Objective: Vertebral compression fractures (VCF) cause significant disability and
pain and are usually treated by vertebroplasty using polymethylmethacrylate
(PMMA), which has several drawbacks, including fractures and exothermic neural
damage associated to lea-kage. VK100 silicone is a new polymer for vertebroplasty
to resolve these disadvantages.
Material and Methods: This study follows the evolution of seventy patients with
VCF who received a VK100 elastoplasty. The period of follow up was a year average.
Results: Four patients had asymptomatic silicone leakage, none had neural
damage and, at the end of follow up, there had been no adjacent fractures.
Patients reported less pain.
Conclusion: We conclude VK100 is a good option for vertebroplasty to treat
osteoporotic spinal compression fractures.
Introduction
Vertebral body fractures are the most common osteoporosisassociated fractures causing deformity, pain and disability. A compression fracture of the osteoporotic spine is a strong indication for vertebroplasty and the most widely used material is polymethylmetacrylate (PMMA) however there are drawbacks to PMMA. First, it creates an exothermic reaction during polymerization that can induce neural damage. Second, it is not absorbed by the osseous trabeculae. Third, PMMA cement is stiffer than bone, possibly increasing torque forces on adjacent vertebral levels and contributing to fractures in these levels. In this study we evaluate a new filling substance, VK100, an elastic polysiloxane polymer (silicone) used for vertebral augmentation. VK100 is designed to be less rigid than PMMA and it is hypothesized that it will reduce the rate/ frequency/ likelihood of adjacent fractures.
Materials and Methods
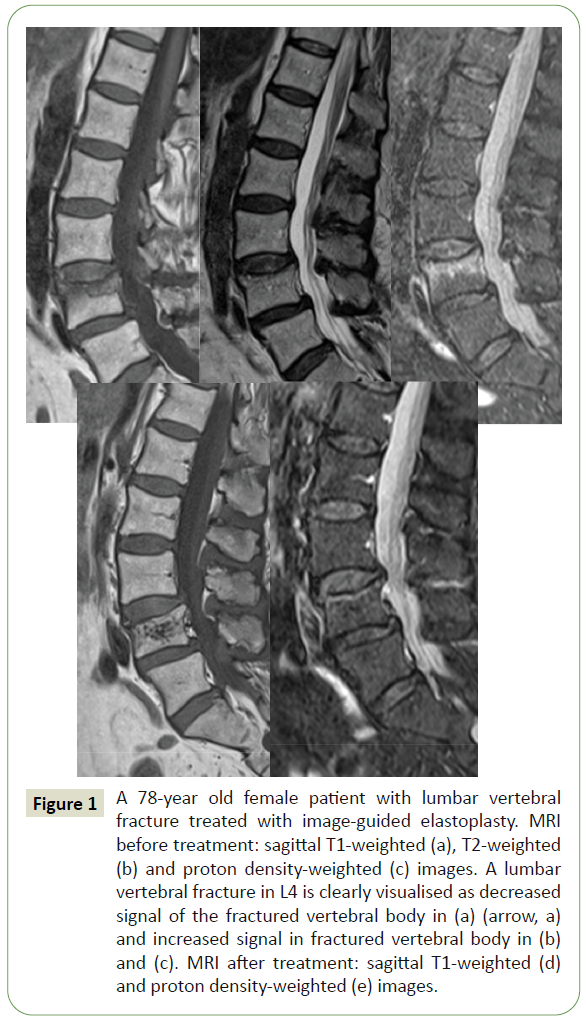
Seventy patients (10 men, 60 women, and mean age 78 years, range 60-90 years) with vertebral compression fractures who were treated with elastoplasty using VK100 are reviewed. The mean follow up period was 1 year average (range 12-24 months) The VCF were osteoporotic in all patients. The total number of treated vertebral bodies was 80. There were 8 VCF in D8, 4 in D9, 4 in D10, 4 in D11, 20 in D12, 20 in L1, 8 in L2, 4 in L3 and L8 in L4. There were 16 patients aged between 60 and 70 years, 28 between 70 and 80 years and 26 were over 80 years old (Figure 1).
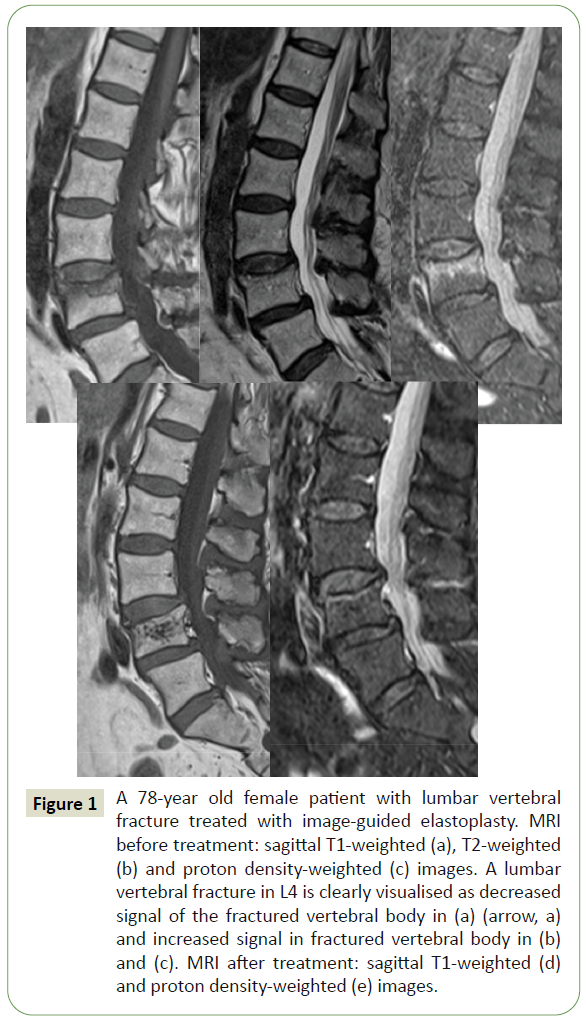
Figure 1: A 78-year old female patient with lumbar vertebral fracture treated with image-guided elastoplasty. MRI before treatment: sagittal T1-weighted (a), T2-weighted (b) and proton density-weighted (c) images. A lumbar vertebral fracture in L4 is clearly visualised as decreased signal of the fractured vertebral body in (a) (arrow, a) and increased signal in fractured vertebral body in (b) and (c). MRI after treatment: sagittal T1-weighted (d) and proton density-weighted (e) images.
The procedure was performed under general anesthesia in all cases. The mean duration of surgery was 15 minutes. We always used a bilateral transpedicular approach. The surgical indication was a VCF between D8 and L4 after a trauma, and a clinical onset of less than 6 months earlier confirmed by X-rays and edema on MRI.
Surgical Technique
Elastoplasty was performed under general anesthesia in prone position and with the help of fluoroscopy. We used a 10 gauge verebroplasty needle with a bilateral transpedicular approach. The amount of VK100 injected varied between 2 to 8 mL (the mean volume of filling in each vertebra was 4 mL) until satisfactory filling was achieved or leakage outside the vertebral body was observed on fluoroscopy. The setting time for VK100 is about 10 minutes from the beginning of the procedure. Patients were discharged 24 hours after surgery.
Results
The procedures were technically successful in all patients, as defined by effective transpedicular puncture of the vertebral body with instillation of VK100. Cement leakage was observed inside paravertebral soft tissue in 6 patients. There were no intraor postoperative neurological or pulmonary complications. Back pain improvement was used as the outcome measure. Mean visual analog scale (VAS) improved from 8 (5-9) to 2.4 (1-5) at discharge and had not changed at 3 months or 1 year of follow up.
The mean Oswesty index improved from 70% (52-91%) to 23% (8-42%) at the 3 months follow up with no significant change at the 12 month exam 21% (8-45%).
We observed silicone leakage in 4 patients. Leakage was seen in the paravertebral venous plexus in 2 cases, in the disc space in 1 case and in the spinal canal in the last case. All of the leakages were asymptomatic. No adjacent vertebral body fractures have been observed in any patient since the procedure to the present time.
Discussion
Percutaneuous vertebroplasty with PMMA has been regarded as an effective management option for vertebral compression fractures but has disadvantages: exothermic reaction >60º during polymerization could be dangerous if cement leaks outside vertebra; short working time, rapid solification, absence of ostoconduction and PMMS is not biodegradable and hard to remove if extrusion of the cement causes neurologic complications or during revision surgeries.
Adjacent level vertebral fractures are also a potential complication, since vertebrae treated with PMMA are stiffer than fractured ones, they may transmit increased forced to adjacent levels and bone absorption have been observed at the interface with PMMA. The incidence of post percutaneous vertebroplasty vertebral fracture is reported to vary from 12% to 52% [1-4] Fahim postulated that the end plate deflection fracture mechanism was the main cause of new fractures after vertebroplasty [5].
Elastoplasty performed with VK100 is a new alternative technique based on vertebroplasty. VK100 is an injectable silicone (Dimethyl methylvinyl siloxane and Dimethyl Methylhidrogen siloxane, with Barium sulfate 15% to provide radio-opacity) which could be an alternative for vertebral augmentation. VK100 has various advantages: its components do not develop exoteric reactions (even in case of leakage inside the spinal canal, the potential of neurological damage is low); the product is less rigid than PMMA and biomechanics studies indicated that fractured vertebrae filled with VK100 show a lower stiffness in comparison to PMMA [6-8]; a further advantage of VK100, which is its elasticity and reduced stiffness, is the possibility of introducing metallic materials such as pedicle screws or biopsy trocars inside it. Latter instrumentation of the augmented vertebra and biopsy for recurrences occurred anterior to the augmentation are viable with this feature.
In their systematic review of 69 clinical studies, Hulme et al. have found the mean VAS score to decrease from 8,2 to 3,0 and found out that 87% of the patients have had pain relief after vertebroplasty of kyphoplasty [9,10] Bornemmann et al. reported that, with elastoplasty, the reduction of VAS or ODI is comparable or slightly better than with the use of PMMA cement (8) In our series of 70 patients, the mean VAS score decreased from 8 to 2.4 VAS score dreaded in all patients postoperatively. Regarding pain relief, elastoplasty seems to be comparable with Vertebroplasty.
The risk of cement leakage in various series of vertebroplasty or kyphoplasty ranges between 3% and 80% with resultant neurological deficits such as radiculopathy and cord compression occurring in 0% to 3.7% and 0% to 0.5% respectively [10].
Silicone pulmonary embolism (SPE) is a serious complication of elastoplasty. Urlings and van Der Linden has performed chest computerized tomography in the early postoperative period in 10 of the 12 patients in whom the performed elastoplaty. They have detected SPE in 60% [11]. Due to the low viscosity, Gasbarrini et al. supposes that SPE may occur during elastoplasty via perivertebral venous plexus. However, with the presence of no symptomatic cases, their study show that SPE is not a clinical event similar with cement pulmonary embolism (CPE) in our study, we did not have silicone pulmonary embolisms (SPE) in 70 patients.
The main limitations of the present study are is retrospective design and the absence of a control group. The influence of the biomechanical properties of silicone on long term reduction of adjacent level features requires further analyses.
Conclusion
Elastoplasty with VK100 is a good procedure that can avoid the drawbacks of PMMA for augmentation of fractured vertebral bodies. This report shows that elastoplasty is as good as PMMA in terms of pain relief and leakage incidents, and does not present the drawbacks of the latter material (neural damage, increased fracture rate). Whether the biomechanics properties of VK100 actually influence biomechanics load distribution and the long term adjacent lever fracture rate in patients treated for vertebral fracture needs confirmation in further studies with longer follow ups and larger patient numbers.
38742
References
- Eichler MK, Göktas V, Hölper BM, Joechel P (2013) Clinical evaluation of elastoplasty, a percutaneous augmentation of vertebral compression fractures with an elastic silicon-based polymer. J Spine Surg 1: 80-85
- Yang H, Zou J (2011) Filling materials used in kyphoplasty and vertebroplasty for vertebral compression fracture: A literature review. Artif Cells Blood Substit Immobil Biotechnol 39: 87-91
- Togawa D, Bauer TW, Liebermann IH, Takikawa S (2003) Histologic evaluation of human vertebral bodies after vertebral augmentation with polymethylmethacrylate. Spine 28: 1521-1527.
- Fribourg D, Tang C, Sra P, Delamarter R, Bae H (2004) Incidence of subsequent vertebral fracture after kyphoplasty. Spine 29: 2270-2276.
- Fahim DK, Sun K, Tawackoli W, Mendel E, Rhines DL, Burton AW, et al. (2011) Premature adjacent vertebral fracture after vertebroplasty: A biomechanics study. Neurosurgery 69: 733-744.
- Lee MJ, Dumonsky M, Cahill P, Stanley T, Park D, Singh K (2009) Percutaneous treatment of vertebral compression fractures: A meta-analysis of complications. Spine 34: 1228-1232.
- Schulte TL, Leider A, Riechelmann F (2013) Biomechanical compraison of vertebral augmentation weht silicone and PMMA cement and two filling grades. Our Spine J 22: 2695-2701.
- Bornemann R, Rommelspacher Y, Jansen TR, Lange T, Schmoelez W (2016) Elastoplasty: A Silicon Polymer as a New Filling Material for Kyphoplasty in Comparison to PMMA. Pain Physician 19: E885-E892.
- Kim JM, Shin DA, Byun DH, Kim HS, Kim S, et al. (2012) Effect of bone cement volume and stiffness on occurrences of adjacent vertebral fractures after vertebroplasty. J Korean Neurosurg Soc 52: 435e440.
- Gasbarrini A, Ghermandi R, Akman YE, Girolami M, Boriani S (2017) Elastoplasty as a promising novel technique: Vertebral augmentation with an elastic silicone-based polymer. Acta Orthop Traumatol Turc 59: 209-214
- Urlings TA, Vander Linden E (2013) Elastoplasty: First experience in 12 patients. Cardiovasc Interv Radiol 36: 479-483.