dumuis ML, Naggara N, Martin A, et al. (2012) Contribution of multimodality imaging for positive and aetiological diagnosis of multiple brown tumours. Ann Endocrinol (Paris) 73: 43-50.
- Delbridge LW, Younes NA, Guinea AI, Reeve TS, Clifton-Bligh P, et al. (1998) Surgery for primary hyperparathyroidism 1962-1996: indications and outcomes. Med J Aust 168: 153-156.
- Morgan G, Ganapathi M, Afzal S, Grant A.J (2002) Pathological fractures in primary hyperparathyroidism: a case report highlighting diagnostic difficulties. Injury 33: 288-289.
- Albright F, Aub JC, Bauer W (1934) Hyperparathyroidism, a common and polymorphic condition as illustrated by seventeen proved cases from one clinic. JAMA 102:1276-1287.
- Younes NA, Mahafza WS, Agabi SS (2004) Brown tumor of the femur associated with double parathyroid adenomas. Saudi Med J 25: 1701-1703.
- Radulescu D, Chis B, Donca V, Munteanu V (2014) Brown tumors of the femur and pelvis secondary to a parathyroid carcinoma: report of one case. Rev Med Chil 142: 919-923.
- Hsieh MC, Ko JY, Eng HL (2004) Pathologic fracture of the distal femur in osteitisfibrosacystica simulating metastatic disease. Arch Orthop Trauma Surg 124: 498-501.
- Hussain A, Mahmood H, Geddoa E, Hamish M, Reda AH (2008) Parathyroid adenoma and hypercalcemia in a patient presenting with multiple pathological fractures of the long bones. Int J Surg 6: 465-468.
- Suchecki G, Szudejko B (1999) [Diagnostic difficulties in primary hyperparathyroidism: a case report]. Chir Narzadow Ruchu Ortop Pol 64: 81-83.
- Yalçin MB , Hiz M, Unlü MC, Dervisoglu S,Kanberoglu K, Bilge I, Ercan O (2008) [A case of brown tumor mimicking fibrous dysplasia in a patient with chronic renal failure]. Acta Orthop Traumatol Turc 42: 296-301.
- Pérez JA, López B, Valdivia P, Norambuena L (1989) [Pathologic fracture of the femur due to primary hyperparathyroidism]. Rev Med Chil 117: 1018-1022.
- Goerlich R (1983) [Left spontaneous femoral fracture in primary hyperparathyroidism and postgastrectomy bone disease following a Billroth II stomach resection]. Chirurg 54: 600-604.
- Meydan N, Barutca S, Guney E, Boylu S, Savk O, et al. (2006) Brown tumors mimicking bone metastases. J Natl Med Assoc 98: 950-953.
- Al-Homrany M, Grillo IA, Al-Ghamdi B, El-Tahir M, Malatani TS, et al. (1998) Diffuse pulmonary calcinosis& multiple soft tissue calcification in renal failure patient with pathological femoral fracture. Indian J Chest Dis Allied Sci 40: 205-211.
- Wallace E, Day M, Fadare O, Schaefer H (2013) Pathologic femur fracture due to a brown tumor in a patient with secondary hyperparathyroidism and vitamin D-resistant rickets. Am J Kidney Dis 61: 337-341.
- Younes NA, Mahafza WS, Agabi SS (2004) Brown tumor of the femur associated with double parathyroid adenomas. Saudi Med J 25: 1701-1703.
- Tayfun H, Metin O, Hakan S, Zafer B, Vardar AF2 (2014) Brown tumor as an unusual but preventable cause of spinal cord compression: Case report and review of the literature. Asian J Neurosurg 9: 40-44.
- Mitchell D, Rybak LP, Glatz FR (2004) Hyperparathyroid crisis in a pediatric patient. Int J Pediatr Otorhinolaryngol 68: 237-241.
- Murphey MD, Sartoris DJ, Quale JL, Pathria MN, Martin NL (1993) Musculoskeletal manifestations of chronic renal insufficiency. Radiographics 13: 357-379.
- Silverberg SJ, Shane E, Dempster DW, Bilezikian JP (1999) The effects of vitamin D insufficiency in patients with primary hyperparathyroidism. Am J Med 107: 561-567.
- Grey A, Lucas J, Horne A, Gamble G, Davidson JS, et al. (2005) Vitamin D repletion in patients with primary hyperparathyroidism and coexistent vitamin D insufficiency. J Clin Endocrinol Metab 90: 2122-2126.