Melissa Rae LeBlanc*, Emma Pieris and Michelle Thompson
Oregon Health and Science University, Portland, Oregon, United States
Corresponding Author:
Melissa Rae LeBlanc
Oregon Health and Science University
Portland, Oregon, United States
Tel: (503) 494-8311
E-mail: leblanme@ohsu.edu
Received date: October 07, 2017; Accepted date: October 12, 2017; Published date: October 16, 2017
Citation: LeBlanc MR, Pieris E, Thompson M (2017) Digoxin Toxicity Awareness: When Fatigue isn’t what You Think. Arch Med Vol No:9 Iss No:5:5
Copyright: © 2017 LeBlanc MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Digoxin; Toxicity; Digoxin immune fab; Digibind
Introduction
Use of digoxin, a cardiac glycoside, treating atrial fibrillation and heart failure has reduced over the last two decades, as have rates of hospitalization for digoxin toxicity [1] though the therapeutic window remains narrow as ever. Toxicity may be acute or chronic and symptoms include lethargy, somnolence, confusion, anorexia, nausea, vomiting, diarrhea, visual disturbances and a wide variety of cardiac arrhythmias which can occur simultaneously [2,3].
Toxicity more often occurs at higher serum concentrations, but can occur in some populations at lower serum concentrations, particularly the elderly or those with renal disease [3-6]. Decreased use of digoxin and concurrent decrease in the incidence of toxicity has led to decreased awareness and recognition of this toxicity, which may delay treatment with digoxin immune fab, increasing morbidity and mortality [5,6].
Case Presentation
An elderly man with history of atrial fibrillation on metoprolol, digoxin and warfarin; also with diabetes, chronic kidney disease and ulcerative colitis status post colectomy presents with three weeks of progressive fatigue, malaise, muscle weakness, anorexia, confusion, nausea and vomiting and worsening of baseline diarrhea after experiencing viral upper respiratory symptoms one month prior, which had since resolved. Physical exam revealed episodes of intermittent symptomatic bradycardia (heart rate in the thirties) alternating with tachycardia with persistent atrial fibrillation. Labs revealed hyperkalemia (5.7), acute kidney injury (AKI) with a creatinine of 3.1 from baseline of 1.8, mild leukocytosis without left shift (12.7) and digoxin level of 1.8 ng/ml (reference range 0.5-2.0 ng/ ml).
Computed Tomography (CT) of the head without contrast was unremarkable and initial EKG showed prominent T waves in precordial leads. He was admitted to the medical intensive care unit (ICU) for altered mental status, hyperkalemia and AKI. While in the medical ICU he was placed on telemetry, treated with intravenous fluid resuscitation, and his furosemide, aldactone and digoxin were held due to AKI and hyperkalemia, as was metoprolol given bradycardia.
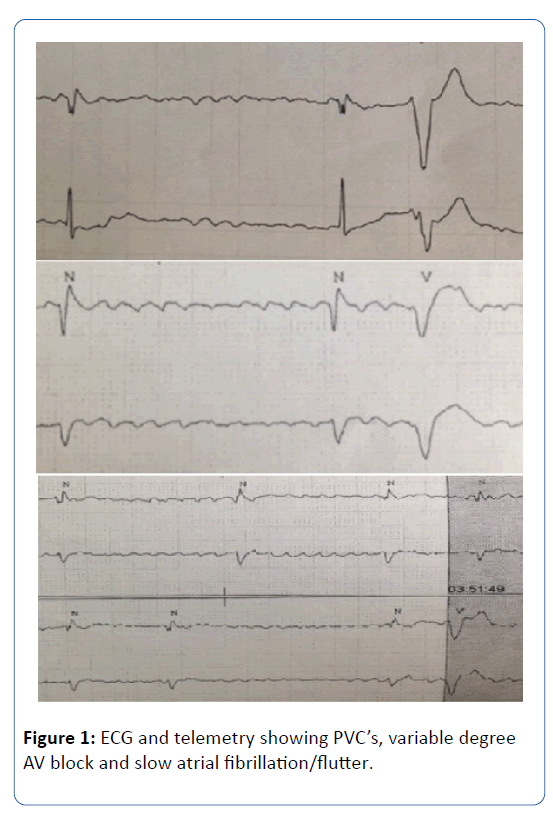
He had improvement in his hyperkalemia (4.6) and mild improvement in his creatinine (2.9). He was subsequently transferred to the general medical floor on the second day of his admission where he continued to have notable muscle weakness, confusion, nausea, vomiting and poor appetite. Review of telemetry showed atrial tachycardia with intermittent AV nodal block, ventricular ectopy evidence by frequent premature ventricular contractions (PVCs) as well as slow ventricular response to atrial fibrillation (Figure 1).
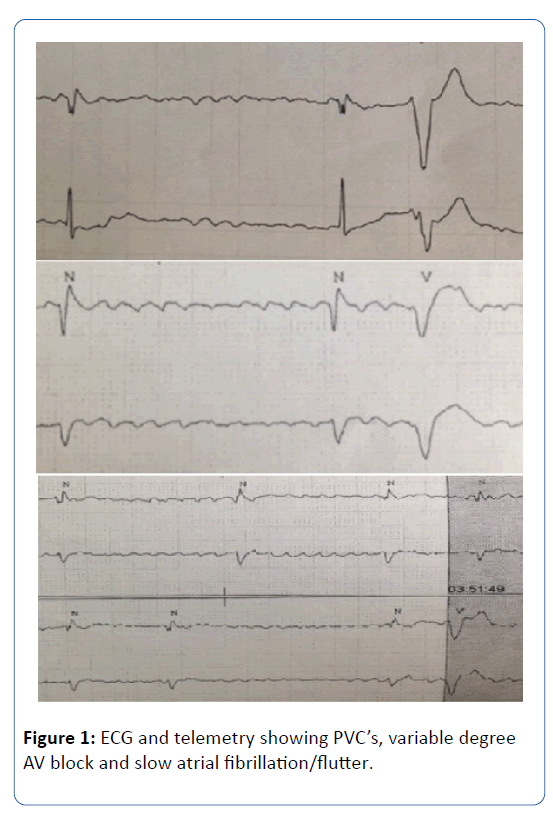
Figure 1: ECG and telemetry showing PVC’s, variable degree AV block and slow atrial fibrillation/flutter.
The confluence of his symptoms, telemetry and risk factors made this case clinically concerning for digoxin toxicity. He was treated with 2 vials of Digoxin immune fab. He responded well with improvement in creatinine from 2.9 to 1.9 the same day, stable potassium, improved mental status, resolution of his nausea and vomiting, improved appetite and improvement in weakness. Telemetry also normalized with resolution of PVC’s, bigeminy and AV blockade to his baseline atrial fibrillation with adequate rate control.
Discussion
It is unclear whether this patients case represents chronic toxicity in an elderly man with chronic kidney disease and diuretics use or whether his recent URI resulted in dehydration and acute worsening of his renal function leading to acute toxicity. Given the constellation and severity of symptoms it was felt that he warranted treatment with digoxin immune fab. This patient had a digoxin level was 1.8 on presentation, while not supra-therapeutic (by lab standards), toxicity can occur at lower serum levels, particularly in elderly populations, persons with renal disease, or with concurrent use of diuretics [3,6]. All of these risk factors were present in this patient. As serum level is not always an indicator of toxicity, the clinical symptoms and patient risk factors should be considered.
Dosing of digoxin immune fab varies depending on whether the toxicity is acute or chronic. In acute digoxin toxicity previous recommendations were use of equimolar dosing, with dosing based on amount ingested, weight, and serum concentration [7]. However, a recent study by Chan and Buckley suggest that 80 mg (2 vials) may be sufficient to stabilize acute toxicity with repeat dosing for recrudescence as needed based on symptoms (hyperkalemia, ECG changes, free digoxin levels). For chronic toxicity 3 vials are generally sufficient and can empirically be given 1 vial at a time. If no benefit within an hour, then additional vials may be given. This is particularly important in the setting of renal disease with reduced volume of distribution of the digoxin immune fab [4]. By using this dosing method cost can be reduced.
While the use of digoxin and incidence of toxicity have decreased [1], the clinical importance of this toxicity has not, and it still has significant potential for morbidity and mortality. Awareness and recognition of this toxidrome with prompt treatment, now with reduced dosing and less financial burden, should be advocated.
20834
References
- Haynes K (2008) Declining public health burden of digoxin toxicity from 1991 to 2004. Nature 84: 90-94.
- Ehle M, Patel C, Giugliano RP (2011)Digoxin: Clinical highlights. CritPathwCardiol10: 93-98.
- Chan BSH, Buckley NA (2014) Digoxin-specific antibody fragments in the treatment of digoxin toxicity. ClinToxicol52: 824-836.
- Megarbane B, Baud FJ (2014) Early Digoxin-specific antibody fragments for treating patients at risk of life-threatening digoxin toxicity. ClinToxicol52: 985-986.
- Goldberger ZD, Goldberger AL (2015) Therapeutic ranges of serum digoxin concentrations in patients with heart failure. Am J Cardiol109: 1818-1821.
- AntmanEM (1990) Treatment of 150 cases of life-threatening digitalis intoxication with digoxin-specific fab antibody fragments. Circulation 81: 1744-1752.