Introduction
HIV Infection is a serious public health problem in developing countries. In 2001, it was estimated that 33.2 million of people were living with HIV infection, with developing countries being the most affected (nearly more than 90% of cases). In addition, new contaminations appear with high frequencies and most particularly the infection is taking a feminine face in the developing world (UNAIDS, 2007) [1].
In Africa, countries in the west and those in the North present low HIV infection prevalences in pregnant women; while those in the Southern, Eastern and Central Africa present high prevalences reaching nearly 40% in some countries. In many Sub-Saharan African countries, HIV epidemic is at a generalized level (UNAIDS, 2004) [2].
In Democratic Republic of Congo (DR Congo), permanent HIV surveillance data indicate that the national HIV prevalence in pregnant women is 4.6%; however, there are differences among provinces (D.R. Congo Multi-sectorial National HIV/ AIDS Program, 2006) [3]. The DRC’s 2006 HIV infection serosurveillance report revealed 5.4% of prevalence in the Katanga Province where Lubumbashi, our study site, is located. The national prevalence of over 5% indubitably sets the DRC in the context of countries with generalized HIV infection epidemic.
Previous works have shown that, in the absence of any intervention, the risk of mother-to-child transmission (MTCT) of HIV infection is 40%; and MTCT may occur during the pregnancy (10-15%), at childbirth (10-15%), in post-partum or during breastfeeding (15-20%) (D.R. Congo National Reproduction Health Program, 2004) [4]. This fact suggests that interventions aimed at reducing the risk of transmission of HIV infection from HIV-infected mother to her child can be successful when targeting those different stages. Polytherapy with the use of two or more antiretroviral molecules is reported to be associated with a significant vertical reduction of HIV infection transmission rate than monotherapy [5].
Lately, epidemiologic reports have shown that the rate of MTCT has significantly gone down in countries where interventions designed to reduce the risk have been implemented. Moreover, rates less than 2% of MTCT have been observed when prophylactic antiretroviral treatment has been implemented during pregnancy, childbirth and neonatal periods with exclusion of breast-feeding. Even when breastfeeding exclusion and cesarean are not performed, some studies have revealed that per partum antiretroviral prophylaxis can reduce MTCT to less than 10%. However, the breastfed child’s subsequent possible contamination remains worrying [5].
In DRC, up to December 2001, the National HIV/AIDS Program recommended monotherapy for HIV+ pregnant women that consists of a single dose of Nevirapine in intra partum, and to the child within 12 hours after birth. To our best knowledge, the effectiveness of this practice has not been investigated. In DRC, antiretroviral polytherapy is in use since 2010 (D.R. Congo Ministry of Health, 2006) [3]; but the generalization of this practice has been facing some obstacles such as the accessibility to ART due to the relatively high cost for households with less income.
In Lubumbashi, the anti-HIV/AIDS non-governmental organization ‘Femme SIDA’ and the School of Public Health of university of Lubumbashi have started implementing the ‘prevention of mother-to-child transmission’ of HIV infection (PMTCT) program in September 2004, using a protocol that includes the administration of Nevirapine to mothers before delivery, and the association of Lamivudine- Zidovudine to the infants. The present study evaluated the effectiveness of this program (2004-2009) in terms of MTCT risk reduction in a sample of HIV-positive pregnant women followed at 15 medical settings within Lubumbashi, the second town of the Democratic Republic of the Congo.
Materials and Methods
Study design and participants
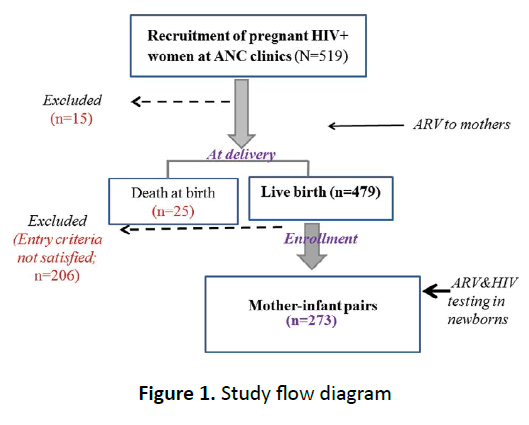
This prospective cohort study was conducted in 15 medical settings where PMTCT activities are implemented, including 4 public referral hospitals (Jason Sendwe, Kapemba, Kisanga and the public health center of Bukama) and 11 privately owned medical settings (Gecamines, Savio, Garengaze, Saint Joseph, Saint Marc, André Barbier, Lwizi, Ave Maria, Bongonga, Hewa Bora and Kyenge). In total, 519 HIV-infected pregnant women were received in antenatal clinics of the above mentioned medical settings from September 2004 through December 2009 (Figure 1).
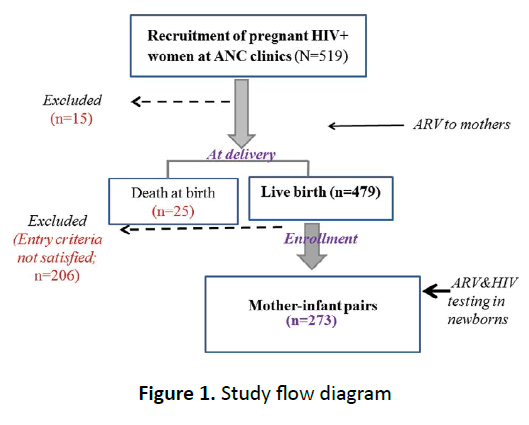
Figure 1. Study flow diagram
Located in the southern province of Katanga, Lubumbashi is the second town of DRC and, with its rich natural resources and mining companies, it is considered as the economic capital of the country. Situated at the proximity of the war-torn Congolese eastern provinces of South and North Kivu, the Katanga province has also been affected the negative impact of the long lasting unrest which has brought gender-based violence that contributes to the rise in the rate of HIV/AIDS [6-8].
Participation in the cohort study was voluntary and only expectant mothers who consented and satisfied the entry criteria were enrolled and administered antiretroviral treatment. Inclusion criteria for the mothers were as follows: being aged 18y. or older, HIV positive pregnant woman, no concurrent antiretroviral medication (ARV) exposure, creatinine < 1.5 mg/dl, serum alanine amino-transferase (ALT) < 2.5 times upper normal limit, hemoglobin equal or higher than 7 g/dl, platelets > 50,000/ ml and absolute neutrophil count (ANC) > 1,000 cells/mm3. Participating mothers indicated breastfeeding after receiving risk-benefit counseling on infants feeding options [9]. Of the 479 expectant mothers who gave live births, only 273 who satisfied entry criteria, underwent both HIV testing and CD4+ cell count, and their infants, entered the cohort (Figure 1).
Antiretroviral prophylaxis
Nevirapine (200 mg) was administered orally to the mother approximately 2 h in intra-partum, and the association of Lamivudine (150 mg) and Zidovudine (300 mg), administered orally and daily to the mother for 5 days in post-partum (one tablet twice a day). The new born received 0.6 ml of Nevirapine administered orally once within 72 hours after birth, and then oral 1.2ml Zidovudine twice a day for 7 days.
Efficacy assessment of PMTCT
Mothers underwent blood sampling twice, and CD4+ cell count was performed before and after childbirth; whereas each child underwent blood sampling after delivery to check for the HIV serological status using Elisa test (Vironostica and Enzygnost).
Ethical consideration and statistical analyses
Informed consent was obtained from each study participant and ethical approval to conduct the study was obtained from the ethics committee of the School of Public Health, University of Lubumbashi. Data are presented as percentages. Wilcoxon test was performed to compare the CD4+ cell count at baseline and after childbirth. All data were analyzed with the use of Epi info version 3.3.2 software. P-values less than 0.05 were considered statistically significant.
Results
Trend of maternal HIV prevalence among all pregnant women who underwent antenatal consultations in 15 study sites in Lubumbashi (2004-2009) The average HIV prevalence rate among all women received at ANC clinics for the 6-year period of the study (2004 – 2009) was 4.6%. The highest HIV rate (7.7%) was observed in the year 2004, whereas the lowest one (2.5%) was noted in 2009 as shown in Figure 2A. When age was taken into account, higher HIV rate (>7%) was found among pregnant women aged 30 – 34 years in 2004 and 2005; however, when considering the period 2006 - 2009, higher rate was noted in pregnant women aged 25 to 34 years (Figure 2B).

Figure 2A. Overall maternal HIV rate among all pregnant women followed in 15 medical settings in Lubumbashi from 2004 through 2009 (N1=34,661) HIV: Human Immunodeficiency Virus, N: Number of all pregnant women followed at the 15 medical settings participating in the study, %: Percentage. The Figure 1a shows that higher prevalence of HIV infection in pregnant women was observed in the year 2004 (7.7%) in medical settings that participated in the study; whereas prevalences of 2- 4% were noted from 2005 to 2009.

Figure 2B. Overall maternal HIV rate among all pregnant women followed in 15 medical settings in Lubumbashi according to age range (N1=34,661)HIV: Human Immunodeficiency Virus, N: Number of all pregnant women followed at the 15 medical settings participating in the study, %: Percentage.
The Figure 2b shows that the group of pregnant women aged 30 - 34 years had the highest HIV prevalence from 2004 to 2007, while the group of those aged 25 – 29 years had highest prevalence in 2008 and 2009.
Demographic profile and characteristics of cohort mothers and their newborns
Of the 519 pregnant women initially recruited; there were 504 who were followed until delivery (15 women lost to follow-up). In all the 15 medical settings participating in the study, there were 479 live births and 25 other newborns died (5.2% of neonatal mortality). From the group of 479 mother-infant pairs, only 273 could be enrolled in the cohort of mother-infant pairs.
Mean age of participating mothers whose newborns were included in the study and underwent HIV testing at 12 months (n=273) was 25 (± 5) years. They were from all counties of Lubumbashi with the majority (> 70%) aged less than 35 y. Most of the mothers were married, 86.4%, and only 13.6% were either single, divorced of widowers; all mothers were Christians. There were 4.8% illiterate (with no education at all); 33.3% had primary education level and 61.9% had high school education level or higher, as shown in Table 1.
| |
Characteristics |
N=273 |
% |
| Age (y.) |
< 20
20-24
25-29
30-34
35-39
40-44
45 or more |
28
51
76
51
28
23
16 |
10.3
18.7
27.8
18.7
10.3
8.4
5.9 |
| Marital status |
Maried(monogamic)
Married (polygamic)
Single |
213
23
37 |
78.0
8.4
13.6 |
| Education level |
None
Elementary
High school
College/university |
13
91
150
19 |
4.8
33.3
54.9
7.0 |
| Occupation |
Office worker
Small business
Tailor
Housewife |
6
78
7
182 |
2.2
28.6
2.6
66.7 |
Table 1. Sociodemographic charateristics of cohort women
Regarding their occupation, 2.6% of the mothers were public servants, whereas 66.7% were either housewives or were running small businesses at home. Obstetrical history showed a median gestity and parity of 6 (gestity range: 1-12) and 5 (parity range: 1-8), respectively (Table 2). Of the newborns tested for HIV (n=273), only 3.7% were born through caesarian delivery; there were 52.7% males and 47.3% females for a sex ratio of 1:1. Mean weight at birth was 2,950 g (± 620) and the rate of low birthweight (LBW) was 12.1%, whereas 3.7% of the neonates had a high birthweight (HBW, ≥4000 g) (not shown).
| Obstetrical parameters |
Median (min.& max.) |
| Gestity |
6 (1-12) |
| Parity |
5 (1-8) |
| Children living in samehousehold |
4 (1-8) |
| Childrenaged 0-12 y. |
3 (0-6) |
| Childrenagedlessthan5y. |
2 (0-3)) |
| Idealnumber of children |
6 (2-12) |
Min : minimum; max : maximum
Table 2. Obstetrical history of cohort women
Effectiveness of PMTCT program in Lubumbashi: rate of mother-to-child transmission (MTCT) of HIV infection and CD4+ count status in cohort mothers
Results of the HIV serological test showed that 24 of 273 (8.8%) children born from HIV positive mothers were HIV positive at birth. On the other hand, CD4+ cell count is considered as an important biological parameter that reflects health status and effectiveness of antiviral treatment in HIV infected patients. Our study showed a 47% increase of CD4 cell count after delivery, when compared with the baseline status (mean: 280 at baseline and 411 after delivery) (Table 3).
| Time-point of theassay |
Nc |
CD4+ count;Mean (SD) |
P-value |
| Baseline |
273 |
280 (28 – 1,202) |
- |
| Afterdelivery |
273 |
411 (43 – 2,321) |
< 0.00001 |
Nc: number of mothersincluded in the cohort.
Table 3. Mothers’ immunological status (CD4+ count) at baseline and after delivery
Discussion
The Figure 2b shows that the group of pregnant women aged 30 - 34 years had the highest HIV prevalence from 2004 to 2007, while the group of those aged 25 – 29 years had highest prevalence in 2008 and 2009.
The present study evaluated the effectiveness of antiretroviral prophylaxis for MTCT in a sample of 273 mother-infant pairs (mothers being HIV+) in 15 medical settings located in Lubumbashi, province of Katanga, Democratic Republic of the Congo. In this study, 24 out of 273 newborns (8.8%) were tested positive at birth, suggesting that the PMTCT protocol used could help reduce the rate of HIV transmission at birth when compared with the national level (15-20%). Similar results have been reported previously in studies by Moodley and colleagues [10], with a transmission rate of 9.3%. In addition, when antiretroviral prophylaxis was combined with replacement feeding, relatively low transmission rates, 8.3% in the US and France [11] and 9.4% in Thailand [12]. Another study conducted in South African hospitals, in which a simple dose of Nevirapine was administered to newborns 72h after delivery, showed transmission rates varying from 8.6 to 13.7% [11]. Furthermore, lower transmission rates have been found with the association Zidovudine-Lamivudine administered to infected mothers at 36 weeks of gestational age and within seven days following childbirth [12].
PMTCT implementation in an area where HIV stigmatization is still high, like in D.R. Congo, faces many challenges. The success of this preventive method depends not only on the acceptance of the situation by infected women, but also the support of their spouses. This would help women to comply with the protocol utilized [13]. Moreover, implementation of short regime PMTCT protocols is beneficial and is thought to be well adapted to developing countries [14].
The question related to breastfeeding by HIV-infected women remains a serious issue. In the environment where our study was conducted, as well in other areas of the country, adherence to breastfeeding exclusion is not a common practice. And this reality can be attributed, at least partially, to husbands’ opposition in one side and the low average literacy rate of women in the other. Public health programs aimed at preventing HIV transmission from mother to her child ultimately aim at protecting the lives of children born from HIV+ mothers and the success of such programs should be evaluated in the context of poor settings in developing countries. In developing countries, among the main causes of death in children under 5 years of age, there are diarrheal diseases mostly due to poor hygiene and malnutrition [5,15].
Thus, bottle-feeding raises a question in connection with its applicability as it is known that it exposes the child to the risk. Even if bottle-feeding could be correctly performed by mothers, there is a subsidiary question related to how the infection is accepted in people’s lives in the context of high illiteracy rate. It is about the difficulty to convince some mothers or families in regard to breastfeeding avoidance. This preventive measure might be easy to adopt if the infection is positively accepted by spouses and HIV is considered as a family threat [15].
Meanwhile, in our environment in Africa, sex specific considerations lead to the fact that the burden of the infection is mostly on the woman; and the majority of women followedup in our PMTCT program live quite secretly, without their male partners’ involvement in the program. This attitude in the family makes the women avoid any suspicious behavior such as avoidance of breastfeeding. In such a situation, they may refuse to comply with the recommendations from the medical staff. Arendt and colleagues have found that a combination of a tritherapy and breast-feeding might be a safe way of preventing the transmission of HIV infection to children born from infected mothers, while keeping the breast-feeding advantages and avoiding stigmatization and bottle-feeding risk [16].
The present study has some limitations. First, avoidance of breastfeeding is often practiced in most PMTCT programs, especially in developed countries, to efficiently reduce the rate of MTCT. However, considering the reality that infected mothers have difficulty to comply with breastfeeding avoidance in the context of poverty and limited nutritional resources due to low average income of most households, antiretroviral therapy was the only intervention implemented in the present study. Nevertheless, our protocol showed a reduced rate of MTCT, when compared with the national rate for breastfed children born from HIV+ mothers. This represent a real advantage given that MTCT was markedly reduced at time point of pregnancy-delivery-breastfeeding continuum with a simultaneous improvement of CD4+ count. In addition, the fact that such a program is implemented mostly in poor medical settings and provide evident benefice in terms of reduction of MTCT is encouraging. Future study should extend the follow-up period in order to find out the real impact of breastfeeding on newborns’ serological status.
Second, in this study, there was in control group to could be compared to that of infected mothers who underwent the PMTCT program implemented in Lubumbashi. In DRC, PMTCT is a routine practice and infected mothers are aware of it. Having a control group of HIV infected mothers not subjected to any PMTCT regiment is viewed as unethical in our environment, whereas making a control group with another treatment protocol was not envisaged in our study design. Instead, the present study was designed to determine the beneficial effects of PMTCT program implemented in Lubumbashi in terms of reducing MTCT rate and improving mothers CD4+ count in comparison to the rate in the population of non-treated infected mothers (15-20%). In future studies, we plan to include one or more control groups with different PMTCT regiments. Such a study design might determine a more effective PMTCT regiment and factors associated with the risk of MTCT.
In conclusion, this study, which consisted of a cohort of 273 mother-child pairs followed in Lubumbashi, Democratic Republic of the Congo, showed that PMTCT program markedly reduced the risk of HIV transmission and improved the immunological status of mothers. This suggests that the PMTCT program implemented in Lubumbashi could be a useful public health intervention if extended in the region. However, subsidiary questions should be addressed, such as HIV infection stigmatization, non-involvement of fathers in the program.
Acknowledgments
The authors thank the staff of “Direction Générale de Développement of Belgium for provided the funds used in the Mother and Child Health Promotion program implemented in Lubumbashi; we also thank the staff of Universud-Liege for their wonderful support.
6480
References
- Programme National Multisectoriel de Luttecontre le Sida (RD Congo). Rapport national surl’épidémie à VIH 2006.
- Programme National de Santé de la Reproduction (2004): Plan national et plan directeur de développement de la santé de la reproduction 2004.
- Newell, M.L. Prevention of mother-to-child transmission of HIV: challenges for the current decade. Bull World Health Organ 2001; 79: 1138-1144.
- Ngatu, N.R., Kanbara, S. Armed conflict, women’s vulnerability and HIV/AIDS in the great lake region of Africa: Reinforcing human security to prevent widespread of the pandemic. Clin Res HIV/AIDS. 2013; 1(1):1003.
- Mukwege, D.M., Nangini, C. Rape with extreme violence: the new pathology in South Kivu, Democratic Republic of Congo. PLoS Med 2009; 6: e1000204.
- Casey, S.E., Gallagher, M.C., Makanda, B.R., Meyers, J.L., Vinas, M.C., et al. Care-seeking behavior by survivors of sexual assault in the Democratic Republic of the Congo. Am J Public Health 2011; 101: 1054-1055.
- Thomas, T.K., Masaba, R., Borkowf, C.B., Ndivo, R., Zeh, C., et al. Triple-antiretroviral prophylaxis to prevent mother-to-child HIV transmission through breastfeeding--the Kisumu Breastfeeding Study, Kenya: a clinical trial. PLoS Med 2011; 8: e1001015.
- Moodley, D., Moodley, J., Coovadia, H., Gray, G., McIntyre, J et al. A multicenter randomized controlled trial of nevirapine versus a combination of zidovudine and lamivudine to reduce intrapartum and early postpartum mother-to-child transmission of human immunodeficiency virus type 1. J Infect Dis. 2003; 187(5): 725-735.
- Connor, E.M., Sperling, R.S., Gelber, R., Kiselev, P., Scott, G. et al. Reduction of maternal-infant transmission of Human immunodeficiency virus type 1 with zidovudine treatment: Paediatric AIDS Clinical Trials Group Protocol 076 study group. N Engl J Med. 1994 Nov3; 331(18):1173-1180.
- Shaffer, N.., Chuachoowong, R., Mock, P.A., Bhadrakom, C., Siriwasin, W., et al. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: a randomised controlled trial. Bangkok Collaborative Perinatal HIV Transmission Study Group. Lancet 1999; 353: 773-780.
- PETRA Study team. Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra study): a randomised, double-blind, placebo-controlled trial. Lancet. 2002;359(9313):1178-86.
- Thairu, L.N., Pelto, G.H., Rollins, N.C., Bland, R.M., Ntshangase, N. Socio-cultural influences on infant feeding decisions among HIV-infected women in rural Kwazulu Natal, South Africa. Matern Child Nutr.2005; 1(1): 2-10.
- Seidel, G., Sewpaul, V., Dano, B. Experiences of breastfeeding and vulnerability among a group of HIV-positive women in Durban, South Africa. Health Policy Plan 2000; 15: 24-33.
- Arendt, V., Ndimubanzi, P., Vyankandondera, J., Ndatisaba, G., Muganda, J et al. Effectiveness of antiretroviral therapy in breastfeeding mother to prevent post-natal vertical transmission in Rwanda, 4th IAS conference on HIV: Pathogenesis treatment and prevention incorporating the 19th ASHM conference.