Keywords
Intracranial artery stenosis, Extracranial artery stenosis, Transcranial Doppler, Carotid duplex ultrasound
Introduction
Stroke is a heterogeneous diseases caused by a variety of pathophysiological mechanisms. Hitherto, it remains one of the primary reasons leading patients to death and hospitalization in European countries. In the United States, stroke is viewed as the third largest disease leading to death [1,2]. Similarly, the morbidity and mortality of cerebrovascular disease in China is significantly higher than that of cardiovascular disease [3]. Therefore, the prevention of stroke is of great importance. As the intracranial and/or extracranial artery stenosis is an important risk factor for ischemic stroke, the screening of these arteries draws our attention. However, there are marked differences in the distribution of arterial lesions among different populations [4-7]. In white individuals, the extracranial artery stenosis (usually the carotid artery stenosis) is a common cause of cerebral ischemia; in contrast, intracranial large-artery stenosis is the predominant vascular lesion found in patients of Asian, African, or Hispanic ancestry [5-7]. A number of methods may be used to identify stenosis of intracranial and extracranial arteries. However, digital subtraction angiography (DSA) serves as a gold standard, though with the disadvantages of invasive nature and the risk of perioperative complications. In this regard, transcranial Doppler sonography (TCD) and carotid duplex ultrasound have unique advantages in intracranial and extracranial artery evaluation including its noninvasiveness and high sensitivity and specificity [8-10]. Although racial predilection with reference to stenosed artery distribution has been recognized, distribution of intra- and extra-cranial artery stenosis with reference to age and sex has not been clarified which might contributed to the individualized prevention or therapy of stroke. In this study, we aim to explore intracranial and extracranial artery stenosis in a large northeast Chinese cohort by utilizing TCD and carotid duplex ultrasound. Our study relied on our excellent team with high professional ultrasound technology to carry out intracranial and extracranial artery stenosis screening. We expect to provide important basis for screening of intracranial and extracranial artery stenosis in the northeast Chinese population.
Subjects and Methods
Study setting
The study was conducted in the department of neurology of the first Hospital of Jilin University, which is the largest neurology department in northeast China. The Ultrasound Laboratory in the department of neurology is one of the four training centers in China and possesses 10 TCD and 3 carotid duplex machines.
Subject
This study was approved by the ethics committee of the first hospital of Jilin University, Changchun, China. And written informed consent was obtained from all subjects. From January to December 2012, both the outpatients and hospitalized patients who visited our ultrasound laboratory and simultaneously received paired examinations with TCD and carotid duplex ultrasound in our hospital were enrolled. At baseline, we recorded the demographic data including sex, age, and the common vascular risk factors, such as previous history of hypertension, diabetes mellitus, smoking, dyslipidemia, ischemic heart disease. Hypertension, ischemic heart disease and diabetes mellitus were respectively diagnosed by cardiologists and diabetologists.
Inclusion criteria and exclusion criteria
Subjects who received paired examinations with TCD and carotid duplex ultrasound simultaneously in the Ultrasound Laboratory were enrolled. Subjects were excluded if they met the following criteria: presence of a poor temporal acoustic window; could not consent to participate in the study, such as the subjects in an agitated or confused state, presented with orthopnea, or had a neck surgery or trauma, etc. Patients with artery stenosis caused by Moyamoya disease, Takayasu arteritis, vascular amyloidosis, fibromuscular dysplasia, vascular malformation, dissecting aneurysm, intracranial infection and other reasons were also excluded.
Protocol of TCD and carotid duplex ultrasound
For all the recruited subjects, the intracranial and extracranial arteries were assessed by TCD (EMS-9, Delicate, China) and carotid duplex ultrasound (iU22, Philips, USA). TCD examinations were performed with 2 MHz probe to detect middle cerebral artery (MCA)-Ml, anterior cerebral artery (ACA)-Al, posterior cerebral artery (PCA) and intracranial segment of internal carotid artery (including siphon and terminal segments) through the temporal window, intracranial segment of vertebral artery (VA) and basilar artery (BA) through the pillow window, and the ophthalmic artery and the siphon segment of internal carotid artery through the eye window. As to extracranial arteries, the L3-9 MHz linear array probe and C5-1 MHz convex array probe were used to detect bilateral carotid arteries, external carotid arteries, internal carotid arteries bifurcation and extracranial segment of internal carotid arteries (including initial, proximal and distal segments), extracranial segment of VAs and subclavian arteries. The criteria for stenosed arteries mainly depend on the peak systolic flow velocity (PSV) which was specially defined as follows [11-13]: ≥140 cm/s for the MCA, ≥120 cm/s for the ACA, ≥100 cm/s for the PCA and vertebrobasilar artery, and ≥120 cm/s for the siphon internal carotid artery and extracranial carotid artery.
Statistics
Statistical data analysis was performed with SPSS version 17.0 software (SPSS, IBM, West Grove, PA, USA). The χ2 tests were used for discrete variables and the student-t tests for contiguous variables. The logistic regression was done for the relationship for MES and the mentioned risk factors. For all statistical tests, P < 0.05 was considered significant.
Results
Baseline demographics
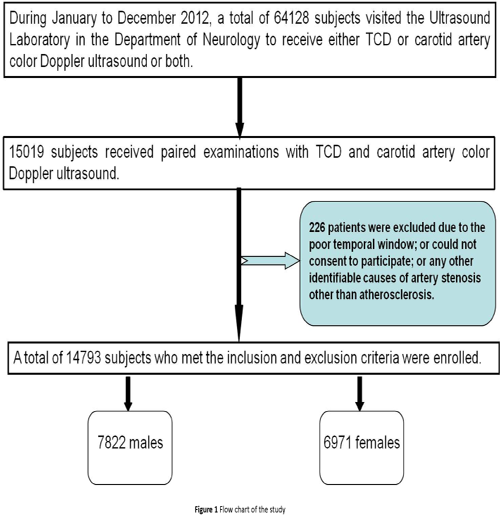
During January to December 2012, a total of 64128 subjects visited our ultrasound laboratory, among whom 15019 received paired examinations with TCD and carotid duplex ultrasound. A total of 226 subjects were excluded because of the poor temporal window, disturbance of consciousness, and any other identifiable causes of artery stenosis other than atherosclerosis. Finally, 14793 subjects, including 7822 males and 6971 females, who met our inclusion were enrolled for data analysis (Figure 1). The median age of the enrolled subjects was 58.5 years old. The distribution of the common vascular risk factors, including hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease, and history of smoking were recorded and analyzed for all the enrolled subjects, was shown in Figure 2.
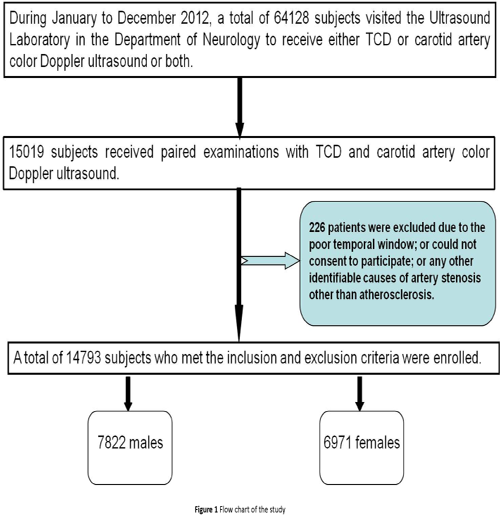
Figure 1: Flow chart of the study.
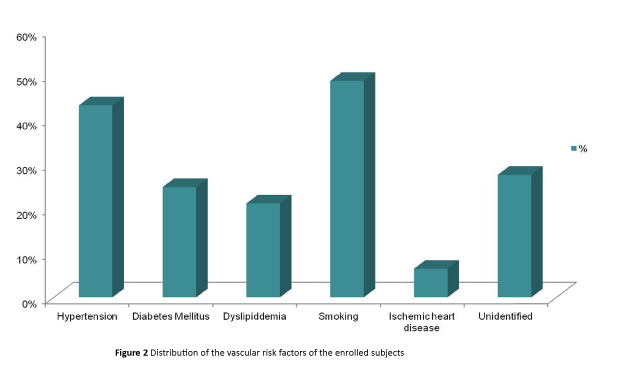
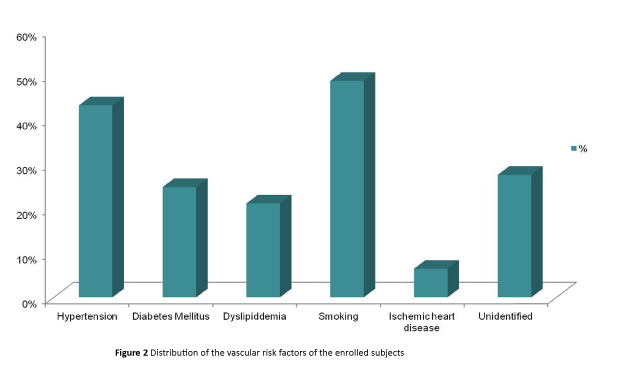
Figure 2: Distribution of the vascular risk factors of the enrolled subjects.
Intracranial artery stenosis was more prevalent than extracranial artery stenosis
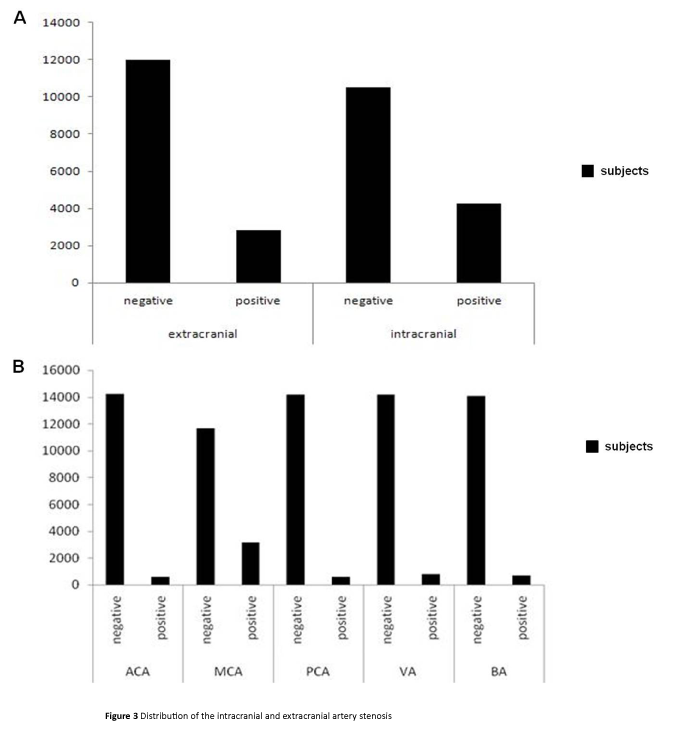
If stenosis was found in one of the intracranial or extracranial arteries regardless of any other arteries, the patient fell into the positive group, which could be further divided into mere intracranial artery stenosis group, mere extracranial artery stenosis group, or the group with both involvements of the intracranial and extracranial artery. While the subjects with none intracranial or extracranial artery stenosis fell into the negative group. Among the enrolled 14793 subjects, 5441 subjects (36.8%) were in the positive group. Mere intracranial artery stenosis was identified in 2632 (17.8%) subjects while mere extracranial artery stenosis was found in 1186 (8%) subjects, indicating that the incidence of mere intracranial artery stenosis was higher than that of extracranial artery stenosis (17.8% vs. 8%, P=0<0.05), as shown in Figure 3A. Patients with concurrent artery stenosis were 1623 cases (11%). In addition, we found that 4255 (28.8%) subjects had intracranial artery stenosis regardless of the condition of extracranial arteries. Extracranial artery stenosis was found in 2809 subjects, with a lower incidence of intracranial artery stenosis (19.0% vs. 28.8%, P<0.05), suggesting that intracranial artery stenosis was commonly involved independent of extracranial arteries stenosis. Furthermore, we analyzed the incidence of different intracranial arteries stenosis, including MCA, VA, PCA and ACA, as shown in Figure 3B. The MCA involvement was found in 3145 subjects (21.3%), which was the most common, and followed by VA stenosis which was found in 770 subjects (5.2%). It is noteworthy that the ACA stenosis was only found in 567 subjects (3.8%), with the lowest incidence.
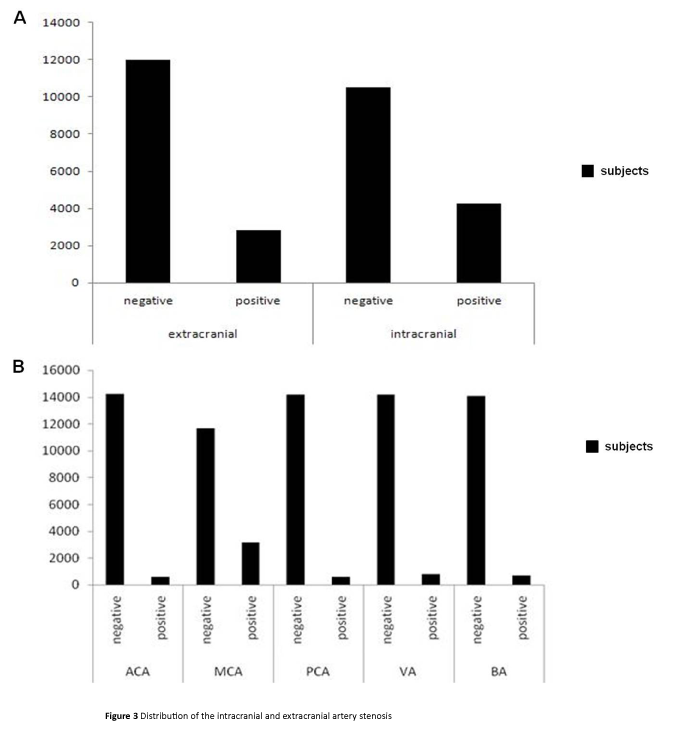
Figure 3: Distribution of the intracranial and extracranial artery stenosis.
Incidence of intracranial artery stenosis was related with elder age
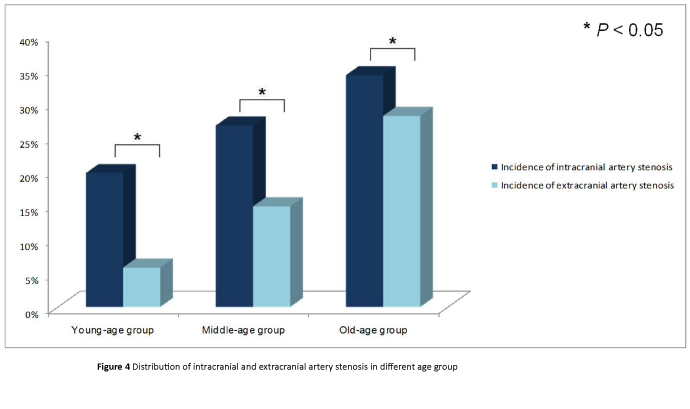
According to the age of the recruited subjects, all the 14793 subjects were divided into the young-age group (≤45 years old), the middle-age group (>45 and ≤60 years old) and the old-age group (>60 years old), which respectively included 2096 (14.2%) subjects, 6589 (44.5%) subjects and 6108 (41.3%) subjects. In the young-age group (≤45 years old), the mean age was 38.5 ± 6.3 years old, and 412 cases were found (19.7%) intracranial artery stenosis while 122 cases (5.8%) with extracranial artery stenosis, implying that the intracranial artery stenosis was more prevalent in this age group (P<0.05). Similarly, in the middle-age group, the median age was 54 ± 4.2 years old, with 1758 cases (26.7%) were intracranial artery stenosis and 972 cases (14.8%) were extracranial artery stenosis, suggesting the difference of the distribution of the intracranial and extracranial artery stenosis (P<0.05). In the old-age group (>60 years old) with the mean age of 69.3 ± 6.2 years old, 2085 cases (34.1%) were found intracranial artery stenosis and 1715 cases (28.1%) were extracranial artery stenosis, as well suggesting the prevalence of the intracranial artery stenosis. The distribution of intracranial and extracranial artery stenosis of each age group was showed in Figure 4. Except for the finding of the prevalence of the intracranial artery stenosis, the incidence of the intracranial and extracranial artery stenosis was increased with age in each group (P<0.05).
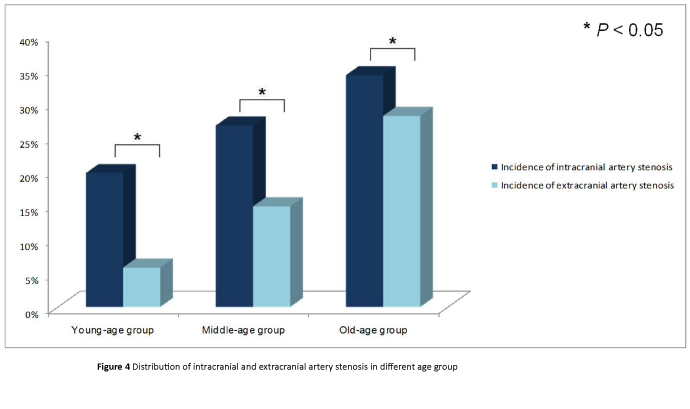
Figure 4: Distribution of intracranial and extracranial artery stenosis in different age group.
Incidence of intracranial artery stenosis was associated with gender
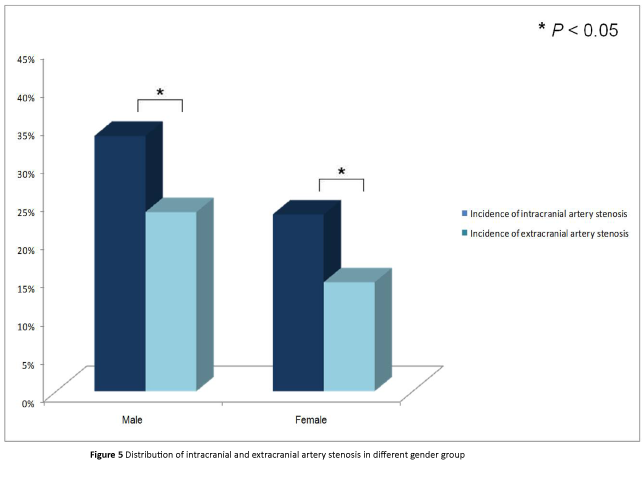
We further took the impact of the gender on the distribution of the intracranial and extracranial artery stenosis into consideration. Among the 14793 subjects, there were 7822 (52.9%) males with the mean age of 57.6 ± 11.9 years old, and 2618 (33.5%) of them were found with intracranial artery stenosis while 1637 (23.5%) were extracranial artery stenosis, suggesting that intracranial artery stenosis was more prevalent (P<0.05), as shown in Figure 5. Similarly, among the 6971 (47.1%) females with the mean age of 57.9 ± 11.5 years old, 1811 (23.2%) were intracranial artery stenosis and 998 (14.3%) were extracranial artery stenosis, as well as indicating that intracranial artery stenosis was more common (P<0.05), as shown in Figure 5. Moreover, both the intracranial and extracranial artery stenosis was more common in male (P<0.05).
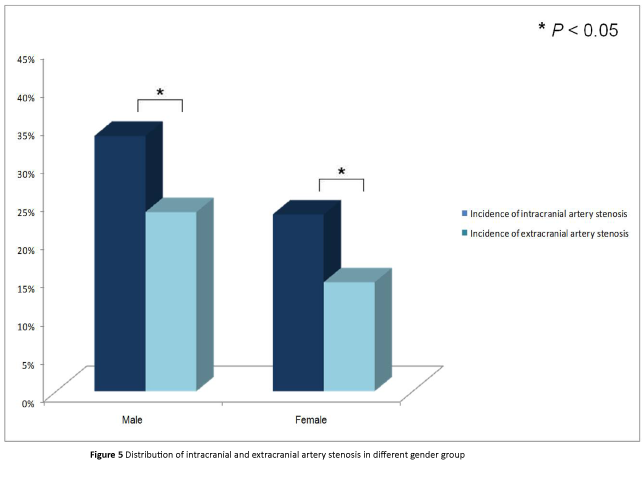
Figure 5: Distribution of intracranial and extracranial artery stenosis in different gender group.
Discussion
Although racial predilection with reference to stenosed artery distribution has been recognized, distribution of intra- and extra-cranial artery stenosis with reference to age and sex has not been clarified. Our ultrasonographic evidence from a northeast Chinese cohort demonstrated that the incidence of cerebral artery stenosis in the population increases with age. The intracranial artery stenosis is more common than extracranial artery stenosis within different age group and the MCA stenosis accounted for the highest proportion among different intracranial artery stenosis. Our results were consistence with previous studies [14]. Fan et al. whose study focused on the 2711 asymptomatic subjects, found that the incidence of mere intracranial artery stenosis, mere extracranial artery stenosis and combined intracranial and extracranial artery stenosis was 3.7%, 1.5% and 0.7%, respectively [15], implying that intracranial artery stenosis was common. However, our results were different from studies from the western countries, suggesting the racial predilection, which had been reported [5-7]. Weimar et al. found that 7.4% of symptomatic subjects in German were found with extracranial internal carotid artery stenosis while that 6.5% were found with intracranial artery stenosis [16]. Another study conducted in America using TCD showed that 39.2% of the total 510 asymptomatic subjects were found with extracranial carotid stenosis, while intracranial artery stenosis was found in 12.9% of the enrolled subjects [17]. Taken together, extracranial artery stenosis suggesting was more common in western countries. The racial difference of distribution of the intracranial and extracranial artery stenosis was speculated to associate with different genetic, diet, and risk factors for susceptibility and many other factors in variety of racial population, among which race is an independent risk factor [6].
In addition, we found that the incidence of different intracranial vascular stenosis, e.g. MCA, PCA, ACA, etc, was different from our study. And MCA stenosis was more likely to involved compared to other intracranial arteries, which was consistence with previous study, such as Chimowitz et al. which found that stenosis rate for internal carotid artery (intracranial segment), MCA, VA, BA was 20.8%, 43.7%, 13.3%, and 22.2%, respectively, among which the MCA was the highest [18]. Another study conducted in TIA subjects from Peking Union medical college hospital found 51% of intracranial artery stenosis or occlusion, 19% of extracranial artery stenosis, 4% of concurrent stenosis of intracranial and extracranial artery, and it is of note that MCA was the most prevalent among the intracranial lesion responsibility artery, accounting for 66% [19]. However, Weimar et al. found that the internal carotid was more common, accounting for 6.5%, than the M1 segment of MCA which accounted for 3.7% [16], which might caused by the racial difference. Taken together, intracranial artery stenosis, especially the MCA stenosis was more common in our cohort.
Moreover, our result showed that intracranial and extracranial artery stenosis was more likely to occur in male compared with female. Dick et al. [20] suggested that gender difference was an important risk factor for asymptomatic severe carotid stenosis and male with asymptomatic severe carotid stenosis had relatively poorer prognosis. de Weerd et al. [21] have made a metaanalysis which found that asymptomatic carotid artery stenosis in different age groups have a relatively high incidence in male compared to female, suggesting the impact of gender on artery stenosis. Our result was consistent with these previous research results, although the intracranial artery stenosis was more prevalent in our cohort. As to why a difference of the incidence of artery stenosis between male and female exists, the difference of specific gene expression, medical treatment, inflammatory markers and hormone levels [22] may be attributable to.
Our findings have significant clinical implications. As per our findings, the incidence of intracranial artery stenosis is higher than that of extracranial artery stenosis. Hence more focus in the screening for cerebral artery stenosis should be given to TCD instead of carotid duplex ultrasound. For those at high risk for cerebral artery stenosis, TCD alongside with carotid duplex ultrasound may serve as a screening tool. That is also the reason why we have such a large sample size for data analysis. Since TCD is cheaper than carotid duplex ultrasound in China (less than 1/2), we empirically utilize TCD in the screening for cerebral artery stenosis so as to lower the burden of our patients.
Furthermore, both the incidence of intracranial and extracranial artery stenosis increased with age, with intracranial artery stenosis was more common than extracranial artery stenosis in different age group. This result was consistent with previous studies as well [23]. de Weerd et al. also suggested that the incidence of asymptomatic carotid artery stenosis may increase with age [21]. Similarly, another study showed that the intima-media thickness (IMT) increased with age in the elderly [24]. In addition, Fan et al reported that age was an independent risk factor for intracranial and extracranial artery stenosis [14]. A probable reason is that artery atherosclerosis gradually increases with age and potential risk factors for vascular stenosis influence arteries much more seriously in high risk groups.
Strengths of our study include the large sample size and excellent professional color artery screening team. Participants received the examination in our single center which may minimize bias due to different inspectors and inspection equipment. However, one limitation of our study was that our analysis was not performed on a representative sample of the population, limiting the generalizability. The results of the present study represent wide applicability for the population of northeast China, but not for all parts of China. Second, though color ultrasound can achieve high accuracy in terms of evaluation of artery stenosis, unified standards are lacking for the evaluation of artery stenosis, thus part inspection result bias in this study is inevitable. In summary, incidence of cerebral artery stenosis in the population increases with age. Intracranial artery stenosis is more common than extracranial artery stenosis and the MCA stenosis accounted for the highest proportion among cerebral artery stenoses, within each age group. More males suffer from intracranial or extracranial artery stenosis than females.
Risk factors including the history of the hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease, smoking were recorded. The incidence of the hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease and smoking in the recruited patients was 43.1%, 24.8%, 21.1%, 6.4% and 48.6%, respectively. Approximately 27.5% of the enrolled patients had no identified risk factors.
The incidence of mere extracranial artery and the mere extracranial artery stenosis of the enrolled subjects, which was 8% and 17.8%. The incidence of intracranial artery stenosis was higher than that of extracranial artery stenosis (17.8% vs. 8%, P<0.05) (Figure 3A). The incidence of different intracranial arteries stenosis, including middle cerebral artery (MCA), vertebral artery (VA), anterior cerebral artery (ACA) and posterior cerebral artery (PCA). The MCA involvement was found in 3145 subjects (21.3%), which was the highest, and followed by VA stenosis which was found in 770 patients (5.2%). While the ACA stenosis was only found in 567 patients (3.8%), with the lowest incidence (Figure 3B).
The enrolled 14793 subjects were divided into the young-age group (≤45 years old), the middle-age group (>45 and ≤60 years old) and the old-age group (>60 years old) according to age. The incidence of the intracranial artery stenosis and extracranial artery stenosis in each age group was respectively 19.7% and 5.8%, 26.7% and 14.8%, 34.1% and 28.1%. More intracranial than extracranial artery stenoses was seen within each age group, and rates of both increased with age (P<0.05).
Among the 14793 subjects, there were 7822 males and 6971 females. The incidence of intracranial artery stenosis and extracranial artery stenosis in each gender group was 33.5% and 23.5%, 23.2% and 14.3%, respectively. Intracranial and/or extracranial artery stenosis was more frequently identified in males than females; moreover, the intracranial artery stenosis in both groups was respectively more common compared to extracranial stenosis.
9350
References
- Primatesta P, Allender S, Ciccarelli P, Doring A, Graff-Iversen S, et al. (2007) Cardiovascular surveys: manual of operations. Eur J Cardiovasc Prev Rehabil 14: S43-S61.
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, et al. (2006) Heart disease and stroke statistics-2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 113: e85-e151.
- Van den Hoogen PC, Feskens EJ, Nagelkerke NJ, Menotti A (2000) The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. N Engl J Med 342: 1-8.
- Bauer C, Sheehan S, Wechsler N, Meyer JS (1962) Arteriographic study of sites, incidence, and treatment of arterosclerotic cerebraovascular lesions. Neurology 12: 698-711.
- Caplan LR, Gorelick PB, Hier DB (1986) Race, sex and occlusive cerebrovascular disease: a review. Stroke 17: 648-655.
- Sacco RL, Kargman DE, Gu Q, Zamanillo MC (1995) Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stoke Study. Stroke 26: 14-20.
- Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, et al. (1996) Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 27: 1974-80.
- You Y, Hao Q, Leung T, Mok V, Chen X, et al. (2010) Detection of the siphon internal carotid artery stenosis: transcranial Doppler versus digital subtraction angiography. J Neuroimaging 20: 234-239.
- Demchuk AM, Demchuk AM, Wein TH, Grotta JC (1999) Yield of transcranial Doppler in acute cerebral ischemia. Stroke 30: 1604-1609.
- Yu D, Zhang W (2007) Assessment of anterior circulation cerebral artery atherosclerosis with combination of carotid color Doppler ultrasonography and transcranial Doppler ultrasonography. Chinese Journal of Contemporary Neurology and Neurosurgery 7: 434-438.
- Wong KS, Li H, Chan YL, Ahuja A, Lam WW, et al. (2000) Use of transcranial Doppler ultrasound to predict outcome in patients with intracranial large-artery occlusive disease. Stroke 31: 2641-2647.
- Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, et al. (2003) Carotid artery stenosis: grayscale and Doppler ultrasound diagnosis--Society of Radiologists in Ultrasound consensus conference. Ultrasound Q 19: 190-198.
- Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, et al. (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339: 1415-1425.
- Fan C, Huang Y (2007) Prevalence of cerebral arterial stenosis in 2711 rural community people aged over 40 years in Beijing. Chinese Journal of Geriatric Heart Brain and Vessel Diseases 9: 36-38.
- Roh YN, Woo SY, Kim N, Kim S, Kim YW, et al. (2011) Prevalence of asymptomatic carotid stenosis in Korea based on health screening population. J Korean Med Sci 26: 1173-1177.
- Weimar C, Goertler M, Harms L, Diener HC (2006) Distribution and outcome of symptomatic stenoses and occlusions in patients with acute cerebral ischemia. Arch Neurol 63: 1287-1291.
- Elmore EM, Mosquera A, Weinberger J (2003) The prevalence of asymptomatic intracranial large-vessel occlusive disease: the role of diabetes. J Neuroimaging 13: 224-227.
- Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, et al. (2011) Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 365: 993-1003.
- Huang YN, Gao S, Li SW, Huang Y, Li JF, et al. (1997) Vascular lesions in Chinese patients with transient ischemic attacks. Neurology 48: 524-525.
- Dick P, Sherif C, Sabeti S, Amiqhi J, Minar E, et al. (2005) Gender differences in outcome of conservatively treated patients with asymptomatic high grade carotid stenosis. Stroke 36: 1178-1183.
- de Weerd M, Greving JP, de Jong AW, Buskens E, Bots ML (2009) Prevalence of asymptomatic carotid artery stenosis according to age and sex: systematic review and metar egression analysis. Stroke 40: 1105-1113.
- Rundek T (2007) Do women have worse outcome after stroke caused by intracranial arterial stenosis? Stroke 38: 2025-2027.
- Rundek T, Arif H, Boden-Albala B, Elkind MS, Paik MC, et al. (2008) Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan Study. Neurology 70: 1200-1207.
- Tamura H, Suzue T, Jitsunari F, Hirao T (2011) Evaluation of carotid arterial intima-media thickness (IMT) and its relation to clinical parameters in Japanese children. Acta Med Okayama 65: 21-25.